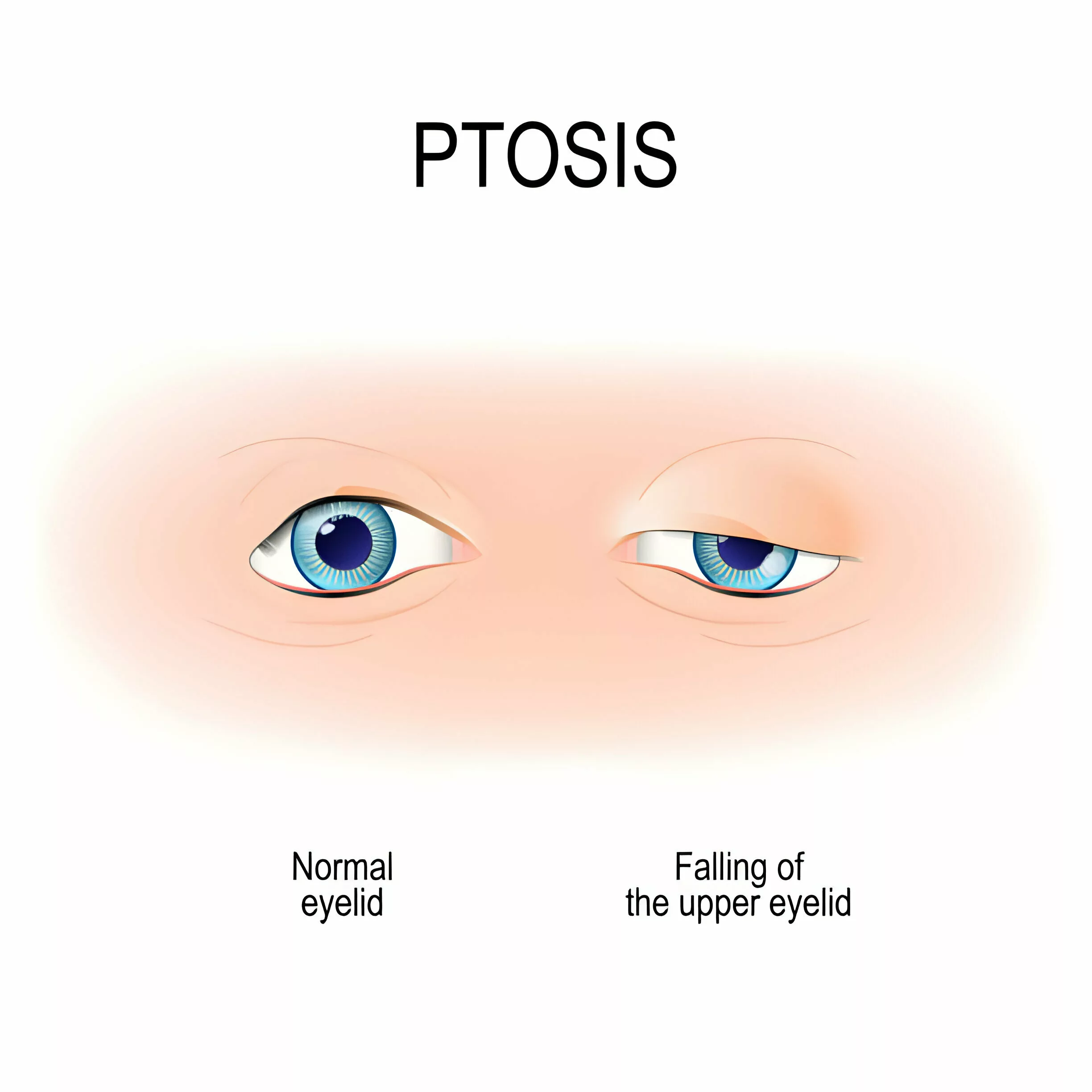
What is Ptosis?
Ptosis or Blepharoptosis is a condition in which the upper eyelid drops over the eye, limiting normal vision. It can present from birth or occur later in life. In some cases, it is associated with any underlying disease.
Pathophysiology
Your eyelid has two important muscles: The levator palpebrae superioris and the Muller’s muscle, and they help elevate your eyelid when you look up. The oculomotor nerve (third cranial nerve) supplies your levator palpebrae superioris, the primary muscle for upward movement of your eyelid. Along with its sheet of fibrous tissue, the levator muscle makes the crease of your upper eyelid. The sympathetic nerve supplies your Muller’s muscle, which originates below the levator palpebrae superioris. Any factor that interferes with the nerve supply of muscles causes ptosis. You can also get ptosis by any trauma or by increasing age.1McInnes, C. W., & Lee-Wing, M. (2015). Eyelid ptosis. CMAJ : Canadian Medical Association journal = journal de l’Association medicale canadienne, 187(14), 1074. https://doi.org/10.1503/cmaj.140579
Causes of Ptosis
It is either congenital or acquired, and ptosis has many causes.2Finsterer J. (2003). Ptosis: causes, presentation, and management. Aesthetic plastic surgery, 27(3), 193–204. https://doi.org/10.1007/s00266-003-0127-5Based on causes, it is divided into the following types:
Myogenic Ptosis:
It occurs when there is a defect in the muscles of your eyes that helps in upward movement, especially levator palpebrae superioris.
Conditions in which muscles of your eyes become defective are:
Myasthenia Gravis
In Myasthenia gravis, your immune system makes antibodies against the acetylcholine receptor. This causes weakness in the voluntary muscles of your eyes, arms, and legs. It is the most common symptom of ocular myasthenia gravis.
Oculopharyngeal Dystrophy
It is a genetic disease that affects the eyes and throat muscles. When the muscles of the eyes are involved, it causes ptosis. This disease also causes weakness in the facial muscles.
Myotonic Dystrophy
It is also a genetic disease that affects the muscles of the face, eyes, and gastrointestinal tract. There are two types, and chromosomes 9 and 13 become defective.
Chronic Progressive External Ophthalmoplegia
CPEO occurs when there is a defect in your nuclear or mitochondrial DNA, but mostly in mitochondrial DNA. This disease leads to drooping in both eyes and limited eye movement.
Mechanical Ptosis:
This occurs when you have an abnormal external mass that affects the function of your eye muscles or causes your eyelids to drop. These masses may include:
- Neoplasm (tumor)
- Chalazion (a small bump in your eyelid)
- Neurofibroma (a tumor in your nerves)
- Hemangioma (tumor of blood vessel, appears as a red lump on your skin)
- Scarring
Neurogenic Ptosis:
Neurogenic means that any congenital or acquired factor affects the nerve supply of your eye muscles.
Congenital neurogenic ptosis occurs in the genetic third nerve palsy and congenital Horner syndrome. In third nerve palsy, you have a small pupil and mild ptosis. In congenital Horner syndrome, you may experience:
- Ptosis (drooping of your upper eyelid)
- Anhidrosis (loss of sweating)
- A small or constricted pupil
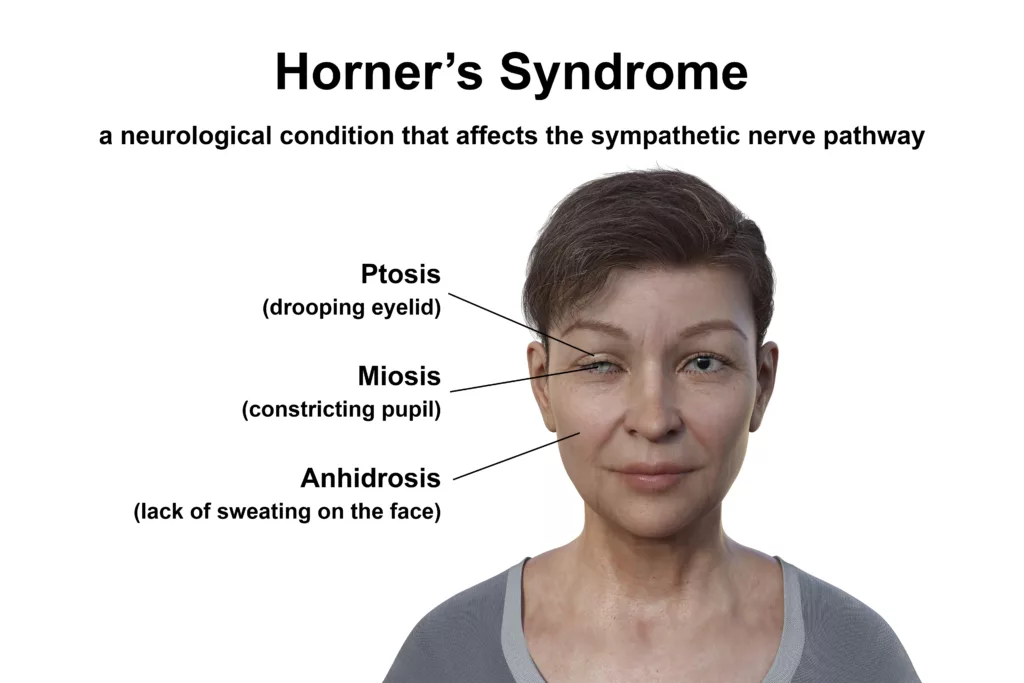
If you acquire neurogenic ptosis in adult life, it is due to myasthenia gravis, acquired third nerve palsy, or acquired Horner syndrome. Neoplasms, trauma, infections, and multiple sclerosis can cause palsy of your third cranial nerve and Horner syndrome.
Traumatic Ptosis:
Drooping eyelids can result from any direct or indirect trauma to the eye. This includes injury to the eye during eye surgery and orbital floor fractures caused by a direct blow to the eye.
Aponeurotic Ptosis:
It is the most common cause of adult ptosis, also known as involutional ptosis. Aponeurotic ptosis can result from any trauma, increasing age, or injury to the eye during surgery.
Pseudoptosis:
What are the Symptoms associated with Ptosis?
You may experience some associated symptoms along with drooping of your eyelid. These are:
- Increase production of tears
- Reduced vision in your affected eye
- Itching in your affected eye
- Tiredness in the eye due to lagging of the upper eyelid
- Backward tilt of your head ( to see clearly through the affected eye )
How to diagnose Ptosis?
Your doctor diagnoses this condition by taking your proper history and performing a complete examination of your eyes.
The following points are important for the diagnosis:
History:
Your doctor can quickly diagnose it by the physical appearance of your eye. You should give a comprehensive and detailed history of your symptoms before going for an eye examination:
Important questions your doctor may ask you are:
- When was the onset of ptosis?
- What is the duration of your symptoms?
- Any family history of ptosis?
- Any history of trauma to the eye?
- Any history of eye or brain surgery?
- What are the associated symptoms?
Examination:
Your doctor observes the following things to make a diagnosis:
Both Eyes, along with your Forehead
Examination of both eyes is necessary because it helps your doctor diagnose the cause of ptosis. This condition, caused by any trauma, mainly affects one of your eyes. However, in most cases of myasthenia gravis, it is present in both of your eyes. Observing the skin of the forehead is also necessary, as it gets wrinkled when you try to see through your droopy eye.
Observation of Eyebrows
You lift your eyebrow when you try to see clearly through the affected eye. Your doctor must check this sign to observe how severe the ptosis is.
Upper Eyelid Crease
The levator muscle forms the upper eyelid crease; in ptosis, this muscle does not function properly. Your doctor must check the absence of this crease to assess the function of the levator muscle.
Presence of any Abnormal Tissue or Scar
Your doctor examines your whole face for abnormal growth or scar tissue. The presence of abnormal tissue may indicate ptosis, either due to trauma or postoperative injury.
Jaw-Winking Sign
This sign is present if you have ptosis due to Marcus Gunn syndrome. To check this sign, your doctor observes your upper eyelid while you chew, smile, or move your jaw to the opposite side. Your upper eyelid moves or winks if you have Marcus Gunn syndrome.4Keene, K. R., Kan, H. E., van der Meeren, S., Verbist, B. M., Tannemaat, M. R., Beenakker, J. M., & Verschuuren, J. J. G. M. (2022). Clinical and imaging clues to the diagnosis and follow-up of ptosis and ophthalmoparesis. Journal of cachexia, sarcopenia, and muscle, 13(6), 2820–2834. https://doi.org/10.1002/jcsm.13089
Tests for Ptosis
Your doctor may do some necessary tests to confirm that you have ptosis.
These are:
Slit-Lamp Examination:
In slit lamp examination, your doctor sees the internal structures of your eyes by putting light into your eyes. It helps diagnose the cause of ptosis, which is either the presence of abnormal tissue or a tumor in your eye.

Visual Field Test:
The visual field test is crucial if your vision deteriorates due to ptosis. This test quickly detects your central and peripheral vision loss.

Ocular Motility Test:
An ocular motility test assesses the function of six extraocular muscles of your eye: four recti and two obliques. These muscles have different actions; your doctor considers them individually to determine the cause of ptosis.
Edrophonium Test:
Your doctor administers 1 mg of edrophonium into your affected eye and waits at least 2-5 times. If the ptosis is due to myasthenia gravis, your upper eyelid elevates. If there is no improvement in the ptosis, this test is negative.5Grace Lee, N., Lin, L. W., Mehta, S., & Freitag, S. K. (2015). Response to phenylephrine testing in upper eyelids with ptosis. Digital journal of ophthalmology: DJO, 21(3), 1–12. https://doi.org/10.5693/djo.01.2015.05.001
Blood Serum Test:
If you have ptosis due to myasthenia gravis, your blood serum test will show antibodies against the acetylcholine receptor.
Ice Pack Test:
Put an ice pack on your affected eye for at least 2 minutes. If the ptosis of your eye improves, the cause of ptosis is myasthenia gravis.
CT Scan or MRI of the Brain:
Tumors in your orbit and skill or any trauma to the brain can cause ptosis. Your ophthalmologist may advise you to get a CT scan or MRI of the brain to identify the cause.6Buechner, S., & Capone, L. (2021). Ice Pack Test Eased Ptosis in a Patient Presenting with a Possible Oculomotor Nerve Schwannoma: A Case Report. Neurology International, 13(4), 510–516. https://doi.org/10.3390/neurolint13040050
Critical Measurements to Take to Diagnose Ptosis
Your ophthalmologist may take some critical measurements of your eye because they help make the complete diagnosis of ptosis.
These are:
Marginal Reflex Distance Test:
Your doctor measures your eye’s marginal reflex distance by putting light directly into your eye and measuring the distance between the light reflex in your pupil and your upper eyelid margin. This test is important to determine the degree of ptosis.7Ural O, Mocan MC, Dolgun A, Erdener U. The utility of margin-reflex distance in determining the type of surgical intervention for congenital blepharoptosis. Indian J Ophthalmol. 2016 Oct;64(10):752-755. doi: 10.4103/0301-4738.195016. PMID: 27905338; PMCID: PMC5168917.
Levator Muscle Function:
Measuring the levator muscle function helps doctors decide which procedure is appropriate for your eye. Your doctor puts his thumb on your eyebrow while you look downwards and asks you to look upward. Then, a scale measures this activity. A measurement of 9-15mm is considered normal, and if you have a measurement of less than 4mm, it means the function of your muscle is poor.
Palpebral Fissure Height:
Palpebral fissure height is the distance of the cornea from the upper and lower lid margins. Usually, the upper and lower lid margins cover 2 mm and 1 mm of the cornea, respectively. In ptosis, the upper lid margin covers more than 2 mm of the cornea. Your doctor should examine both eyes to confirm the diagnosis of ptosis.
Margin Crease Distance:
Margin crease distance is the distance between your lid margin and skin crease when you look downward. Its standard value in men is from 7 mm to 8 mm; in women, it is 8-10 mm. This distance is usually absent when you have congenital ptosis, but if you have aponeurotic ptosis, as in aging, MCD increases more than its average value.8Ural, O., Mocan, M. C., Dolgun, A., & Erdener, U. (2016). The utility of margin-reflex distance in determining the type of surgical intervention for congenital blepharoptosis. Indian journal of ophthalmology, 64(10), 752–755. https://doi.org/10.4103/0301-4738.195016
How Is It Treated?
Only surgical procedures can permanently treat it, while medical treatment may treat its associated symptoms.
Medical Treatment:
Symptomatic treatment includes:
Eye Drops
If you have ptosis due to trauma or infection, your doctor may prescribe 0.1% oxymetazoline eye drops. You should use only one drop daily in your affected eye.
Myasthenia gravis (MG) typically responds well to medical therapy, which is the preferred treatment for these patients. Ptosis caused by Horner syndrome may see temporary improvement with topical apraclonidine, naphazoline, or tetrahydrozoline. Although these treatments haven’t been formally studied for ptosis, they can help alleviate symptoms.

Artificial Tears or Cold Compressor
If you feel itching with ptosis, put artificial drops in your affected eye. You can also use a cold compressor on your eye for a few minutes, which helps to relieve your itching temporarily.
Treatment with Special Glasses:
If you want to avoid surgery, your doctor may suggest using glasses specially made for ptosis. These glasses have a crutch on their inner side that lifts your upper lid and helps you see clearly through the ptotic eye.
Surgical Treatment:
The best and most permanent treatment for this condition is surgery. Surgical options that you can choose are:
Resection of the Levator Muscle
It is the best surgical option if you have mild to moderate ptosis and your levator muscle is not completely damaged. Your doctor can choose one of the three following approaches for this operation:
- Everbush Operation: In this operation, your doctor resects the levator muscle by an incision through your skin.
- Blaskovics Operation: In Blaskovics, your doctor approaches the levator muscle through your palpebral conjunctiva.
- Fasanella-Servat Operation: If you have minor ptosis, your surgeon may choose this option. In this approach, your surgeon cuts the Muller’s muscle, tarsal plate (connective tissue), palpebral conjunctiva, and the levator palpebrae superioris muscle.
Motais Operation
This operation is beneficial when your levator muscle is not functioning, and resection is not helpful. In addition to the levator muscle, the superior rectus muscle also helps to elevate your eyes. In the Motais operation, your surgeon utilizes this function of the superior rectus to treat this condition.
Mullerectomy:
Müllerectomy can be considered for treating Horner syndrome and mild ptosis (1 to 2 mm). The potential benefit of this procedure can be assessed by instilling 10% neosynephrine or 2.5% phenylephrine eye drops, which stimulate Müller’s muscle. If the ptosis improves by 2 to 3 mm within 10 minutes, a better response to the surgery is predicted.9Perry JD, Kadakia A, Foster JA. A new algorithm for ptosis repair using conjunctival Müllerectomy with or without tarsectomy. Ophthal Plast Reconstr Surg 2002; 18:426.
Hess’s Operation
If the muscles that elevate your upper eyelid are paralyzed, your doctor may advise you to have Hess’s operation. In this operation, the frontalis muscle (the muscle of your forehead) is used to elevate your drooping upper eyelid.
Frontalis Brow Suspension
When you have severe ptosis, you should choose frontalis brow suspension for its treatment. Your surgeon attaches the frontalis muscle to your upper eyelid with any synthetic material or fascia tunica (sheet of connective tissue). This method is also helpful if you have congenital ptosis.10Ali, A. A., Hassan, A. A. M., & Salman, M. S. (2020). Surgical Treatment of Severe Ptosis by Modified Brow Suspension Technique. Plastic surgery (Oakville, Ont.), 28(1), 40–45. https://doi.org/10.1177/2292550319880923
What are the Complications of Ptosis Repair?
In some cases, you may experience complications after its repair.
These are:
Early Complications:
Complications you may experience after one or two days of repair are:
- Asymmetry in your eyelid shape
- Asymmetry in your eyelid height
- Infection at the surgical site
- Postoperative bleeding
- Incomplete closure of your palpebral fissure (area between your two eyelids)
Most of these complications get better on their own after some time.
Late Complications:
Complications that you get after one to two weeks of repair are late complications. These are:
- Exposure keratopathy (dryness in your eye due to its incomplete closure)
- Permanent lagophthalmos (abnormal closure of your eyelids)
- Recurrent ptosis
You may need revision surgery to treat these complications.11Collin J. R. (1979). Complications of ptosis surgery and their management: a review. Journal of the Royal Society of Medicine, 72(1), 25–26. https://doi.org/10.1177/014107687907200109
What is the Prognosis of Ptosis?
The prognosis is good if you make a better choice for its treatment. Better preoperative evaluation and management help to treat this condition completely. For example, if your levator is wholly paralyzed and you go for levator resection for its treatment, it will give poor results. Moreover, it is essential for you to take proper postoperative care for better outcomes and to avoid any postoperative complications.12Zikić, Z., Ljutica, M., Karabeg, R., & Stamenkovic, M. (2020). Outcomes of Early Correction of Congenital Myogenic Ptosis Using Transconjunctival Levator Plication. Medical archives (Sarajevo, Bosnia and Herzegovina), 74(3), 205–209. https://doi.org/10.5455/medarh.2020.74.205-209
Difference between Dermatochalasis & Ptosis
Both ptosis and dermatochalasis cause the upper eyelid to drop. In ptosis, the muscles that elevate the upper eyelid become defective and cause it to fall. On the other hand, in dermatochalasis, the upper eyelid drops due to the presence of extra skin or fat on it. Dermatochalasis mainly occurs later in life because the eyes lose elasticity with age.
Conclusion
In conclusion, drooping upper eyelids are caused by defective eye muscles or underlying diseases like myasthenia gravis or Horner syndrome. This condition is not impossible to treat. You can make your eye cosmetically pleasing by choosing a better surgical option. Taking good care of your eye after repair is crucial to avoid complications.
Refrences
- 1McInnes, C. W., & Lee-Wing, M. (2015). Eyelid ptosis. CMAJ : Canadian Medical Association journal = journal de l’Association medicale canadienne, 187(14), 1074. https://doi.org/10.1503/cmaj.140579
- 2Finsterer J. (2003). Ptosis: causes, presentation, and management. Aesthetic plastic surgery, 27(3), 193–204. https://doi.org/10.1007/s00266-003-0127-5
- 3UpToDate. (n.d.). Overview of ptosis. Retrieved June 15, 2024, from https://www.uptodate.com/contents/overview-of-ptosis?search=ptosis&source=search_result&selectedTitle=1%7E150&usage_type=default&display_rank=1
- 4Keene, K. R., Kan, H. E., van der Meeren, S., Verbist, B. M., Tannemaat, M. R., Beenakker, J. M., & Verschuuren, J. J. G. M. (2022). Clinical and imaging clues to the diagnosis and follow-up of ptosis and ophthalmoparesis. Journal of cachexia, sarcopenia, and muscle, 13(6), 2820–2834. https://doi.org/10.1002/jcsm.13089
- 5Grace Lee, N., Lin, L. W., Mehta, S., & Freitag, S. K. (2015). Response to phenylephrine testing in upper eyelids with ptosis. Digital journal of ophthalmology: DJO, 21(3), 1–12. https://doi.org/10.5693/djo.01.2015.05.001
- 6Buechner, S., & Capone, L. (2021). Ice Pack Test Eased Ptosis in a Patient Presenting with a Possible Oculomotor Nerve Schwannoma: A Case Report. Neurology International, 13(4), 510–516. https://doi.org/10.3390/neurolint13040050
- 7Ural O, Mocan MC, Dolgun A, Erdener U. The utility of margin-reflex distance in determining the type of surgical intervention for congenital blepharoptosis. Indian J Ophthalmol. 2016 Oct;64(10):752-755. doi: 10.4103/0301-4738.195016. PMID: 27905338; PMCID: PMC5168917.
- 8Ural, O., Mocan, M. C., Dolgun, A., & Erdener, U. (2016). The utility of margin-reflex distance in determining the type of surgical intervention for congenital blepharoptosis. Indian journal of ophthalmology, 64(10), 752–755. https://doi.org/10.4103/0301-4738.195016
- 9Perry JD, Kadakia A, Foster JA. A new algorithm for ptosis repair using conjunctival Müllerectomy with or without tarsectomy. Ophthal Plast Reconstr Surg 2002; 18:426.
- 10Ali, A. A., Hassan, A. A. M., & Salman, M. S. (2020). Surgical Treatment of Severe Ptosis by Modified Brow Suspension Technique. Plastic surgery (Oakville, Ont.), 28(1), 40–45. https://doi.org/10.1177/2292550319880923
- 11Collin J. R. (1979). Complications of ptosis surgery and their management: a review. Journal of the Royal Society of Medicine, 72(1), 25–26. https://doi.org/10.1177/014107687907200109
- 12Zikić, Z., Ljutica, M., Karabeg, R., & Stamenkovic, M. (2020). Outcomes of Early Correction of Congenital Myogenic Ptosis Using Transconjunctival Levator Plication. Medical archives (Sarajevo, Bosnia and Herzegovina), 74(3), 205–209. https://doi.org/10.5455/medarh.2020.74.205-209

