Uterine prolapse is the breaching of the uterus in the vaginal canal through the hymen or introitus (opening) of the vagina. However, it is not a life-threatening disease but can cause severe physical dysfunction, depression, and postural defects in adult females.
What is Uterine Prolapse?
Uterine prolapse refers to a condition in which the uterus descends or slips from its normal position into the vaginal canal or outside the vaginal opening. This occurs when the muscles and ligaments that support the uterus become weak or damaged, causing the uterus to sag downward. It is a type of pelvic organ prolapse that involves the uterus.1C. J. Chen and H. Thompson, “Uterine Prolapse,” in StatPearls, Treasure Island (FL): StatPearls Publishing, 2023. Accessed: Jun. 01, 2023. [Online]. Available: http://www.ncbi.nlm.nih.gov/books/NBK564429/
Pelvic organ prolapse is the protrusion of any organ in the pelvic region, like the uterus, the vagina, the bladder, and the rectum in the vagina, due to the weakening of pelvic floor muscles. It is more common in women with one or more vaginal deliveries after menopause. The severity of the disease depends on the capability of the pelvic floor muscles to further support the uterus.
Stages of Uterine Prolapse
The severity of uterine prolapse can vary. In mild cases, the uterus may only partially descend into the vagina. In more severe cases, the uterus can protrude outside the vaginal opening, leading to discomfort, pain, and difficulty with bowel movements or urination. The following are the stages of prolapse:
- Stage 0:
There is no prolapse. - Stage I:
The prolapse extends more than one centimeter above the level of the hymen at its furthest point. - Stage II:
The prolapse is only one centimeter away from the hymen. - Stage III:
The distant part of the prolapse is greater than 1 cm but does not protrude out of the vagina.2Doshani A, Teo RE, Mayne CJ, Tincello DG. Uterine prolapse. BMJ. 2007 Oct 20;335(7624):819-23. doi: 10.1136/bmj.39356.604074.BE. PMID: 17947787; PMCID: PMC2034734. - Stage IV:
Complete inversion of the vagina. The uterus completely bulges out of the vagina.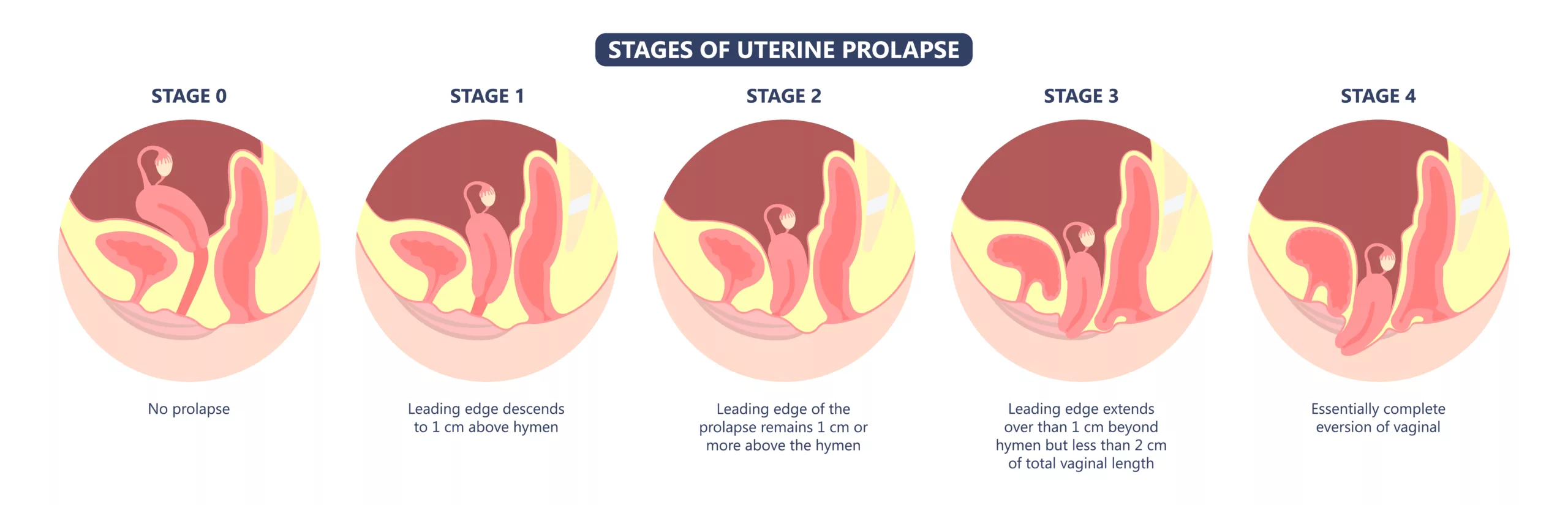
Symptoms of Prolapse
The symptoms of uterine prolapse can vary depending on the severity of the condition. Some common symptoms include:
- Urinary Symptoms: Uterine prolapse can affect the functioning of the bladder, leading to various urinary symptoms. These may include increased frequency of urination, urgency, difficulty emptying the bladder completely, urinary incontinence (leakage of urine), or recurrent urinary tract infections.
- Dyspareunia (Painful intercourse): Women with uterine prolapse may experience discomfort or pain in the pelvic region, lower back, or during sexual intercourse. The pain can range from mild to severe and may be exacerbated by physical activity or prolonged standing.
- Pressure or heaviness in the pelvic region: Many women with uterine prolapse describe a feeling of pressure or heaviness in the pelvic area. It may feel like something is falling out or sagging.
- Constipation: In some cases, uterine prolapse can impact bowel function. Women may experience constipation, difficulty emptying the bowels completely, or a feeling of incomplete bowel movements.
- Vaginal tissue protrusion: In more advanced cases of uterine prolapse, the uterus may descend into the vaginal canal or even protrude outside the vaginal opening. This can be visible and may be accompanied by a feeling of bulging or fullness.
Uterine Prolapse bleeding
As mentioned above, uterine prolapse is the dislocation of the uterus from its usual position; this dislocation can cause vaginal bleeding during sexual intercourse. Vaginal bleeding can be a sign of uterine prolapse. However, uterine prolapse itself does not directly cause vaginal bleeding, particularly during sexual intercourse. Bleeding due to sexual activity, known as postcoital bleeding, can occur due to various reasons or underlying gynecological conditions, such as vaginal tissue irritation, ulceration, or the presence of other abnormalities like cervical polyps, uterine fibroids, or cervical or uterine cancer. It’s essential to consult with a healthcare professional if you experience vaginal bleeding during or after sexual intercourse or have any unexplained or persistent bleeding.
Types of Pelvic Organ Prolapse
Based on the area of weakness and the organs affected, there are six following types of pelvic organ prolapse.
Cystocele:
The pelvic organ prolapse that is most prevalent is the anterior wall prolapse, in which the bladder drops into the vagina due to weakened supporting muscles.
Rectocele:
The rectum drops into the vaginal canal, also known as the posterior wall prolapse.
Apical Prolapse:
The superior part of the vagina itself drops into the vaginal canal.
Uterine Prolapse:
The weakening of pelvic floor muscles causes the uterus to fall into the vaginal canal.
Enterocoele:
Dropping of the small intestine in the vaginal canal.
Urethrocoele:
Protrusion of the urethra in the vaginal canal.
Causes & Risk Factors
The following are the factors that can contribute to developing a uterine prolapse:
- Vaginal delivery: The process of childbirth, particularly multiple vaginal deliveries, can weaken the pelvic floor muscles and ligaments, increasing the risk of uterine prolapse.
- First delivery at an older age: Delivering a baby for the first time at an older age may increase the risk of uterine prolapse due to reduced muscle tone and resilience in the pelvic area.
- Obesity: Excess weight puts additional pressure on the pelvic organs, including the uterus, making it more susceptible to prolapse.
- Delivery of a large baby: Delivering a large baby can stretch the pelvic floor muscles and tissues, potentially leading to weakened support for the uterus.
- Low estrogen levels: Reduced estrogen levels, especially during menopause, can lead to a loss of tissue elasticity and muscle tone in the pelvic area, increasing the risk of uterine prolapse.
- Trauma during labor: Complications or trauma during labor, such as prolonged or difficult deliveries, can damage the pelvic floor muscles and tissues, contributing to uterine prolapse.
- Chronic constipation: Straining during bowel movements due to chronic constipation can put pressure on the pelvic organs and weaken the pelvic floor muscles, potentially leading to uterine prolapse. It’s important to remember that these factors may increase the likelihood of developing uterine prolapse, but they do not guarantee its occurrence.
Diagnosis
Uterine prolapse is usually diagnosed after a detailed history and a physical examination called the bimanual pelvic exam (where the patient’s vagina is observed).
Additionally, a speculum examination of the pelvis can be done that uses an instrument called a speculum to have a more detailed look.
Treatment of Uterine Prolapse
The treatment options for prolapse depend upon the level of disease, the severity of the symptoms, the patient’s future fertility plans, and the age of the patient. There are both conservative and surgical treatments present to treat uterine prolapse.3C. Aboseif and P. Liu, “Pelvic Organ Prolapse,” in StatPearls, Treasure Island (FL): StatPearls Publishing, 2023. Accessed: May 31, 2023. [Online]. Available: http://www.ncbi.nlm.nih.gov/books/NBK563229/
Conservative treatment includes pelvic floor muscle training and vaginal pessaries, whereas surgical intervention includes hysterectomy and many others.
Uterine Prolapse Exercises:
Kegel’s exercise is a conservative treatment option for uterine prolapse, generally implemented in the early stages of the disease. The exercise is performed to strengthen the pelvic muscles.4Y.-C. Huang and K.-V. Chang, “Kegel Exercises,” in StatPearls, Treasure Island (FL): StatPearls Publishing, 2023. Accessed: Jun. 01, 2023. [Online]. Available: http://www.ncbi.nlm.nih.gov/books/NBK555898/ To perform this exercise, squeeze your pelvic muscles for a few seconds and repeat multiple times. Hence, this exercise helps strengthen muscles easily and is inexpensive, time effective and doesn’t require any additional arrangements.
Heel slides, marches, happy baby poses, and diaphragmatic breathing are some other simple routine exercises to strengthen your pelvic floor muscles.
Vaginal Pessaries:
Vaginal pessaries are silicon-made U-shaped or doughnut-shaped devices inserted in the vagina to push up the dislocated uterus. It is a conservative treatment option for the later stages of the disease.5“Pelvic organ prolapse: Pelvic floor exercises and vaginal pessaries,” in InformedHealth.org [Internet], Institute for Quality and Efficiency in Health Care (IQWiG), 2018. Accessed: Jun. 01, 2023. [Online]. Available: https://www.ncbi.nlm.nih.gov/books/NBK525762/ Pessaries are very beneficial in treating uterine prolapse, and patients are more comfortable with it. Since they are artificial objects, regular hygiene maintenance is very necessary to prevent any infection.
Uterine Prolapse Surgery:
Surgery is often decided after a detailed patient history and lifestyle preferences, particularly sexual life and fertility.
Hysterectomy:
Hysterectomy is the surgical removal of the uterus. The surgery can be through the vaginal path or the abdomen. Vaginal hysterectomy is less invasive and complicated and has fewer risk factors. However, one drawback of hysterectomy is that patients can then never be pregnant.
Colpocleisis:
Colpocleisis is an obliterative, noninvasive surgical intervention in which the vaginal opening or vaginal canal is permanently closed. Closure of the vaginal canal can act as a support for the remaining pelvic floor muscles. Hence, elderly or sexually inactive patients usually prefer this option.
Uterine Sparing Surgery:
Uterine-sparing surgery is an alternative to hysterectomy and colpocleisis for patients interested in some future fertility plans. In this procedure, the uterus anatomy is not disturbed. Therefore, the chances of future pregnancies persist.
There are a few different uterine-sparing procedures available:
- Uterine Suspension Techniques: Uterine suspension procedures, such as uterosacral ligament suspension, aim to restore support to the uterus by reattaching the uterosacral ligaments to their normal position.6Jenkins VR 2nd. Uterosacral ligament fixation for vaginal vault suspension in uterine and vaginal vault prolapse. Am J Obstet Gynecol. 1997 Dec;177(6):1337-43; discussion 1343-4. doi: 10.1016/s0002-9378(97)70073-5. PMID: 9423733. This helps lift and hold the uterus in place, alleviating the prolapse while preserving the organ.
- Mesh-Augmented Repair: In some cases, a mesh or graft material can be used to reinforce the pelvic floor tissues and provide additional support to the uterus.7Kapur K, Dalal V. Mesh repair of vaginal wall prolapse. Med J Armed Forces India. 2014 Apr;70(2):105-10. doi: 10.1016/j.mjafi.2013.09.011. Epub 2014 Mar 12. PMID: 24843196; PMCID: PMC4017197. This can be done through various techniques, such as using mesh implants or grafts to strengthen the weakened ligaments or tissues. It’s important to note that while uterine-sparing surgery allows for the potential of future pregnancies, it may not be suitable for all patients. The decision to pursue uterine-sparing surgery should be made in collaboration with a healthcare professional, considering factors such as the severity of the prolapse, the patient’s overall health, and their specific fertility goals. Additionalit’sit’s crucial to discuss the potential risks, benefits, and long-term outcomes of the procedure before making a decision.
Uterine Prolapse Prevention
Although it is difficult to prevent prolapse, using the following measures can help lower the risk.
- Losing weight (if you are overweight),
- Doing Kegels exercises
- Having fiber-rich food
- Avoiding heavy weight lifting
- Treating constipation
- Quitting smoking
Conclusion
Uterine prolapse is the dissociation of the uterus from its usual position due to the weakening of pelvic floor muscles. Hence, the uterus ends up falling into the vaginal canal, sometimes even reaching the opening. The symptoms of uterine prolapse include urine urgency, painful sexual intercourse, vaginal bleeding, heaviness in the abdomen, etc. Both conservative and surgical treatment options are available to cure uterine prolapse. Kegel exercise is the most beneficial daily routine procedure that one can easily follow to strengthen their pelvic muscles. In extreme cases, surgery is an option.
Refrences
- 1C. J. Chen and H. Thompson, “Uterine Prolapse,” in StatPearls, Treasure Island (FL): StatPearls Publishing, 2023. Accessed: Jun. 01, 2023. [Online]. Available: http://www.ncbi.nlm.nih.gov/books/NBK564429/
- 2Doshani A, Teo RE, Mayne CJ, Tincello DG. Uterine prolapse. BMJ. 2007 Oct 20;335(7624):819-23. doi: 10.1136/bmj.39356.604074.BE. PMID: 17947787; PMCID: PMC2034734.
- 3C. Aboseif and P. Liu, “Pelvic Organ Prolapse,” in StatPearls, Treasure Island (FL): StatPearls Publishing, 2023. Accessed: May 31, 2023. [Online]. Available: http://www.ncbi.nlm.nih.gov/books/NBK563229/
- 4Y.-C. Huang and K.-V. Chang, “Kegel Exercises,” in StatPearls, Treasure Island (FL): StatPearls Publishing, 2023. Accessed: Jun. 01, 2023. [Online]. Available: http://www.ncbi.nlm.nih.gov/books/NBK555898/
- 5“Pelvic organ prolapse: Pelvic floor exercises and vaginal pessaries,” in InformedHealth.org [Internet], Institute for Quality and Efficiency in Health Care (IQWiG), 2018. Accessed: Jun. 01, 2023. [Online]. Available: https://www.ncbi.nlm.nih.gov/books/NBK525762/
- 6Jenkins VR 2nd. Uterosacral ligament fixation for vaginal vault suspension in uterine and vaginal vault prolapse. Am J Obstet Gynecol. 1997 Dec;177(6):1337-43; discussion 1343-4. doi: 10.1016/s0002-9378(97)70073-5. PMID: 9423733.
- 7Kapur K, Dalal V. Mesh repair of vaginal wall prolapse. Med J Armed Forces India. 2014 Apr;70(2):105-10. doi: 10.1016/j.mjafi.2013.09.011. Epub 2014 Mar 12. PMID: 24843196; PMCID: PMC4017197.





