A herniation is derived from the word “hernia,” which means the outpouching of something through an abnormal opening. A herniated disc is defined as bulging out of jelly-like material (nucleus pulposus) through a ruptured outer fibrous layer of the disc. Cervical disc herniation causes neck pain that radiates into the arm.
Neck pain or upper back pain is one of the most common clinical conditions nowadays. The most common cause of neck pain is cervical disc herniation. There are seven cervical vertebrae in our body, starting from the base of the skull and ending at the thoracic spine level (T1). These cervical vertebrae surround spinal nerves and the cervical canal. Herniation results in impinging of the adjacent nerve that induces neurological manifestations such as numbness, tingling sensation, and muscle weakness.
 The prevalence of cervical disc herniation is age dependent. It increases with advancing age due to degenerative changes in the spine. Cervical disc herniation is most common at 30-50 years of age. It is more prevalent in females accounting for 60% of the cases. The incidence of cervical disc herniation is 5-20 cases per 1000 patients. 1Sharrak, S. (2022, August 29). Cervical Disc Herniation. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK546618/#:~:text=%5B4%5D%20Cervical%20disc%20herniation%20is,contained%20within%20the%20spinal%20canal.
The prevalence of cervical disc herniation is age dependent. It increases with advancing age due to degenerative changes in the spine. Cervical disc herniation is most common at 30-50 years of age. It is more prevalent in females accounting for 60% of the cases. The incidence of cervical disc herniation is 5-20 cases per 1000 patients. 1Sharrak, S. (2022, August 29). Cervical Disc Herniation. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK546618/#:~:text=%5B4%5D%20Cervical%20disc%20herniation%20is,contained%20within%20the%20spinal%20canal.
What are the Causes of Cervical Disc Herniation?
Anatomically, the cervical disc or intervertebral disc is a cartilaginous structure composed of 3 components:
- Nucleus pulposus (inner part)
- Annulus fibrosus
- End plate (that fixes one vertebra with the others)
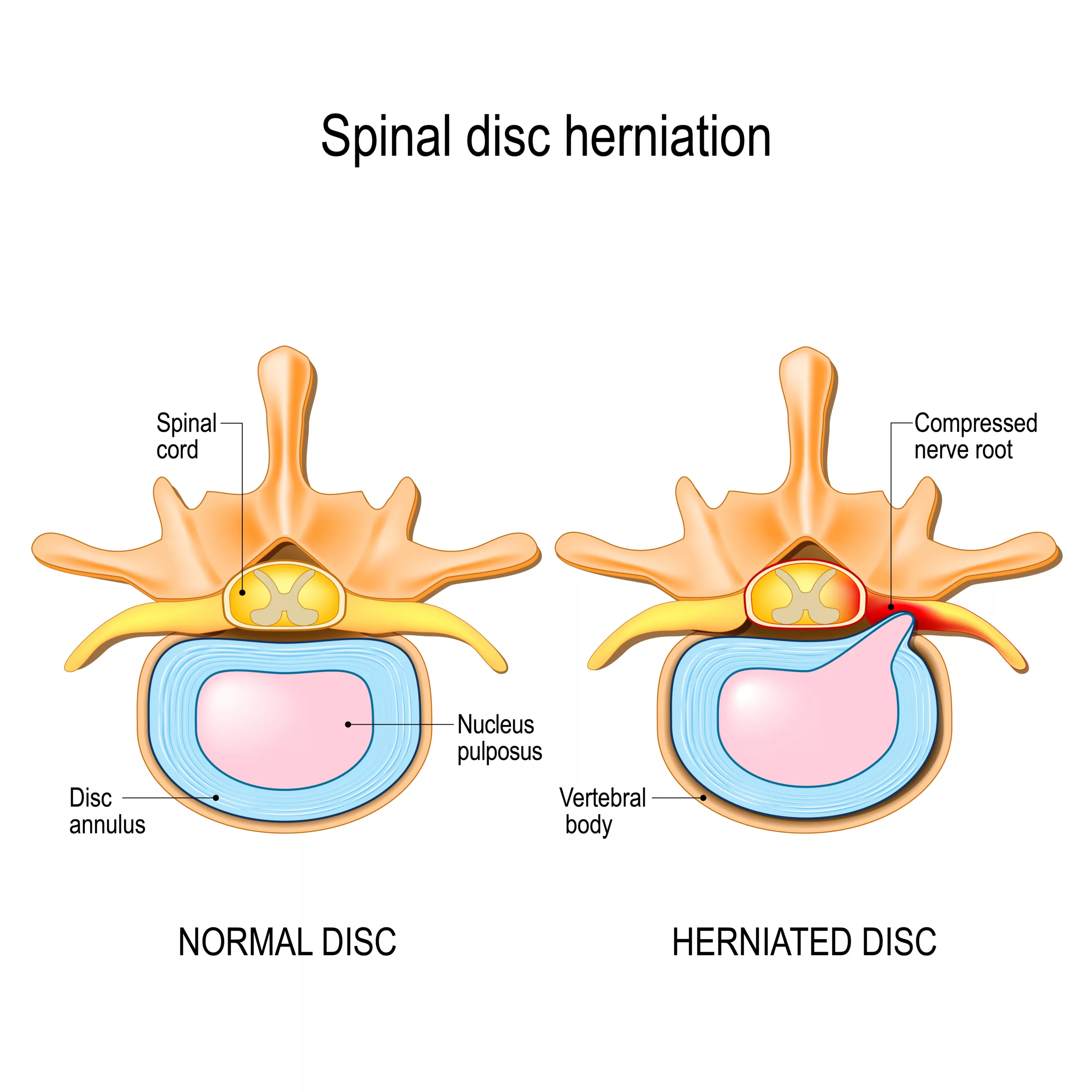
Disc herniation occurs when there is a tear in the nucleus fibrosis resulting in bulging out of the nucleus pulposus. This occurs in the following conditions:
- Injury or trauma to the back
- Disc degeneration associated with aging
- Genetics
What are the Risk Factors of Cervical Disc Herniation?
There are some factors that contribute to causing cervical disc herniation. These include:
- Heavy weight lifting
- Smoking
- Bad posture
- Positive family history
- Frequent driving
- Obesity
What are the Symptoms of Cervical Disc Herniation?
Symptoms of cervical disc herniation vary depending on the location of the cervical disc. It occurs most commonly at the level of the C5-C6-C7 vertebra. If you have a cervical disc herniation, you may have the following symptoms:
- Neck pain (moderate to severe in nature)
- Upper back pain
- Muscle spasm
- Reduced neck or shoulder mobility
- The feeling of ipsilateral (at the same side) numbness in your shoulder, arm, and hand.
- Ipsilateral tingling sensation (pins-needle-like sensation on the same side)
- Weakness of shoulder, arm, and hand muscles
How to Diagnose cervical disc herniation?
Diagnosis of cervical disc herniation begins with taking proper history, physical examination, laboratory, and imaging studies.2Fakhoury, J., & Dowling, T. J. (2023, April 15). Cervical Degenerative Disc Disease. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK560772/
History:
History is the initial step of diagnosis in patients with cervical disc herniation. Your doctor will take a complete history and make a diagnosis accordingly. Your doctor may ask the following question :
- Your age?
- Do you have pain in your neck or upper back? If yes, then how much? Duration of the pain? Any relieving or aggravating factor?
- Do you feel numbness in your arms or hands?
- Do you have weaknesses in your muscles ( bicep, tricep, and hand muscles)?
- Is there any history of trauma?
- Any previous medical illness?
- Medical history?
- Occupational history
- Personal history
- Family history
In addition to the above-mentioned questions, your doctor may also ask these questions about unexplained weight loss, fever and chills, and night sweats, as they can indicate an underlying problem associated with cervical disc herniation.
Physical examination:
In a physical examination, your doctor will do a clinical assessment to diagnose cervical disc herniation. A thorough neurological examination evaluates sensory loss, motor weakness, and reflex abnormalities. After a neurological examination, your doctor will check for the following:
- Temperature / Tenderness in the affected area
- Cervical lymphadenopathy
- Any mass or tumor

Provocative test:
There are three provocative tests to diagnose cervical disc herniations:
Spurling test:
This test is used to diagnose cervical radiculopathy (pinched nerve). In this test, your doctor will ask you to extend your head and rotate it toward the affected side. If symptoms reproduce, the test is positive; otherwise, it is negative. This test is highly specific for cervical disc herniation but has low sensitivity.
Hoffman test:
Hoffman test diagnoses cord compression and myopathies. In this test, your doctor will hold your finger and flick the distal tip downward. If there is flexion and adduction (movement of thumb toward middle finger) of the thumb, then the test is positive; otherwise, it is negative. In correspondence with MRI images, a positive Hoffman test helps with the diagnosis of cervical disc herniation.
Lhermitte sign:
Lhermitte sign also indicates cord compression and cervical radiculopathy. In this test, your doctor will flex your neck resulting in an electrical sensation that travels down the spine and into the extremities. These provocative tests play a crucial role in evaluating cervical disc herniation, as they help medical professionals assess specific aspects of conditions like cervical radiculopathy, myopathies, and cord compression.
Laboratory studies:
Your doctor will also prescribe some laboratory investigations to rule out other diseases. These laboratory investigations include:
- Level of Inflammatory markers in your body (ESR and CRP), If your doctor suspects a chronic systemic illness such as rheumatoid arthritis.
- Complete blood count (CBC)
- Serum uric acid level
- Serum Vit D level
Imaging studies:
In most cases, cervical disc herniation settles down on its own without any medical and surgical intervention within 4-6 weeks. An imaging study is not recommended unless there is a suspicion of potentially serious illness. In case of chronic and persistent pain that hinders the patient’s routine activities, your doctor will prescribe Imaging studies like:
X-ray:
X-ray is the best initial test to diagnose cervical disc herniation because it is the cheapest and most accessible tool in every clinical setup. This radiological modality provides radiographs in three views; anteroposterior, lateral, and oblique. X-ray helps in assessing spinal alignment and degenerative and spondylotic changes.
CT scan:
CT scan is the most sensitive test to examine the bony structure of the spine. It shows herniated discs and other damaged parts in the cervical spine. However, a CT scan can not give information about the soft structures. Your doctor may also prescribe CT myelography to diagnose cervical disc herniation.
MRI:
MRI is the investigation of choice for cervical disc herniation. It gives a detailed and enhanced view and provides a clear view of soft structures.
Electrodiagnostic studies:
It includes electromyography and nerve conduction studies. These tests are used to rule out peripheral myopathy (a disease that affects skeletal muscles).
Treatment of cervical disc herniation
Your doctor will prefer conservative management to normalize the pathology before opting for surgery. There is a step-by-step treatment approach to treat Cervical disc herniation. If conservative or non-surgical intervention measures fail, your doctor will opt for surgery. The following are non-surgical interventions to manage cervical disc herniation: 32- Corniola, M. V., Tessitore, E., Schaller, K., & Gautschi, O. P. (2015). Hernie discale cervicate–diagnostic et prise en charge [Cervical disc herniation–diagnosis and treatment]. Revue medicale suisse, 11(492), 2023–2029.
Self-care :
Self-care is an important measure that helps you resolve the signs and symptoms of cervical disc herniation. However, you can take the following measures to ameliorate the symptoms:
- Stay active
- Maintain your body posture
- Use collar
- Traction
- Do physiotherapy exercises
- Use of heating and cooling pads
- Good sleep
- Avoid strenuous exercises
- Avoid driving
Pharmacological treatment:
Non-steroidal anti-inflammatory drugs (NSAIDs) are the drugs of choice for the treatment of cervical radiculopathy secondary to cervical disc herniation. Your doctor may prescribe other medications like:
- Analgesics
- Muscle relaxants (e.g. Orphandirne)
- Opioids
- Antidepressants (Amitriptyline)
- Anticonvulsants ( Pregabalin and Gabapentin)
- Oral Steroids
Epidural steroid injection:
If your pain gets worse and halts your physical activity, your doctor will prescribe an epidural steroid injection to reduce pain and inflammation. An epidural injection is given under the x-ray-guided fluoroscopy technique. About 50 percent of the patients feel pain-free after having an epidural steroid injection. Additionally, the Effects of these injections last for weeks, months, or years depending on the dose and formulation.
Surgical treatment:
It is the last option for the patient with no improvement in symptoms after performing the above therapies. Moreover, there are some factors that should be noticed before planning surgery. These factors include:
- Patient age
- Any previous neck surgery
- Any other medical illness
- Expected outcome after surgery
The following are surgical treatment options:
Anterior cervical discectomy and fusion:
It is a minimally invasive procedure in which your surgeon makes a small incision in front of your neck. After dissection of the neck (anteriorly), muscles, nerves, and vessels, he will move aside to avoid injury. Then he will reach the vertebra and remove the ruptured disc that presses the adjacent nerve root. Finally, after removing a part of the affected vertebra, he will fill the gap with a bone graft and do a fusion. With the passage of time, this bony graft will fuse with the vertebra. Screw and metal plates can provide a better fusion and recovery rate.
Artificial disc replacement:
Artificial disc replacement is a surgical procedure to treat cervical disc herniation that involves the placement of an artificial disc instead of fusion. This procedure is more beneficial than fusion, as the disc preserves your natural motion. On the other hand, fusion halts your disc motion.
Minimal invasive endoscopic microdiscectomy:
It is an endoscope-guided, minimally invasive procedure in which a tiny incision is made, and dilators are used to dilate the incised area to reach the affected side. After reaching the affected area, the surgeon will remove the disc endoscopically or through a microscope. This procedure has a good recovery time and less muscle, nerve, and vessel damage.
Posterior cervical discectomy:
It is a surgical procedure in which the incision is made on the posterior side of the neck. Finally, after reaching the affected area, your doctor removes the ruptured disc and widens the cervical canal to avoid further nerve compression after surgery.
Recovery time for cervical herniated disc
The patient’s recovery depends on the surgery and self-care adopted by the patient. In most cases, symptoms improve within two weeks after surgery, and full recovery time is about 2-4 months. Moreover, the following preventive measures can hasten your recovery and avoid recurrence.
- Avoid heavy weight lifting.
- An appropriate physical therapy exercise
- Maintain your body posture
- Proper medication according to the doctor’s prescription
- Lose weight if you are obese
- Avoid smoking
- Avoid stress
Herniated Disc vs. Bulging Disc
A disc bulge is also known as disc prolapse. Unlike herniated discs, bulging discs is a less severe condition. In comparison, the nucleus pulposus bulges out in bulging discs, but the outer fibrous layer of the disc remains intact. While in a herniated disc, there is a hole in the outer fibrous layer through which annulus fibrosus seeps out and compresses adjacent nerves.
Conclusion
To conclude, cervical disc herniation is a painful neck condition that should not be neglected. It can occur due to heavy weight lifting, trauma, bad posture, and injury. It is a treatable condition. Your doctor will prescribe analgesics and anti-inflammatory medications first. Surgery is the treatment of choice for patients who fail to respond to conservative management. Preventive measures like avoiding heavy weight lifting, good body posture, losing weight, and a healthy lifestyle prevent cervical disc herniation.
Refrences
- 1Sharrak, S. (2022, August 29). Cervical Disc Herniation. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK546618/#:~:text=%5B4%5D%20Cervical%20disc%20herniation%20is,contained%20within%20the%20spinal%20canal.
- 2Fakhoury, J., & Dowling, T. J. (2023, April 15). Cervical Degenerative Disc Disease. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK560772/
- 32- Corniola, M. V., Tessitore, E., Schaller, K., & Gautschi, O. P. (2015). Hernie discale cervicate–diagnostic et prise en charge [Cervical disc herniation–diagnosis and treatment]. Revue medicale suisse, 11(492), 2023–2029.