Chikungunya is a viral disease transmitted to humans by infected mosquitoes. It is a major health concern in several parts of the world, including Asia, America, and Africa, where outbreaks occur sporadically. While it shares symptoms like fever and joint pain with other mosquito-borne illnesses, such as dengue, chikungunya stands out for the severe joint pain it can cause, which can last for months but is rarely fatal.
Causes of Chikungunya
Chikungunya is prevalent in many parts of the world, including Asia, Africa, Europe, North and South America, and in islands in the Indian and Pacific Oceans.1Diop, D., G. Meseznikov, and M. Sanicas. “Chikungunya outbreaks from 2000 to 2015: a review.” MOJ Public Health 2.6 (2015): 181-187. Specifically, it was first reported from Tanzania in 1952–53 and spread to sub-Saharan Africa, Southeast Asia, and the Pacific, causing large epidemics.2Sudeep, A. B., and D. Parashar. “Chikungunya: an overview.” Journal of Biosciences 33.4 (2008): 443-449.
This viral disease is caused by the chikungunya virus (CHIKV), which belongs to the Togaviridae family, Alphavirus. Chikungunya virus (CHIKV) is an alphavirus transmitted by mosquitoes, mostly Aedes aegypti and Aedes albopictus.3Simon, Fabrice, et al. “Chikungunya virus infection.” Current infectious disease reports 13 (2011): 218-228 The word “chikungunya” comes from the Kimakonde language, meaning “to become contorted,” referring to the stooped posture of patients due to severe joint pain.
Spread & Transmission of Chikungunya
As mentioned earlier, chikungunya is a mosquito-borne viral disease primarily transmitted through the bite of infected mosquitoes. The primary cause of its spread is directly linked to the transmission by the bite of specific mosquito species, Aedes aegypti and Aedes albopictus. These mosquitoes also transmit other arboviruses, such as dengue and Zika.

Mosquito Vector: Aedes Aegypti
Aedes aegypti is linked to the main spread of the virus. This mosquito species thrives in urban environments, particularly tropical and subtropical regions. These mosquitoes breed in small collections of clean water found in household objects like flowerpots, discarded tires, containers, and gutters. Aedes aegypti is a day-biting mosquito whose activity is concentrated in the morning or afternoon. Moreover, these mosquitoes feed on human blood, which makes human populations the primary reservoir for the virus. If an infected person is bitten, the virus is transmitted to the mosquito, which can then spread it to others.
Mosquito Vector: Aedes Albopictus
Aedes albopictus, commonly known as the “Asian tiger mosquito,” is another key vector for chikungunya transmission. This species is more resilient than Aedes aegypti, as it can survive in cooler climates. This mosquito is not limited to urban areas, making urban and rural areas equally susceptible to the disease. Aedes albopictus, like Aedes aegypti, is a day-biting mosquito.
Transmission Cycle
Human-Mosquito-Human Transmission in Chikungunya
The most common transmission cycle is mosquito to human bite. People infected with the chikungunya virus have high enough virus levels in their blood (viremia) during the first few days of illness to transmit the virus to mosquitoes. This cycle involves an infected person who is bitten by a mosquito, which then becomes infected and can transmit the virus to other people through its bite.
The virus is not spread from person to person or through coughing, sneezing, or touching.
Pregnancy & Breastfeeding
Rarely chikungunya can spread from mothers to newborn babies. The chikungunya epidemic that occurred on La Reunion Island revealed for the first time the possibility of mother-to-child transmission in the perinatal period with a high rate of morbidity. If the pregnant woman is infected at the time of delivery, then the child can develop severe morbidity. Usually, the mean interval between the onset of maternal illness and the onset of neonate illness is five days (range 3-9 days).4Ramful, Duksha, et al. “Mother-to-child transmission of Chikungunya virus infection.” The Pediatric Infectious Disease Journal 26.9 (2007): 811-815.
Studies have shown that breast milk does not carry the chikungunya virus. To date, there are no reports of infants being infected by breastfeeding.
Symptoms of Chikungunya
Symptoms of chikungunya usually appear 4-8 days after being bitten by an infected mosquito. Even though symptoms may appear in some people as early as day two and as late as day 12, the illness can occur as a sudden onset of fever and malaise accompanied by joint pain. The hallmark symptoms of chikungunya are fever and joint pain. Below are some of the common and rare symptoms of chikungunya.
Acute phase Symptoms:
High-Grade Fever
The first and foremost symptom is the sudden onset of high-grade fever, often more than 39C (102 F).5Borgherini, Gianandrea, et al. “Outbreak of chikungunya on Reunion Island: early clinical and laboratory features in 157 adult patients.” Clinical infectious diseases 44.11 (2007): 1401-1407. The fever typically subsides within a week and may be biphasic, meaning it can subside and then recur after a brief period.
Arthralgia or Joint Pain
Severe joint pain can occur in the hands, wrists, feet, and ankles. The pains are symmetrical; that is, they affect both sides equally. The pain can sometimes be so severe that it can limit mobility and can lead to a stooped posture. Joint pain can last for a few days to a few weeks, depending on the severity of the condition. In severe cases, the pain can be prolonged to a few months or even years, mimicking rheumatoid arthritis.6Suhrbier, Andreas. “Rheumatic manifestations of chikungunya: emerging concepts and interventions.” Nature Reviews Rheumatology 15.10 (2019): 597-611.
Headache
Headaches are commonly reported in the acute phase of chikungunya. Some patients may even complain of photophobia (sensitivity to light).
Myalgia or Muscle Pain
Muscle pain is also a common symptom of chikungunya and can affect various muscle groups. The combination of muscle and joint pain contributes to the feeling of general malaise and fatigue during the disease.
General Malaise & Fatigue
Moreover, severe tiredness has been reported in patients with chikungunya. The fatigue may persist even after the other acute symptoms have been resolved. This can lead to a delay in full recovery.
Rash
A rash can occur on the patient’s face, trunk, and limbs. It can be maculopapular, with both flat and raised red lesions, or petechial, with pinpoint non-blanching spots measuring less than 2 mm in size. The rash can affect the skin and mucosa.

Gastrointestinal Symptoms:
Nausea and vomiting are some of the rare symptoms of chikungunya, and they are usually observed in children.
Chronic Phase Symptoms:
In some patients, the disease can be prolonged in newborns or in adults over 65 years who have other underlying health issues like hypertension and diabetes.
Persistent Joint Pain
Chronic joint pain may last from three months to a few years. Its long-term effects can resemble inflammatory arthritis. The most commonly affected joints are the hands, ankles, and knees.

Chronic Fatigue
Persistent fatigue can deteriorate the quality of life of the patient. Fatigue, in combination with joint and muscle pain, can have detrimental effects, especially in patients who have diabetes or are suffering from cardiovascular disease.
Neurological Symptoms:
In rare cases, chikungunya can cause neurological complications such as encephalitis, meningitis, and Guillain-Barré syndrome.77.Lebrun, Gaëtan, et al. “Guillain-Barré syndrome after chikungunya infection.” Emerging infectious diseases 15.3 (2009): 495. Studies have reported cases of cognitive dysfunction, memory loss, and mood disorders following infection.
Atypical Symptoms & Complications:
Although rare, Chikungunya can develop severe symptoms in newborn babies and the elderly and in individuals with co-morbidity.
Neurological Complications
Complications like encephalitis, seizures, and confusion have been observed in newborns under the age of 2 months and in the elderly.
Cardiovascular Complications
Heart conditions usually occur in patients with preexisting heart issues. Myocarditis (inflammation of the heart muscle), pericarditis, and acute heart failure have been observed.
Ocular Symptoms:
Conjunctivitis (inflammation of the conjunctiva) and photosensitivity are common in the acute phase of the disease, but uveitis (inflammation inside the eye), retinitis (inflammation of the retina), and optic neuritis (swelling of the optic nerve) have been reported in a small percentage of cases, leading to vision disturbances.
Although fatalities due to chikungunya are rare, the disease can cause severe complications in newborns, older adults, and individuals with underlying health conditions.
Diagnosis of Chikungunya
Correctly diagnosing chikungunya is necessary, especially in areas with prevalent mosquito-borne diseases like chikungunya, Zika, and dengue. All these diseases have different complications and treatment protocols. Below, we outline the key steps and methods used in diagnosing chikungunya.
Clinical Diagnosis:
Chikungunya is often suspected in areas where the disease is endemic. Typically, a physician begins by reviewing the patient’s medical history, symptoms, and travel history.
However, clinical diagnosis alone can be challenging because chikungunya shares many common symptoms with other arboviral infections. Therefore, laboratory confirmation tests are important.
Laboratory Tests:
Specific laboratory tests are available to detect the chikungunya virus.
RT-PCR (Reverse Transcriptase-Polymerase Chain Reaction) Test:
This is the golden standard test for early diagnosis of chikungunya. It detects the viral RNA and is highly specific and sensitive. RT-PCR is the test of choice, especially for pregnant women, infants, and the elderly.8Edwards, T., Del Carmen Castillo Signor, L., Williams, C., Larcher, C., Espinel, M., Theaker, J., Donis, E., Cuevas, L. E., & Adams, E. R. (2017). Analytical and clinical performance of a Chikungunya qRT-PCR for Central and South America. Diagnostic microbiology and infectious disease, 89(1), 35–39. https://doi.org/10.1016/j.diagmicrobio.2017.06.001
Serological Tests:
Serological tests are used to detect antibodies produced by the immune system in response to chikungunya virus. These tests are useful in detecting the virus at later stages when the PCR test is not effective.
Enzyme-Linked Immunosorbent Assay (ELISA)
IgM antibodies can be detected in blood 3-8 days after the onset of the infection. ELISA is the most reliable procedure for diagnosing chikungunya.
IgG Antibody Detection
IgG antibodies are usually detected later, around 10-14 days after the onset of the infection. It is useful for detecting past illness but is not a very good tool for detecting acute illness.
Plaque Reduction Neutralization Test (PRNT)
PRNT is another more advanced test for diagnosing chikungunya. It is more specific and measures the ability of the patient’s serum to neutralize the virus in a laboratory setting. This test is less commonly used as it is time-consuming and requires advanced facilities.
Diagnosing chikungunya requires a combination of clinical assessment and laboratory testing. PCR is the gold standard for early diagnosis, especially during the acute phase of the illness, while serological tests are useful in the later stages.
Treatment of Chikungunya
Currently, there is no specific antiviral treatment available for chikungunya. Treatment is mostly palliative, focusing on symptoms like fever and joint pain. The treatment plan can be as follows.
Rest & Hydration
Adequate rest and keeping the patient hydrated are necessary for improving symptoms. Oral Rehydration Solutions (ORS) or intravenous fluids can be given for hydration. Dehydration exaggerates symptoms of fatigue and muscle pain.
Fever & Pain Management
Paracetamol (Acetaminophen) is the first drug of choice for treating fever and pain. Doctors prefer paracetamol over nonsteroidal anti-inflammatory drugs (NSAIDs) in the early stages of chikungunya due to the risk of hemorrhagic complications, which are more common with dengue.
Once dengue is ruled out, NSAIDs can also be administered, like ibuprofen and naproxen, for severe joint pain.
Lastly, corticosteroids can be administered. They are not the drug of choice in the acute phase of chikungunya. However, when patients experience severe, chronic joint pain or inflammation that does not respond to NSAIDs, doctors may prescribe a short course of low-dose corticosteroids under close medical supervision.9Sharma, Shweta, et al. “A comparative study of short course corticosteroids v/s NSAIDS in debilitating post-chikungunya arthritis.” J Ind Acad Clin Med. 19.2 (2018): 102-5.
Supportive care
Although chikungunya is self-limiting, certain populations are at a higher risk of developing complications, like infants, the elderly, people with co-morbidity, and pregnant ladies. Continuous monitoring of this high-risk group is important. A complete evaluation of neurological and cardiovascular symptoms should be done.
Chikungunya Vaccination
A live attenuated chikungunya vaccine (manufactured by Valneva as IXCHIQ) is the only chikungunya vaccine currently licensed in the United States. This vaccine was approved by the Food and Drug Administration (FDA) in November 2023.10Valneva SE. (n.d.). Chikungunya. Retrieved October 2, 2024, from https://valneva.com/research-development/chikungunya/
Prevention of Chikungunya
Since there is no antiviral treatment for chikungunya, prevention is the most effective strategy for reducing the spread of the virus. The following are some tips for preventing infection.

- Elimination of breeding grounds of mosquitoes by ensuring proper water disposal and continuously draining water accumulation sites.
- Fogging and insecticides have proven useful in areas where chikungunya is endemic. Consequently, communities often implement campaigns during outbreak periods.
- Wear full protective clothing to reduce exposed areas for mosquito bites.
- Experts recommend applying mosquito repellent for individuals living in or traveling to chikungunya-endemic regions.
- Choose indoor lodging with air conditioning and closed doors and windows. If sitting or sleeping in the open air, wear a net to protect against mosquitoes.
Differential Diagnosis
Chikungunya shares its symptoms with similar diseases, such as dengue and Zika. Here’s a detailed comparison table between them.
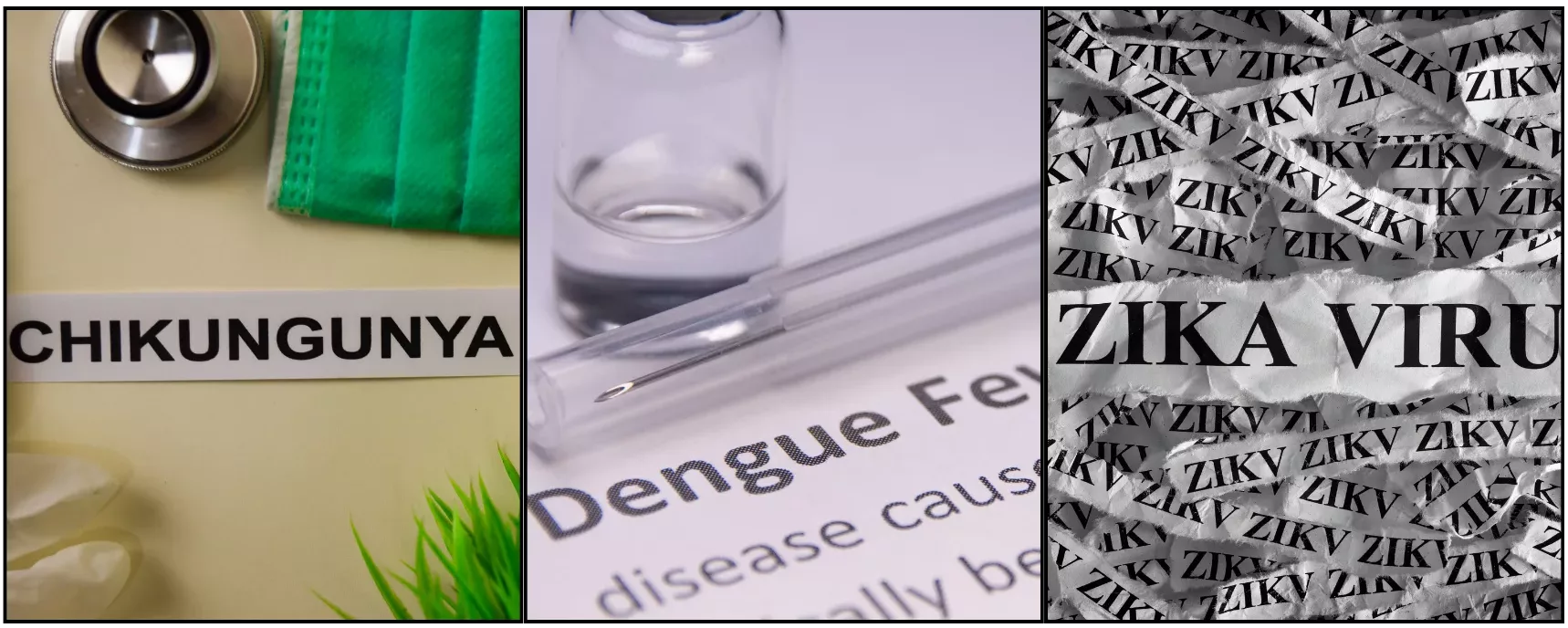
| Aspects | Chikungunya | Dengue | Zika |
| Virus | Chikungunya virus (CHIKV) | Dengue virus (DENV, types 1-4) | Zika virus (ZIKV) |
| Mode of Transmission | Aedes aegypti and Aedes albopictus mosquitoes | Aedes aegypti and Aedes albopictus mosquitoes | Aedes aegypti and Aedes albopictus mosquitoes, also sexually transmitted |
| Incubation Period
(Days) |
2-7 | 4-10 | 3-14 |
| Primary Symptoms | Sudden high fever, severe joint pain (arthralgia), headache, rash, muscle pain | High fever, severe headache, pain behind eyes, muscle and joint pain, rash, bleeding | Mild fever, rash, joint pain, conjunctivitis (red eyes), muscle pain |
| The Severity of Joint Pain | Severe | Moderate | Mild to moderate |
| Rash | Maculopapular rash and petechial rash, usually in early stage | Maculopapular rash, typically appears later in disease | Fine maculopapular rash, usually appears early |
| Treatment | Symptomatic (pain relief, hydration, rest) | Symptomatic (pain relief, hydration, monitoring for bleeding). NSAIDs not recommended | Symptomatic (pain relief, hydration, rest); avoid NSAIDs |
| Mortality | Low | It can be high due to hemorrhagic fever or shock | Very low |
Conclusion
Chikungunya is characterized by a broad range of symptoms, the most prominent being fever, joint pain, and rash. While many patients recover within weeks, the disease can lead to prolonged joint pain and fatigue, particularly in older adults or those with pre-existing health conditions. Early diagnosis and supportive care is crucial for management of this disease.
Refrences
- 1Diop, D., G. Meseznikov, and M. Sanicas. “Chikungunya outbreaks from 2000 to 2015: a review.” MOJ Public Health 2.6 (2015): 181-187.
- 2Sudeep, A. B., and D. Parashar. “Chikungunya: an overview.” Journal of Biosciences 33.4 (2008): 443-449.
- 3Simon, Fabrice, et al. “Chikungunya virus infection.” Current infectious disease reports 13 (2011): 218-228
- 4Ramful, Duksha, et al. “Mother-to-child transmission of Chikungunya virus infection.” The Pediatric Infectious Disease Journal 26.9 (2007): 811-815.
- 5Borgherini, Gianandrea, et al. “Outbreak of chikungunya on Reunion Island: early clinical and laboratory features in 157 adult patients.” Clinical infectious diseases 44.11 (2007): 1401-1407.
- 6Suhrbier, Andreas. “Rheumatic manifestations of chikungunya: emerging concepts and interventions.” Nature Reviews Rheumatology 15.10 (2019): 597-611.
- 77.Lebrun, Gaëtan, et al. “Guillain-Barré syndrome after chikungunya infection.” Emerging infectious diseases 15.3 (2009): 495.
- 8Edwards, T., Del Carmen Castillo Signor, L., Williams, C., Larcher, C., Espinel, M., Theaker, J., Donis, E., Cuevas, L. E., & Adams, E. R. (2017). Analytical and clinical performance of a Chikungunya qRT-PCR for Central and South America. Diagnostic microbiology and infectious disease, 89(1), 35–39. https://doi.org/10.1016/j.diagmicrobio.2017.06.001
- 9Sharma, Shweta, et al. “A comparative study of short course corticosteroids v/s NSAIDS in debilitating post-chikungunya arthritis.” J Ind Acad Clin Med. 19.2 (2018): 102-5.
- 10Valneva SE. (n.d.). Chikungunya. Retrieved October 2, 2024, from https://valneva.com/research-development/chikungunya/