Cannabis use disorder (CUD) is a recognized psychiatric condition characterized by problematic cannabis use that leads to clinically significant impairment or distress. It involves changes in brain chemistry and behavior, making it difficult for individuals to reduce or control their use, even when it interferes with their daily lives.
Cannabis, also commonly known as marijuana or weed, is one of the most widely used psychoactive substances in the world. It has been legalised in at least twenty-seven states in the world. Some people believe that it’s not truly addictive because many individuals use it occasionally for satisfaction or as a form of therapy, but that’s a myth. It is actually the fourth most common addiction worldwide, following alcohol, caffeine, and tobacco.1Hall, W., & Degenhardt, L. (2009). Adverse health effects of non-medical cannabis use. The Lancet, 374(9698), 1383–1391.https://doi.org/10.1016/S0140-6736(09)61037-0
The more your body consumes cannabis, the more it builds dependence, and over time, it becomes extremely difficult to stop its use. In the last few decades, there has been a noticeable rise in cannabis use due to its legalization in many Western countries. As a result, young adults and teenagers across the world are showing high rates of cannabis addiction.2UNODC World Drug Report 2023 – United Nations Office on Drugs and Crime https://www.unodc.org/unodc/en/data-and-analysis/world-drug-report-2023.html
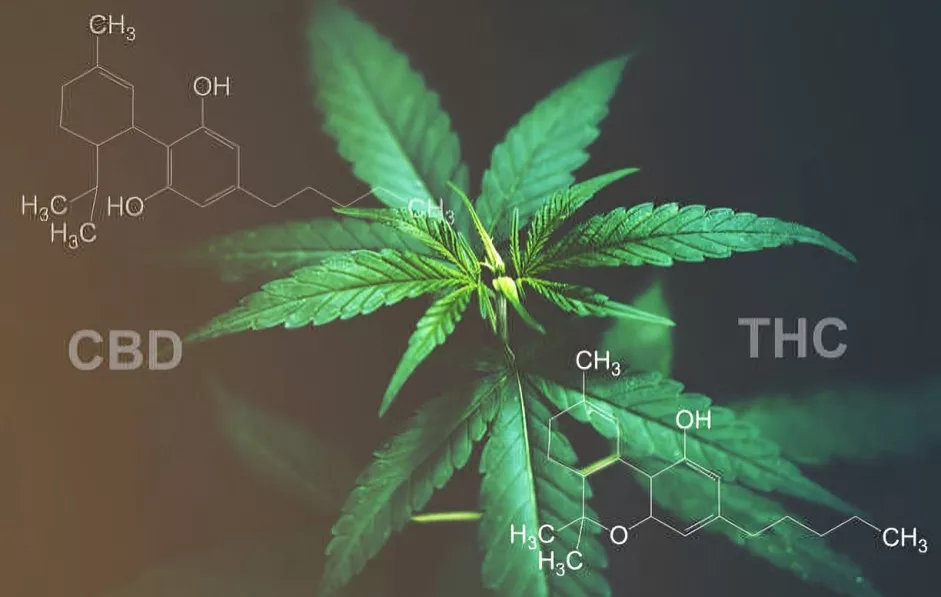
Key Compounds in Cannabis
Cannabis is a plant that belongs to the Cannabaceae family and contains two main active compounds: THC (tetrahydrocannabinol), which is responsible for its psychoactive effects, and CBD (cannabidiol), which has potential therapeutic benefits without causing a “high.” Unlike THC, CBD does not lead to dependence or intoxication.3Connor, J. P., Stjepanović, D., Le Foll, B., Hoch, E., Budney, A. J., & Hall, W. D. (2021). Cannabis use and cannabis use disorder. Nature reviews. Disease primers, 7(1), 16. https://doi.org/10.1038/s41572-021-00247-4

How THC Works and Why It’s Addictive?
Tetrahydrocannabinol (THC) is an intoxicating material, and its consumption can cause altered effects in the human brain. THC chemicals impact the brain in a way that causes a person to become confused, have a distorted perception of reality, and shift moods. Not only does THC consumption leave an impact on emotional well-being, but it also damages the physical health of a person.THC quickly enters the bloodstream when inhaled, most commonly through smoking or vaping, and reaches the brain within seconds. Once in the brain, it binds to cannabinoid receptors (CB1 and CB2), which are part of the endocannabinoid system. This interaction triggers the release of several neurotransmitters, most notably:
- Glutamate (involved in learning and memory. These changes affect mood, memory, pain perception, appetite, and other brain functions.)
- Dopamine (associated with pleasure and reward)
- Serotonin (affects mood and emotional balance)
Repeated stimulation of dopamine pathways by THC can lead to psychological dependence. This makes users crave cannabis to feel good or cope with stress, eventually leading to tolerance (needing more to get the same effect) and withdrawal symptoms when use stops.4Ferland, J. N., & Hurd, Y. L. (2020). Deconstructing the neurobiology of cannabis use disorder. Nature neuroscience, 23(5), 600–610. https://doi.org/10.1038/s41593-020-0611-0
Moreover, THC is lipophilic (fat-loving); it binds to fat cells and can stay in the body for several weeks after use. Its slow elimination makes detox and withdrawal more difficult, especially for chronic users.
Ways THC Is Consumed
Currently, there are multiple ways to consume THC, and it is available in different forms. For instance:
- Rolled into a cigarette (Most common form)
- Extracts are burnt and used as an electronic vape
- Smoked from a pipe or vaporiser
- Present in certain foods
- Used as a drink
Epidemiology of Cannabis Use Disorder
In 2015, the use of Cannabis in the world was about 4%, involving 8% teenagers in the US and 16% in Europe. Among all the users of Cannabis, almost 9% develop addiction to it, which mainly involves adults. Interestingly, CUD has also been reported in healthcare settings, particularly among psychiatric residents, some of whom use cannabis out of curiosity or stress relief.
Almost 4% of pregnant women admit to taking Cannabis during pregnancy, which also led to many complications during childbirth. Moreover, the percentage of women who use Cannabis during breastfeeding is nearly 18%.
With the increase in consumption of Cannabis among adults, there is also a significant increase in its exposure to children.5Shah, K., Farwa, U. E., Vanaparti, A., Patel, S., Kanumuri, M., Vashishth, O., Hossain, N., Dahiya, R., Banala, M., Enamorado, F. R. P., Patel, A. S., Nadeem, H., Kanani, R., Desai, H. D., Sharma, K. H., & Tripathi, S. (2024). Global epidemiology of cannabis use disorders and its trend from 1990 to 2019: Benchmarking analysis of the global burden of disease study. Journal of family medicine and primary care, 13(3), 881–889. https://doi.org/10.4103/jfmpc.jfmpc_824_23
Common Causes of Cannabis Use Disorder
The causes of Cannabis use disorder depend on the particular region. Most teenagers use it to get socially accepted. Some students use it to experiment with a new product or for enjoyment. Almost 12% of the people use cannabis to cope with their stress, anxiety, and also to overcome the symptoms of post-traumatic stress disorder. Cannabis use disorder development depends on the frequency of its use. Some people may develop cannabis use disorder by using small amounts for an extended period.
In some cases, pregnant women also turn to cannabis to relieve nausea, pain, or anxiety, which can increase the risk of CUD. The likelihood of developing this disorder often depends on how frequently and how much cannabis is used, even if the amount is small but used over a long time.6Tarter, R., Kirisci, L., & Reynolds, M. (2014). A new approach to researching the etiology of cannabis use disorder: integrating transmissible and nontransmissible risk within a developmental framework. Substance abuse, 35(4), 336–343. https://doi.org/10.1080/08897077.2014.956918
Risk Factors of Cannabis Use Disorder
Several factors can potentially increase the risk of cannabis use disorder, such as younger age, as in these years, young adolescents are shaping their personalities and going through phases of development that at times might seem overwhelming and emotionally draining. For this reason, they might find cannabis use therapeutic.
A previous history of any psychiatric disorder is a major risk factor for cannabis use disorder. Another risk factor of cannabis use disorder is a family history of mental health disorders.7Masataka, Y., Sugiyama, T., Akahoshi, Y., & Matsumoto, T. (2023). Risk factors for cannabis use disorders and cannabis psychosis in Japan: Second report of a survey on cannabis-related health problems among community cannabis users using social networking services. Neuropsychopharmacology reports, 43(1), 85–94. https://doi.org/10.1002/npr2.12307
Symptoms of Cannabis Use Disorder
Symptoms of cannabis use disorder vary depending on how frequently and how much cannabis is used. The mental status of the individual often reflects whether they are experiencing the acute or chronic phase of use. Each phase shows different signs and symptoms, such as intoxication, withdrawal, or cannabis-induced psychiatric disorders.
In the acute phase, symptoms may include a mix of intoxication and withdrawal signs like delirium, psychosis, anxiety, and insomnia, while the chronic phase is typically marked by disordered behavior.8 Pellegrino, A. J., Duck, K. D., Kriescher, D. P. J., Shrake, M. E., Phillips, M. M., Lalonde, T. L., & Phillips, K. T. (2020). Characterizing symptoms of cannabis use disorder in a sample of college students. Journal of drug issues, 50(4), 524–537. https://doi.org/10.1177/0022042620936655
Cannabis intoxication may present with:
- Euphoria (a state of intense happiness)
- Uncontrollable laughter
- Anxiety or nervousness
- Forgetfulness and restlessness
- Fast heart rate (tachycardia)
- Dry mouth9Sorkhou, M., Dent, E. L., & George, T. P. (2024). Cannabis use and mood disorders: a systematic review. Frontiers in public health, 12, 1346207. https://doi.org/10.3389/fpubh.2024.1346207
Long-term use or withdrawal may lead to:
- Low motivation
- Irritability
- Loss of interest in daily activities
- Social isolation
It’s important to rule out other mental health conditions like persistent depressive disorder or generalized anxiety disorder, which can have similar symptoms. Also, some cannabis-related conditions should be excluded before confirming a diagnosis of cannabis use disorder.
Related Cannabis Conditions
Cannabis Intoxication:
It typically presents with motor incoordination, anxiety, social withdrawal, and impaired judgment. Increased appetite, dry mouth, and tachycardia are some other symptoms of cannabis intoxication.
Cannabis Withdrawal:
Cannabis withdrawal symptoms develop when a person is taking cannabis almost daily for some months, and when he withdraws its usage, he presents with the following signs and symptoms within a week: 10Bonnet, U., & Preuss, U. W. (2017). The cannabis withdrawal syndrome: current insights. Substance abuse and rehabilitation, 8, 9–37. https://doi.org/10.2147/SAR.S109576
- Anger
- Depression and anxiety
- Insomnia ( lack of sleep)
- Weight loss with decreased appetite
- Tremors
- Abdominal pain
- Fever
- Chills
How to diagnose Cannabis Use Disorder?
Doctors usually look for recurring patterns in the patient, their distress level, intolerance, inability to spend days without cannabis use, or strong desire for cannabis consumption, and withdrawal symptoms. It’s also necessary to differentiate between symptoms of CUD and other psychiatric conditions like depression or anxiety. There are some cannabis associated conditions like Cannabis intoxication, cannabis withdrawal, cannabis induced psychiatric and anxiety disorders. Symptoms of these conditions may resemble cannabis use disorder.11Fink, D. S., Shmulewitz, D., Mannes, Z. L., Stohl, M., Livne, O., Wall, M., & Hasin, D. S. (2022). Construct validity of DSM-5 cannabis use disorder diagnosis and severity levels in adults with problematic substance use. Journal of Psychiatric Research, 155, 387–394. https://doi.org/10.1016/j.jpsychires.2022.09.016
A proper and detailed history and examination help to diagnose cannabis use disorder. The following is a criterion to diagnose cannabis use disorder. A person is considered to have cannabis use disorder if they meet at least two of the following criteria within 12 months:
- The use of Cannabis in large amounts or taking cannabis for an extended period of time.
- A strong desire to take Cannabis and make a significant effort to withdraw from it.
- Inability to perform daily life activities or work.
- Reducing or giving up activities because of use.
- Isolation from people and avoiding going out.
- Gradual increase in the amount of cannabis use, i-e, increase in its tolerance.
- The use of cannabis despite knowing its adverse neurological and physical problems.
- Withdrawal symptoms or using cannabis to avoid withdrawal.
- Using in risky or dangerous situations.
The severity depends on the number of criteria met:
- 2–3: Mild
- 4–5: Moderate
- 6 or more: Severe
Role of Laboratory Testing
Some laboratory tests also aid in diagnosing cannabis use disorder. The laboratory tests of urine, blood, hair, and saliva help to detect the presence of cannabis. It is important to compare the clinical symptoms of cannabis use disorder with these laboratory tests. All laboratory tests detect the primary active metabolite in cannabis, which is delta-9-tetrahydrocannabinol. However, a negative test result does not necessarily rule out cannabis use, especially in chronic users. This is because regular cannabis use results in higher tolerance and may need more substantial quantities for detection.12 Artigaud, L., Fener, C., Bisch, M., Schwan, R., Schwitzer, T., De Ternay, J., Adamson, S. J., Rolland, B., & Laprévote, V. (2020). Les outils de repérage pour les troubles de l’usage du cannabis et leur adaptation au DSM-5 : une revue de littérature [Screening tools for cannabis use disorders and their adaptation to DSM-5: A literature review]. L’Encephale, 46(5), 382–389. https://doi.org/10.1016/j.encep.2020.02.010

Doctors prescribe some other tests too to rule out conditions that are similar to cannabis use disorder. These tests include head imaging, lab tests for heavy metals, immunological markers, hormones, electrolytes, and infection markers.
Treatment for Cannabis Use Disorder
The main goal of treatment is to help the person become functional and drug-free. Both psychiatric and psychological management are necessary, as psychiatric evaluation aids in diagnosing any other underlying disease, and the counselling sessions by a good psychologist help the patient to change their behavior and make them able to deal with the cannabis use disorder.13Sherman, B. J., & McRae-Clark, A. L. (2016). Treatment of Cannabis Use Disorder: Current Science and Future Outlook. Pharmacotherapy, 36(5), 511–535. https://doi.org/10.1002/phar.1747
For those with heavy or long-term use, doctors recommend gradual reduction rather than abrupt cessation to minimize withdrawal symptoms.14Walther, L., Gantner, A., Heinz, A., & Majić, T. (2016). Evidence-based Treatment Options in Cannabis Dependency. Deutsches Arzteblatt international, 113(39), 653–659. https://doi.org/10.3238/arztebl.2016.0653
There is no specific medication for cannabis use disorder. However, symptomatic treatments can be given:
- Beta-blockers to manage a rapid heart rate
- Benzodiazepines for panic attacks
- Antihistamines for anxiety or insomnia
A calm and supportive environment is often just as crucial as medical intervention.
Complications of Cannabis Use Disorder
Cannabis use disorder has social, physical, and psychological complications. The heavy use of cannabis disturbs the social life of the addict and makes him isolated. It affects the brain by causing addiction, defective brain development, and poor intellect. The use of cannabis in smoked form causes respiratory problems like chronic bronchitis. Heavy Cannabis use can also decrease fertility in both men and women.
The use of cannabis during pregnancy adversely affects the fetus by affecting intelligence, visual memory, and attention. It can also lead to preterm delivery, stillbirth, and low birth weight children.15 Shah, J., & Fermo, O. (2022). Review of systemic and syndromic complications of cannabis use: A review. Medicine, 101(49), e32111. https://doi.org/10.1097/MD.0000000000032111
Prognosis
The outcome depends on the reason and pattern of use. People who try cannabis once or twice out of curiosity are less likely to develop a disorder. However, those who use it regularly for enjoyment or to relieve stress have a much higher risk of addiction.
With proper support and treatment, many individuals can overcome cannabis use disorder and resume a healthy lifestyle.16Budney, A. J., Sofis, M. J., & Borodovsky, J. T. (2019). An update on cannabis use disorder with comment on the impact of policy related to therapeutic and recreational cannabis use. European archives of psychiatry and clinical neuroscience, 269(1), 73–86. https://doi.org/10.1007/s00406-018-0976-1
Conclusion
Cannabis Use Disorder is a growing concern worldwide and should not be taken lightly. Similar to any other drug addiction, it can be treated with regular therapies, and rehabilitation centers can facilitate patients. Instead of directly sending children to rehab centers, it is often suggested that teenagers and young adults who suffer from cannabis use disorder should be provided guidance and support to help them find coping strategies. Regular therapies can go a long way in the treatment of cannabis use disorder.
Furthermore, cannabis should not be easily accessible unless a person needs it for medical purposes, or else it is difficult to stop teenagers and young adults, specifically below 18, from consuming cannabis daily. They should also be told about the adverse effects of cannabis on their health and lifestyle. Cannabis use disorder negatively influences a person’s physical and emotional well-being; therefore, it needs to be banned to protect citizens.
Refrences
- 1Hall, W., & Degenhardt, L. (2009). Adverse health effects of non-medical cannabis use. The Lancet, 374(9698), 1383–1391.https://doi.org/10.1016/S0140-6736(09)61037-0
- 2UNODC World Drug Report 2023 – United Nations Office on Drugs and Crime https://www.unodc.org/unodc/en/data-and-analysis/world-drug-report-2023.html
- 3Connor, J. P., Stjepanović, D., Le Foll, B., Hoch, E., Budney, A. J., & Hall, W. D. (2021). Cannabis use and cannabis use disorder. Nature reviews. Disease primers, 7(1), 16. https://doi.org/10.1038/s41572-021-00247-4
- 4Ferland, J. N., & Hurd, Y. L. (2020). Deconstructing the neurobiology of cannabis use disorder. Nature neuroscience, 23(5), 600–610. https://doi.org/10.1038/s41593-020-0611-0
- 5Shah, K., Farwa, U. E., Vanaparti, A., Patel, S., Kanumuri, M., Vashishth, O., Hossain, N., Dahiya, R., Banala, M., Enamorado, F. R. P., Patel, A. S., Nadeem, H., Kanani, R., Desai, H. D., Sharma, K. H., & Tripathi, S. (2024). Global epidemiology of cannabis use disorders and its trend from 1990 to 2019: Benchmarking analysis of the global burden of disease study. Journal of family medicine and primary care, 13(3), 881–889. https://doi.org/10.4103/jfmpc.jfmpc_824_23
- 6Tarter, R., Kirisci, L., & Reynolds, M. (2014). A new approach to researching the etiology of cannabis use disorder: integrating transmissible and nontransmissible risk within a developmental framework. Substance abuse, 35(4), 336–343. https://doi.org/10.1080/08897077.2014.956918
- 7Masataka, Y., Sugiyama, T., Akahoshi, Y., & Matsumoto, T. (2023). Risk factors for cannabis use disorders and cannabis psychosis in Japan: Second report of a survey on cannabis-related health problems among community cannabis users using social networking services. Neuropsychopharmacology reports, 43(1), 85–94. https://doi.org/10.1002/npr2.12307
- 8Pellegrino, A. J., Duck, K. D., Kriescher, D. P. J., Shrake, M. E., Phillips, M. M., Lalonde, T. L., & Phillips, K. T. (2020). Characterizing symptoms of cannabis use disorder in a sample of college students. Journal of drug issues, 50(4), 524–537. https://doi.org/10.1177/0022042620936655
- 9Sorkhou, M., Dent, E. L., & George, T. P. (2024). Cannabis use and mood disorders: a systematic review. Frontiers in public health, 12, 1346207. https://doi.org/10.3389/fpubh.2024.1346207
- 10Bonnet, U., & Preuss, U. W. (2017). The cannabis withdrawal syndrome: current insights. Substance abuse and rehabilitation, 8, 9–37. https://doi.org/10.2147/SAR.S109576
- 11Fink, D. S., Shmulewitz, D., Mannes, Z. L., Stohl, M., Livne, O., Wall, M., & Hasin, D. S. (2022). Construct validity of DSM-5 cannabis use disorder diagnosis and severity levels in adults with problematic substance use. Journal of Psychiatric Research, 155, 387–394. https://doi.org/10.1016/j.jpsychires.2022.09.016
- 12Artigaud, L., Fener, C., Bisch, M., Schwan, R., Schwitzer, T., De Ternay, J., Adamson, S. J., Rolland, B., & Laprévote, V. (2020). Les outils de repérage pour les troubles de l’usage du cannabis et leur adaptation au DSM-5 : une revue de littérature [Screening tools for cannabis use disorders and their adaptation to DSM-5: A literature review]. L’Encephale, 46(5), 382–389. https://doi.org/10.1016/j.encep.2020.02.010
- 13Sherman, B. J., & McRae-Clark, A. L. (2016). Treatment of Cannabis Use Disorder: Current Science and Future Outlook. Pharmacotherapy, 36(5), 511–535. https://doi.org/10.1002/phar.1747
- 14Walther, L., Gantner, A., Heinz, A., & Majić, T. (2016). Evidence-based Treatment Options in Cannabis Dependency. Deutsches Arzteblatt international, 113(39), 653–659. https://doi.org/10.3238/arztebl.2016.0653
- 15Shah, J., & Fermo, O. (2022). Review of systemic and syndromic complications of cannabis use: A review. Medicine, 101(49), e32111. https://doi.org/10.1097/MD.0000000000032111
- 16Budney, A. J., Sofis, M. J., & Borodovsky, J. T. (2019). An update on cannabis use disorder with comment on the impact of policy related to therapeutic and recreational cannabis use. European archives of psychiatry and clinical neuroscience, 269(1), 73–86. https://doi.org/10.1007/s00406-018-0976-1

