What is Cervical Insufficiency?
According to the American College of Obstetricians and Gynecologists (ACOG), cervical insufficiency is characterized as the inability of the uterus to hold the fetus in the second or early third trimester of the pregnancy and expulsion of the live fetus in the absence of uterine contractions. It usually results in loss of pregnancy, which is a painful experience for the mother.
It is the most common cause of miscarriage and premature birth that remains neglected at first. However, the diagnosis is confirmed when it occurs in consecutive pregnancies. The incidence of cervical insufficiency in the general obstetric population is about 0.5 percent and 8-10 percent in patients with a previous history of miscarriage.1Thakur, M. (2022, December 17). Cervical insufficiency. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK525954/
How Does Cervical Insufficiency Occur?
The lower part of the uterus, called the cervix, opens into the vagina. Your cervix is made of fibrous and connective tissues. Fibrous parts provide strength to the cervix. The cervix is a dynamic anatomical structure that acts as a barrier between the fetus and the outer environment. During pregnancy, your cervix becomes strong due to collagen deposition that supports your pregnancy and does not allow your fetus to come out. However, collagen breaks at the time of parturition, and the cervix becomes soft and shorter to allow your fetus to come out.
Abnormal remodeling of the cervix results in preterm delivery of the fetus. It can be due to Mullerian duct abnormality or due to infections that cause early fetal loss.2Lotgering, F. (2007). Clinical aspects of cervical insufficiency. BMC Pregnancy and Childbirth, 7(Suppl 1), S17. https://doi.org/10.1186/1471-2393-7-s1-s17

Causes of Cervical Insufficiency
It most commonly affects you during the 2nd trimester and in the early third trimester. There can be multiple causes of cervical insufficiency. It can be congenital or acquired.
Congenital Cause:
Congenitally, cervical insufficiency is caused by abnormal development of the Mullerian duct. Euler-Danlos syndrome or Marfan syndrome can also cause cervical insufficiency. It is a syndrome of connective tissue disorder in which there is a defect in collagen formation, resulting in cervical incompetence.
Acquired Cause:
Acquired causes are those that happen to you after birth. These causes are:
- Cervical trauma is the most common acquired cause of cervical incompetence. It can occur during surgeries (dilatation and curettage, cervical damage during childbirth, and cervical conization).
- A bacterial, viral, or fungal infection that induces inflammation of the cervix, resulting in cervical incompetence.
Who is at Risk for Cervical Insufficiency?
Cervical incompetence can occur at any age, but some factors tell you whether you are at risk of having cervical insufficiency or not. These risk factors are:
Previous Surgery:
Patients with previous surgeries in which the part of the cervix is removed for diagnostic or therapeutic purposes (trachelectomy and biopsy) are at higher risk for cervical insufficiency than others. Cervical trauma can also occur during surgeries like dilatation and curettage (a surgery in which the cervix is opened and fetal parts are removed with the help of instruments). Patients with a history of dilatation and curettage are at higher risk for cervical incompetence. Therefore, regular follow-up and monitoring are necessary to observe the length of the cervix.
Previous History of Emergency C-section:
In case of an emergency C-section during the second or early third trimester, damage to the upper part of the cervix can occur during birth, which increases your risk for cervical insufficiency.3Meng, L., Öberg, S., Sandström, A., Wang, C., & Reilly, M. (2022). Identification of risk factors for incident cervical insufficiency in nulliparous and parous women: a population-based case-control study. BMC medicine, 20(1), 348. https://doi.org/10.1186/s12916-022-02542-7
Connective Tissue Abnormalities:
If you have been born with connective tissue disorder like Marfan syndrome or Ehler-Danlos syndrome, you might have cervical insufficiency because collagen deposition strengthens your cervix. The cervix becomes soft and short without collagen, resulting in cervical insufficiency.
Abnormal Uterus Structure:
Uterus abnormalities usually do not affect the cervical length but can be the cause of preterm birth or fetal loss.
Exposure to Diethylstilbestrol:
Women who are taking diethylbestrol during pregnancy are at higher risk of preterm birth than others.
Genetics:
People with a positive family history of cervical insufficiency are at greater risk for preterm birth than others.
Multiple Pregnancies:
There are some studies indicating that females experiencing twin pregnancies or triplets are more prone to cervical incompetence.4Weak cervix (cervical incompetence or cervical insufficiency). (n.d.). Tommy’s. https://www.tommys.org/pregnancy-information/pregnancy-complications/cervical-incompetence
Signs & Symptoms of Cervical Insufficiency
It is very difficult to diagnose cervical insufficiency. However, there are some signs and symptoms that help your doctor to reach the diagnosis. These:
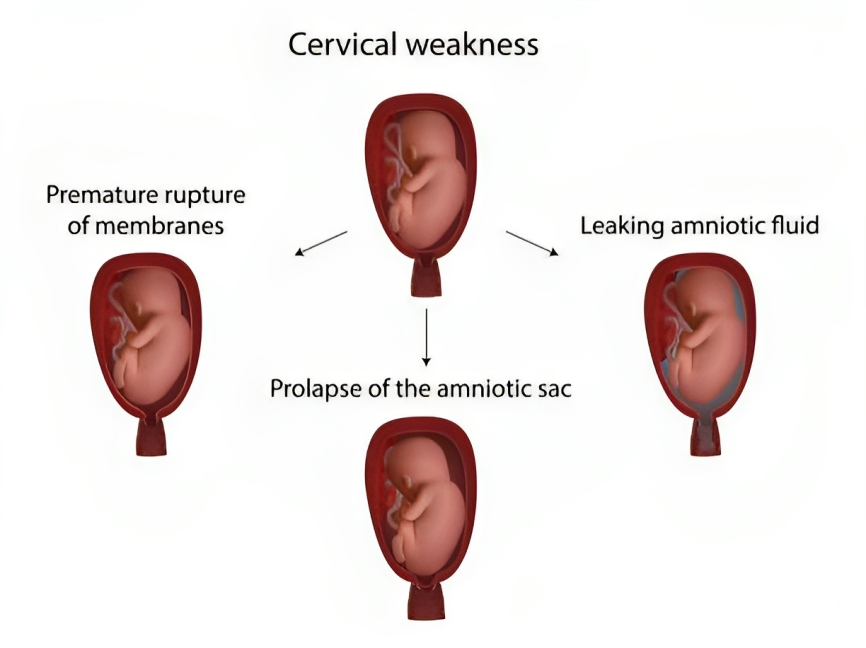
- Preterm premature rupture of the membrane (PPROM)
- Painless cervical dilation
- The presence of fetal membrane during the examination in the second or early third trimester of the pregnancy
Most of the females remain asymptomatic during the early pregnancies. However, the symptoms of cervical insufficiency are:
- Backache (Pain in the lower back)
- Discharge coming out from the vagina with an increase in volume
- Feeling pressure in the pelvic area
- Stomach or abdominal discomfort leading to cramps
- Light bleeding per vagina
How to Diagnose Cervical Insufficiency?
The diagnosis of cervical insufficiency is challenging because of poor objective findings. It depends upon a complete history, physical examination, laboratory, and radiological investigations.
History:
A complete history of the patient is compulsory to reach the diagnosis. Because cervical insufficiency remains undiagnosed in early pregnancy, during complete history, some questions should be asked. These are:
- Do you have any history of previous surgery?
- Any history of a previous miscarriage?
- Positive family history
- Any genetic abnormality?
- Medical history
- Type of discharge coming out of the vagina?
- The color and smell of the discharge
Physical Examination:
After taking a history, your doctor will examine you physically. During the examination, a speculum is used which reveals preterm premature rupture of the membrane (PPROM), and shortening of the cervix.
Your doctor will examine your abdomen and pelvis to check for tenderness, solid mass or Adnexa, and any previous surgery marks.
Laboratory Investigations
Laboratory investigation is usually not required but can be advised to rule out systemic infections. It includes:
- Complete blood count (CBC) to check for anemia
- White blood cell count (WBCs): Neutrophils are raised in case of bacterial infection, and lymphocytes are raised in viral infection
- Amniocentesis to check the infection status of the patient
- Cultural and sensitivity of the discharge coming out from the vagina
- Urine examination
Radiological Investigations:
Radiological investigations are the best modalities to screen and diagnose cervical insufficiency. It includes ultrasound.
Ultrasonography
Ultrasonography is the best possible way to diagnose cervical insufficiency. A transvaginal ultrasound at the gestational age of 15-16 weeks is more accurate than a transabdominal ultrasound. The transvaginal ultrasound findings in patients with cervical insufficiency are:
- Shortening of the cervical length (<2.5 cm)
- Cervical dilation
- Presence of fetal membrane
In asymptomatic patients with a previous history of preterm birth, doctors advise a serial transvaginal ultrasound screening at 16 weeks of gestation, followed by intervals of 2 weeks until 26-28 weeks.5Dulay, A. T. (2023, November 12). Cervical insufficiency. MSD Manual Professional Edition. https://www.msdmanuals.com/professional/gynecology-and-obstetrics/abnormalities-of-pregnancy/cervical-insufficiency
Fetal Fibronectin Testing:
Fibronectin is a glycoprotein that is produced by the fetus. It is an adhesive material present at the interface of chorion and decidual cells. Normally, very low levels of this protein are present. Patients with a high level of fibronectin in the vaginal fluid after 22 weeks of pregnancy are at higher risk of preterm birth. Therefore, fibronectin testing is important in patients with a history of recurrent fetal loss.6Mba, E. R. N. M. P. (n.d.). Cervical Insufficiency WorkUp: approach considerations, ultrasonography, fetal fibronectin testing. https://emedicine.medscape.com/article/1979914-workup#c9?form=fpf
How to Treat Cervical Insufficiency?
There are surgical and non-surgical options to treat cervical insufficiency. Surgical treatment is considered to be recommended to treat cervical insufficiency.
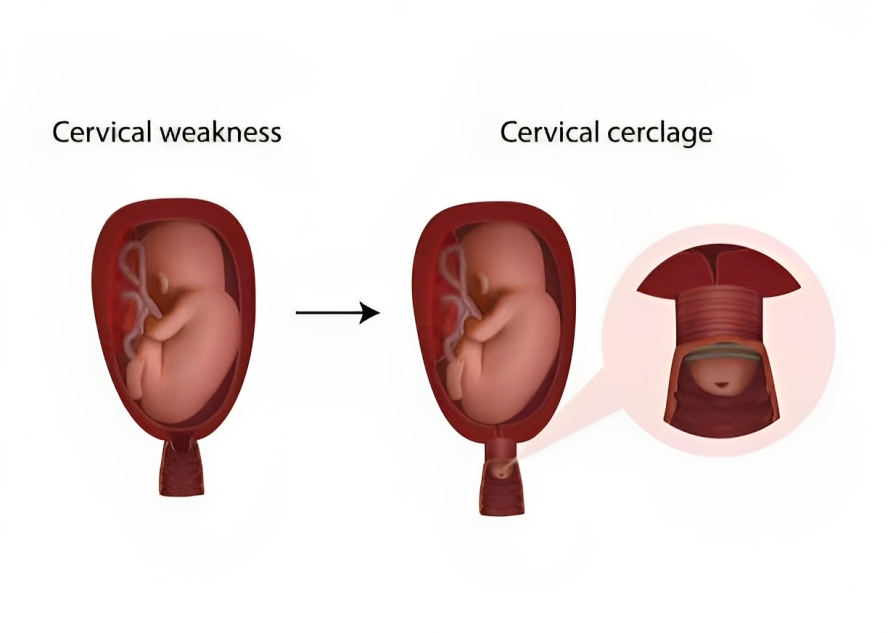
Cervical Cerclage:
Cervical cerclage is a surgical procedure that enhances the tensile strength of the cervix to support the pregnancy. This procedure can be performed through transvaginal and transabdominal approaches. The main objective of each technique is to strengthen the cervix at the level of internal os, and it is removed before normal delivery. The transvaginal approach is considered to be best for cerclage.
Transvaginal Cerclage:
There are two types of transvaginal approaches. These are:
1. Mcdonald Transvaginal Cervical Cerclage
In this approach, the cerclage is placed at the level of a cervicovaginal junction without bladder mobilization.
2. Shirodkar Transvaginal Cervical Cerclage
It is a high transvaginal cerclage in which strings are placed at the level of the Cardinal ligament by mobilizing the bladder.
Transabdominal Cervical Cerclage:
Transabdominal cerclage is placed at the level of the internal cervical OS before pregnancy.7Cervical insufficiency. (2019, October 22). Yale Medicine. https://www.yalemedicine.org/conditions/cervical-insufficiency#:~:text=%E2%80%A2A%20condition%20in%20pregnancy,%2C%20and%20surgery%20(cervical%20cerclage)
Indications of Cervical Cerclage
According to the American College of Gynecology and Obstetricians (ACOG), there are some indications of cervical cerclage. These include the following:
- Previous history of pregnancy loss in 2nd trimester or cerclage placement (prophylactic cerclage before pregnancy)
- Painless dilation of the cervix in 2nd trimester of the pregnancy (emergency cerclage)
- History of preterm birth with short cervical length (ultrasound-indicated cerclage)
Preoperative evaluation of the cervix and fetus is advised to avoid any complications.
Nonsurgical Management of Cervical Insufficiency
In a non-surgical approach, supplementation of progesterone is suitable in patients with a history of recurrent preterm birth. Your gynecologist will advise progesterone at the gestational age of 16-25 weeks till 36 weeks of pregnancy. It has reduced the risk of preterm deliveries. In women with no history of preterm birth and shorter cervical length, intravaginal progesterone is suitable to reduce the risk of preterm birth.
Cervical Pessaries:
Cervical pessaries are the noninvasive treatment options for cervical insufficiency. The pessaries aim to shift the weight of the fetus away from the cervix.
What are the complications of cervical insufficiency?
If cervical incompetence remains neglected, it can cause complications. These are:
- Preterm birth
- Fetal death
- Psychological impairments
How can you Prevent Cervical Insufficiency?
You can never prevent your cervical insufficiency, but you can make your pregnancy healthy by following:
Healthy Diet:
During pregnancy, you need more vitamins and nutrients to maintain your pregnancy. A healthy diet plan will help you to support the pregnancy.
Avoid Harmful Substances:
Avoid harmful substances such as smoking and alcohol because these substances affect your pregnancy.
Regular Follow-up for Prenatal Care:
A regular follow-up is necessary to check the viability of the fetus and to evaluate other abnormalities.
Gain Weight Wisely:
The target weight gain during the pregnancy is about 11-13 Kg. Gaining weight wisely will help your child to grow because obesity will affect the growth of your child.
Septate Uterus Vs. Cervical Insufficiency
The Septate uterus is a congenital Mullerian duct abnormality in which a membrane halves the uterus into two parts. In the septate uterus, there are two uterine cavities instead of one. On the other hand, in cervical insufficiency, there is only one uterine cavity, and dilatation of the cervix without uterine contractions causes this problem.
Can I Exercise with a Shorter Cervix?
Usually, your doctor advises you to take bed rest during pregnancy. It is best to avoid strenuous exercise because a shorter cervix cannot withstand the pressure, and it opens during strenuous activities. Your doctor may also advise avoiding long-standing positions affecting the shorter cervix.8Lotgering F. K. (2007). Clinical aspects of cervical insufficiency. BMC pregnancy and childbirth, 7 Suppl 1(Suppl 1), S17. https://doi.org/10.1186/1471-2393-7-S1-S17
Is the Removal of the Cerclage Painful?
No, cerclage removal does not cause a lot of pain. Your doctor can perform it in the outpatient department and remove your stitches.
Conclusion
To conclude, this is a condition in which your uterus can not hold the fetus in the second or third trimester and pushes the fetus out without uterine contractions. It is the most common cause of premature birth and miscarriages among fertile females. Patients with positive history, surgery, and trauma are at greater risk than others. Cervical cerclage or transvaginal cerclage can effectively manage this condition. Before delivery, do not forget to mention it to your gynecologist if you had cerclage during the second or third trimester of pregnancy.
Refrences
- 1Thakur, M. (2022, December 17). Cervical insufficiency. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK525954/
- 2Lotgering, F. (2007). Clinical aspects of cervical insufficiency. BMC Pregnancy and Childbirth, 7(Suppl 1), S17. https://doi.org/10.1186/1471-2393-7-s1-s17
- 3Meng, L., Öberg, S., Sandström, A., Wang, C., & Reilly, M. (2022). Identification of risk factors for incident cervical insufficiency in nulliparous and parous women: a population-based case-control study. BMC medicine, 20(1), 348. https://doi.org/10.1186/s12916-022-02542-7
- 4Weak cervix (cervical incompetence or cervical insufficiency). (n.d.). Tommy’s. https://www.tommys.org/pregnancy-information/pregnancy-complications/cervical-incompetence
- 5Dulay, A. T. (2023, November 12). Cervical insufficiency. MSD Manual Professional Edition. https://www.msdmanuals.com/professional/gynecology-and-obstetrics/abnormalities-of-pregnancy/cervical-insufficiency
- 6Mba, E. R. N. M. P. (n.d.). Cervical Insufficiency WorkUp: approach considerations, ultrasonography, fetal fibronectin testing. https://emedicine.medscape.com/article/1979914-workup#c9?form=fpf
- 7Cervical insufficiency. (2019, October 22). Yale Medicine. https://www.yalemedicine.org/conditions/cervical-insufficiency#:~:text=%E2%80%A2A%20condition%20in%20pregnancy,%2C%20and%20surgery%20(cervical%20cerclage)
- 8Lotgering F. K. (2007). Clinical aspects of cervical insufficiency. BMC pregnancy and childbirth, 7 Suppl 1(Suppl 1), S17. https://doi.org/10.1186/1471-2393-7-S1-S17





