Button battery ingestion is a growing health concern, especially among children. These small, coin-shaped batteries—also called disc batteries—are found in various household electronics, including watches, calculators, toys, and hearing aids. With the increasing demand for compact electronic devices over recent decades, the number of reported battery ingestions has also gone up.
Ingestions of button batteries can cause significant injuries when swallowed. Fortunately, most cases are benign. In fact, more than 97% of ingestion cases result in either minor symptoms or no symptoms at all.1Newman, R.K., B. Dijkstra, and J. Gibson, Disk Battery Ingestion. 2017. However, complications—though rare—can be severe. When lodged in the esophagus or other parts of the aerodigestive tract, button batteries can cause tissue damage due to electrical discharge, pressure necrosis, or leakage of caustic contents. This can lead to severe injuries involving the esophagus, trachea, vocal cords, and adjacent structures, including the laryngeal nerve.
Epidemiology
The American Poison Control Centers reported more than 3,300 button battery ingestions every year.2Eliason, M.J., R.L. Ricca, and T.Q. Gallagher, Button battery ingestion in children. Current opinion in otolaryngology & head and neck surgery, 2017. 25(6): p. 520-526. Most of the cases of ingestion were observed in children under the age of six years. The peak frequency of cases was in children between the ages of one and three years. The second peak frequency of ingestion is in elderly patients. Almost 10% of the cases occur in patients between the ages of 60 and 89.3Newman, R.K., B. Dijkstra, and J. Gibson, Disk Battery Ingestion. 2017.
A slight male predominance occurs in button battery ingestions. Elderly patients are likely to have the batteries lodged in the small or large intestines. The majority of ingestions in both children and older people remain unwitnessed. Over the last decade, researchers have observed a seven-fold increase in the incidence of severe morbidity and mortality. This rise is not only due to the increasing incidence of ingestion but also due to the increased use of more powerful and larger batteries.4Eliason, M.J., R.L. Ricca, and T.Q. Gallagher, Button battery ingestion in children. Current opinion in otolaryngology & head and neck surgery, 2017. 25(6): p. 520-526.
Etiology
Injuries occur when batteries get swallowed or aspirated. After ingestion, most of them pass through the gastrointestinal (GI) tract. Damages or injuries only occur when these batteries become lodged in the oropharynx, nasopharynx, trachea, and esophagus. Lodging can lead to perforation, ulceration, local injury, and, ultimately, the formation of a fistula. Damage can be acute, and long-term sequelae can occur weeks after the injury and initial intervention.5Litovitz, T., et al., Emerging battery-ingestion hazard: clinical implications. Pediatrics, 2010. 125(6): p. 1168-1177.
Pathophysiology
Researchers have theorized several mechanisms of injury. These include:
- Direct electrical discharge
- Local pressure necrosis
- Heavy metal toxicity and
- Corrosive damage due to the leakage of the battery contents
The most likely mechanism to occur is electrical injuries. When a disk battery enters an acidic environment of the GI tract, it causes an electrochemical reaction. This reaction leads to the generation of hydroxide ions at the battery’s negative pole (cathode), causing alkaline burns and tissue damage, particularly in the esophagus. Fragmentation and Corrosion occur in those batteries that stay in the stomach for more than 48 hours.6Newman, R.K., B. Dijkstra, and J. Gibson, Disk Battery Ingestion. 2017. Over time, this can lead to leakage of caustic materials and heavy metals, contributing to further injury.
Batteries containing mercuric oxide are more likely to fragment compared to those made with other chemical compositions.7Schreiner, I. and W. Bonadio, Disk battery ingestion in a toddler: less than meets the eye. The Journal of Emergency Medicine, 2017. 52(6): p. 863-866.
Clinical Manifestations
The clinical presentation of ingestion varies based on the timing of ingestion, the type of battery ingested, and its location in the body. Most of the patients with suspected ingestions are asymptomatic.
Early Signs:
Unwitnessed esophageal obstructions may result in symptoms that either result from the blockage of the esophagus or windpipe or due to a chemical burn as it erodes. The signs and symptoms can include:
- Coughing
- Drooling
- Choking
- Gagging
- Neck pain
- Chest pain
- Blood in the saliva
- Phlegm
- Difficulty in breathing
- Wheezing
- Retching
- Bloody vomits
- Dysphagia
- Irritability
- Abdominal pain
Later Signs or Symptoms:
When the battery erodes through the surrounding structures of the esophagus, your child may become progressively sicker. The signs observed include:
- Chills
- Fever
- Fast heart rate
- Unconsciousness
- Decreased energy
- Breathlessness (dyspnea)8Samantha W.E. Knight, M. Button Battery Ingestion. 2023; Available from: https://www.pedsurglibrary.com/apsa/repview?type=682-141&name=120_1884007_PDF.
- Stridor
- Bloody stools (hematochezia)
- Hoarseness
- Hematemesis
- Melena (Black, tarry stools indicating upper GI bleeding)
A battery present in the nasopharyngeal cavity presents a bloody nasal discharge.
Diagnosis
If button battery ingestion is witnessed, bring your child to the emergency department so that removal can be done immediately to prevent progressive damage to the esophagus.
History & Physical Examination:
No physical inspection findings are specific to battery ingestion. If the battery is present in the nasal cavity, it can be visualized directly. Findings in patients with ingested batteries in the esophagus or distal organs are unremarkable. The history includes:
- What was the type of battery?
- When was the battery last changed? (Fresh batteries pose a higher risk of injury due to higher voltage.)
- What was the time of ingestion? The chances of more severe injury are higher after two to four hours of ingestion.
- The number of batteries ingested?
Imaging Tests:
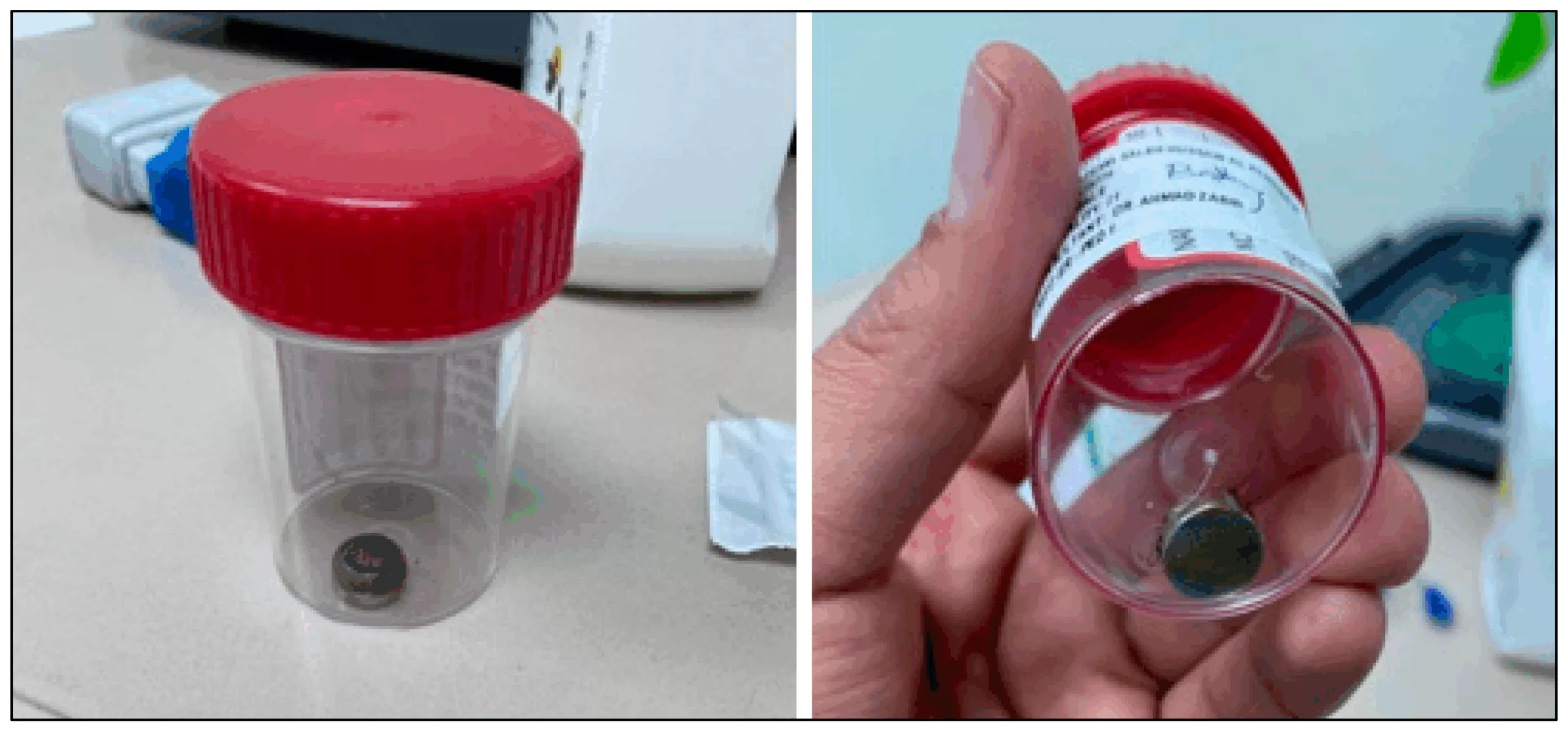
The doctors perform plain radiographs, such as X-rays with both lateral and anteroposterior views of the neck, head, abdomen, and chest, for the evaluation of the suspected battery ingestion. In the lateral view, button batteries show a characteristic step-off at the edge. In the anteroposterior view, it presents a double density or halo sign in the X-ray.9Thabet, M.H., W.M. Basha, and S. Askar, Button battery foreign bodies in children: hazards, management, and recommendations. BioMed Research International, 2013. 2013(1): p. 846091.
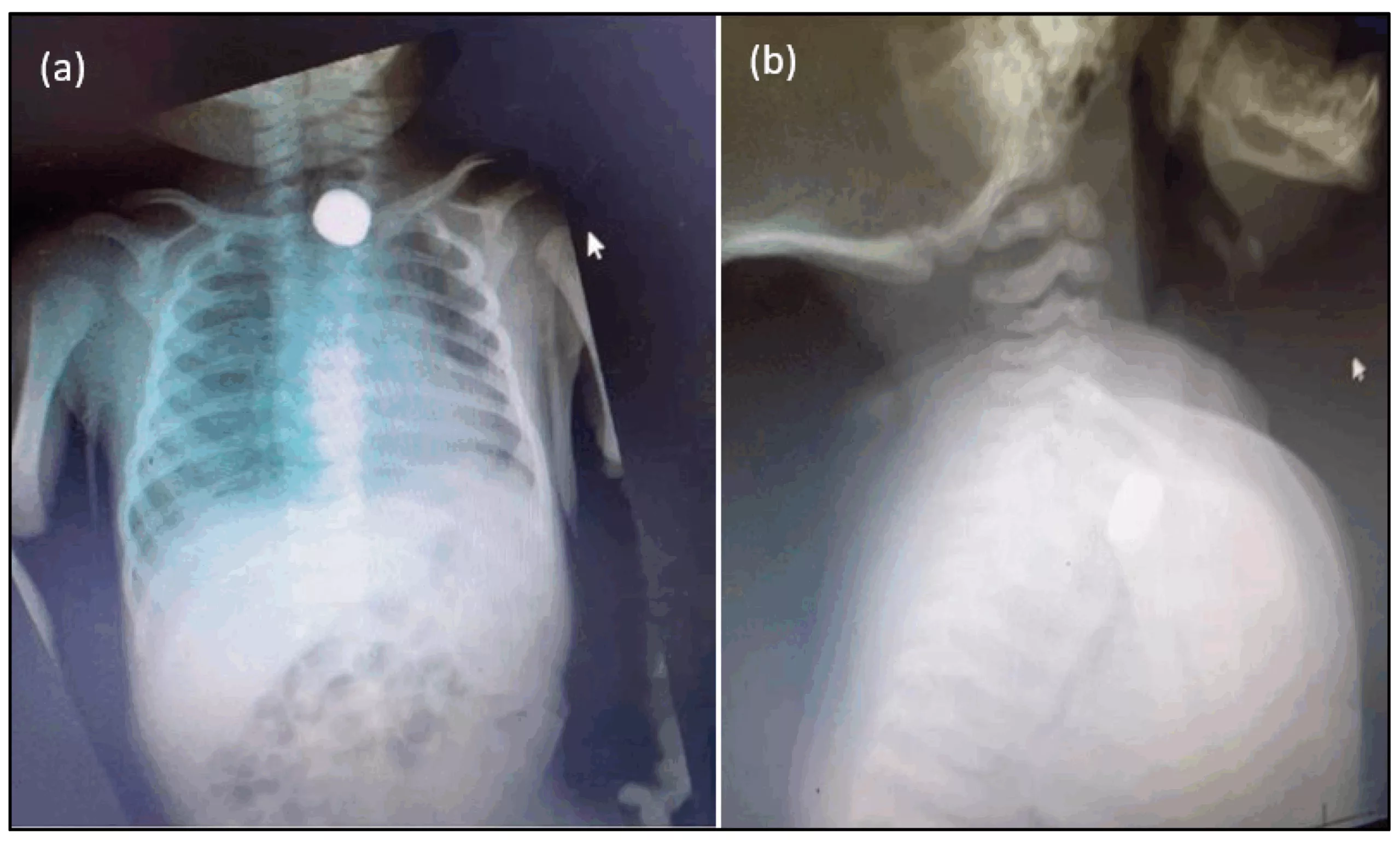
Care should be taken to make a precise diagnosis, as disc batteries can often be mistaken for coins. Hence, repeating films at alternate angles can aid in diagnosis, and doctors need to recognize this, as it requires emergent removal.
If imaging shows fluid accumulation in the chest cavity (pleural effusion), it may indicate esophageal perforation, a surgical emergency.
An esophagram (contrast swallow study) may be performed if perforation is suspected. The patient ingests a contrast agent, and real-time X-rays are taken during swallowing to assess for leaks or perforations in the esophagus.
Treatment & Management
Initial management of button battery ingestion involves assessing the child’s age, the size and type of battery ingested, the time since ingestion, and the current location of the battery within the gastrointestinal tract.
If imaging confirms that the battery has passed beyond the esophagus and is located in the stomach or intestines, and the child is asymptomatic, observation at home is usually safe. In such low-risk cases, the battery is expected to pass naturally in the stool. Asymptomatic children who have passed the battery into the stomach without complications carry a very low risk of morbidity.
Medications:
For children over one year of age, honey or sucralfate may be recommended if ingestion occurred within the last 12 hours. These substances may help coat the mucosa and reduce tissue injury caused by ongoing electrochemical reactions. Honey should be avoided in children under one year due to the risk of infant botulism. Antibiotics may be prescribed if there is concern for esophageal injury, especially if a fistula is suspected. The child may need inhalers if they are wheezing.
Endoscopy or Esophagoscopy:
In high-risk patients (those under six years old with a battery size of 15mm or more), endoscopic removal is the best option.10Leinwand, K., D.E. Brumbaugh, and R.E. Kramer, Button battery ingestion in children: a paradigm for management of severe pediatric foreign body ingestions. Gastrointestinal Endoscopy Clinics, 2016. 26(1): p. 99-118.
Endoscopy is a procedure in which a thin camera is placed in the mouth and then gently pushed through the esophagus and other organs if needed. It requires anesthesia or sedation. Through this procedure, the doctor removes the battery and looks at the evidence of damage or injury directly.
Bronchoscopy:
In some cases, a bronchoscopy may be performed to assess the airways. This involves inserting a telescope-like device to examine the vocal cords, trachea, and bronchi. Even when the battery is in the esophagus, burns may extend to adjacent airway structures, warranting this evaluation.
Surgery:
Surgical intervention is rare but may be required if the battery causes severe complications such as esophageal perforation, fistula formation, or life-threatening symptoms. Surgery is generally reserved for patients who do not improve with conservative or endoscopic management.
Post Button Battery Removal Care:
The post-removal care depends upon the severity of the injury.
- Patients with moderate injuries require hospitalization for a few days, while those with mild injuries are discharged soon after the battery removal.
- Patients with severe injuries will require hospitalization (probably in the intensive care unit) until the recovery of injury.
Complications
Complications due to button battery ingestions can vary widely and include:
- Esophageal or tracheoesophageal fistula formation
- Pneumothorax
- Mediastinitis
- Pneumonia
- Vertebral osteomyelitis
- Peritonitis
- Intestinal perforation
- Vocal cord paralysis
- Recurrent laryngeal nerve injuries11Newman, R.K., B. Dijkstra, and J. Gibson, Disk Battery Ingestion. 2017.
Final Remarks
Button battery ingestion is a common problem, most often seen in emergency departments. It is more common in children who are merely interested in exploring their home environment. The key to managing button battery ingestion is educating parents to keep these items out of reach of children to prevent ingestion.
Refrences
- 1Newman, R.K., B. Dijkstra, and J. Gibson, Disk Battery Ingestion. 2017.
- 2Eliason, M.J., R.L. Ricca, and T.Q. Gallagher, Button battery ingestion in children. Current opinion in otolaryngology & head and neck surgery, 2017. 25(6): p. 520-526.
- 3Newman, R.K., B. Dijkstra, and J. Gibson, Disk Battery Ingestion. 2017.
- 4Eliason, M.J., R.L. Ricca, and T.Q. Gallagher, Button battery ingestion in children. Current opinion in otolaryngology & head and neck surgery, 2017. 25(6): p. 520-526.
- 5Litovitz, T., et al., Emerging battery-ingestion hazard: clinical implications. Pediatrics, 2010. 125(6): p. 1168-1177.
- 6Newman, R.K., B. Dijkstra, and J. Gibson, Disk Battery Ingestion. 2017.
- 7Schreiner, I. and W. Bonadio, Disk battery ingestion in a toddler: less than meets the eye. The Journal of Emergency Medicine, 2017. 52(6): p. 863-866.
- 8Samantha W.E. Knight, M. Button Battery Ingestion. 2023; Available from: https://www.pedsurglibrary.com/apsa/repview?type=682-141&name=120_1884007_PDF.
- 9Thabet, M.H., W.M. Basha, and S. Askar, Button battery foreign bodies in children: hazards, management, and recommendations. BioMed Research International, 2013. 2013(1): p. 846091.
- 10Leinwand, K., D.E. Brumbaugh, and R.E. Kramer, Button battery ingestion in children: a paradigm for management of severe pediatric foreign body ingestions. Gastrointestinal Endoscopy Clinics, 2016. 26(1): p. 99-118.
- 11Newman, R.K., B. Dijkstra, and J. Gibson, Disk Battery Ingestion. 2017.





