Colectomy is a surgical procedure that is done to treat various grave digestive tract conditions like diverticulitis, inflammatory bowel disease (IBD), and colon cancer. The large intestine, also known as the colon, plays a crucial role in the digestive system by absorbing water, forming stool, and eliminating waste from the body. When serious medical conditions affect the colon, surgical intervention may be necessary.
What is Colectomy?
A colectomy is a surgical procedure in which all or part of the colon is removed to treat various digestive disorders. This procedure is commonly performed for colon cancer, inflammatory bowel disease (IBD), diverticulitis, bowel obstructions, and certain hereditary conditions like familial adenomatous polyposis (FAP). The extent of colon removal depends on the severity and location of the disease.1National Cancer Institute. Colectomy. In: NCI Dictionary of Cancer Terms [Internet]. Available from: https://www.cancer.gov/publications/dictionaries/cancer-terms/def/colectomy.
During a colectomy, the surgeon removes the affected portion of the colon and either reconnects the remaining healthy sections or creates an ostomy (an external opening for waste elimination) if reconnection is not possible. The approach may vary, with options including open surgery or minimally invasive laparoscopic techniques, depending on the patient’s condition and medical history.
Indications of Colectomy
The indications of colectomy include:
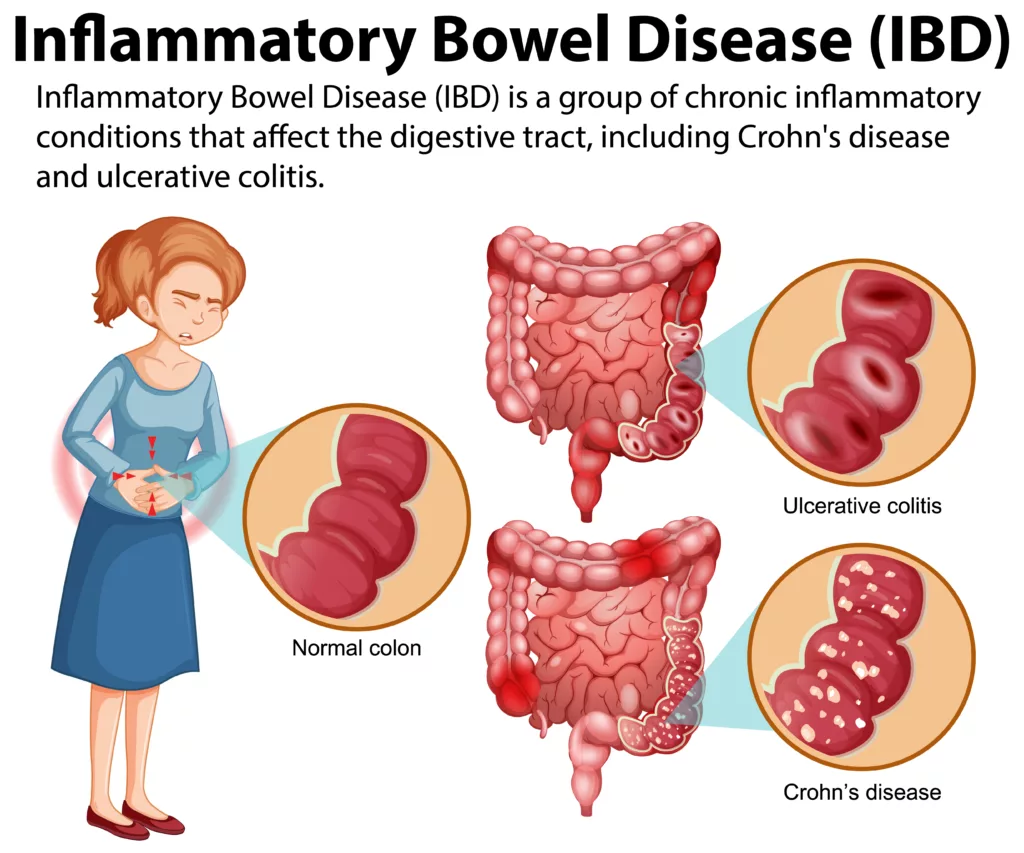
Inflammatory Bowel Disease (IBD)
In inflammatory bowel disease (IBD), there are ulcers and inflammations in the digestive tract. IBD encompasses diseases like Crohn’s disease and Ulcerative Colitis.
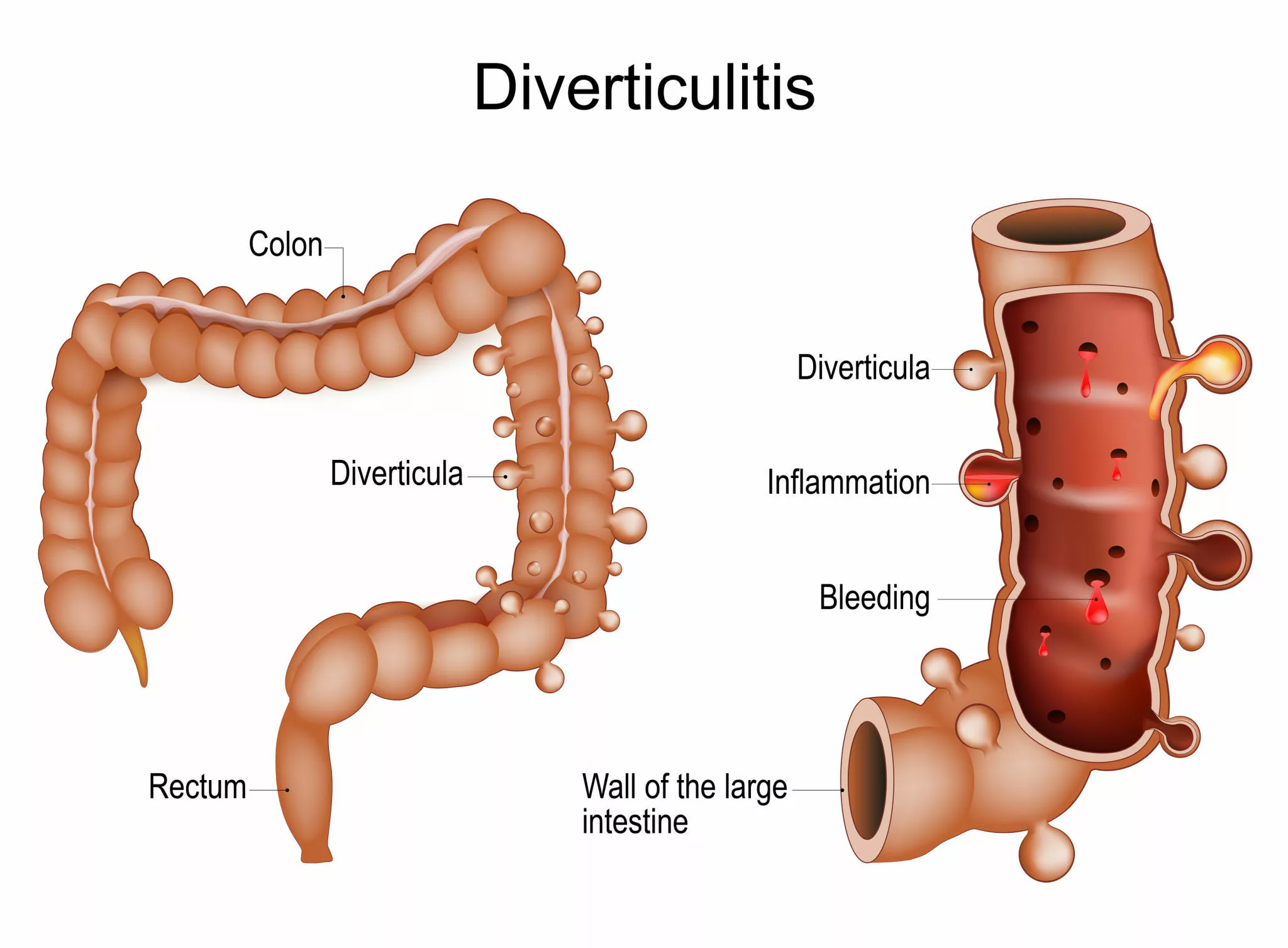
Diverticulitis
There are small pouches in the walls of your colon called diverticula. When these small pouches get inflamed, the condition is called diverticulitis. It can cause abdominal pain, bloating, and frequent changes in bowel habits.
Polyps
Polyps are the small benign growths on the colon. Most colon polyps are harmless, but some have the potential to develop into cancer.2Ozgur, I., Liska, D., Cengiz, T. B., Sapci, I., Valente, M. A., Holubar, S. D., Steele, S. R., Bhatt, A., & Gorgun, E. (2022). Colectomy for polyps is associated with a high risk for complications and low risk for malignancy: Time for endoluminal surgery?. American journal of surgery, 223(3), 463–467. https://doi.org/10.1016/j.amjsurg.2021.11.030 With the advancement in age, the chances of polyp formation increase.
Ischemic Colitis
Ischemic colitis is a condition in which blood supply to the colon is compromised. This is a serious condition which requires colectomy.
Contraindications of Colectomy
It is very important to know and understand when not to choose colectomy as the treatment option. Contraindications are classified as absolute or relative, depending on the risks involved:
Absolute Contraindications:
Surgery should not be performed if the risks outweigh the benefits. Patients with extensive comorbidities or widespread metastatic disease with an asymptomatic primary tumor may not benefit from colectomy and should avoid the procedure.
Relative Contraindications:
Some patients may face significant challenges in recovery due to psychological issues or lack of social support. If a patient cannot manage post-operative care independently, colectomy may not be a feasible option. Other relative contraindications include:
- Old Age reduces the ability of the human body to cope with changes and alterations. Therefore, doctors think twice before choosing it as the treatment of choice.
- Coagulopathy is yet another contraindication. Patients who actively consume anticoagulant medications need proper attention during surgeries because such patients may have excessive bleeding. during surgery.
- Patients suffering from cardiovascular diseases may not be able to go through the surgery. The doctor has to take into consideration all the pros, cons, and risks before opting for colectomy.
- Uncontrolled diabetes first needs to be controlled, otherwise it may lead to post-operative complications.
- Poor immunity may be due to autoimmune diseases like AIDS. In such cases, colectomy may not be performed.
Types of Colectomy
There are various types of colectomies, each focused on a particular portion of the colon:
-
Total Colectomy:
This procedure involves removing the entire colon at once. It is typically performed in cases of familial adenomatous polyposis, severe inflammatory bowel disease, or extensive colon damage.
-
Subtotal or Partial Colectomy:
If only a part of the colon is damaged, surgeons perform a partial colectomy. This approach is less intrusive and has a quicker recovery time compared to a total colectomy. Different kinds of partial colectomies are done according to where the afflicted area is located.
The main aim of the colectomy is to remove the damaged area of the colon and preserve the healthier tissue as much as possible. The colon’s remaining ends are often rejoined after excision to allow for regular digestion.
-
Sigmoid Colectomy:
Sigmoid colectomy is a variation on partial colectomy, where just the sigmoid colon (the last part) of your intestine gets taken out.3Lettieri, P. R., Kunac, A., Oliver, J. B., & Anjaria, D. J. (2022). Sigmoid Colectomy for Sigmoid Volvulus Through a Limited Left Lower Quadrant Transverse Laparotomy Incision Without Laparoscopy. The American surgeon, 88(9), 2233–2234. https://doi.org/10.1177/00031348221093530 This treatment is widely used on patients with diverticulitis and even colon cancer in some cases. Compared with a whole colectomy, sigmoid colectomy is also relatively more focused in that part of the colon remains intact.
-
Right Hemicolectomy:
This surgery takes out the right side of the colon, including the cecum, ascending colon, and part of the transverse colon.
-
Left Hemicolectomy:
It means taking away the left side of the colon, including part of the transverse colon, descending colon, and sigmoid colon. It is performed for left-sided colon cancer or other localized diseases.
-
Ileocecectomy
In an Ileocecectomy, the surgeon resects a portion of the distal ileum and the cecum.4UpToDate. (n.d.). Overview of colon resection. Retrieved from https://www.uptodate.com/contents/overview-of-colon-resection?search=colectomy§ionRank=2&usage_type=default&anchor=H644993939&source=machineLearning&selectedTitle=1%7E150&display_rank=1#H644993939
Pre-operative Preparations for Colectomy
Preoperative preparations for this procedure include:
- Dietary Modifications – Patients may need to follow a low-fiber or liquid diet before surgery to reduce bowel contents.
- Bowel Preparation – Laxatives or enemas may be prescribed to cleanse the colon before the procedure.
- Medication Adjustments – Certain medications, such as blood thinners and NSAIDs, may need to be stopped or adjusted.
- Infection Prevention – Antibiotics may be given to reduce the risk of infection.
- Hydration and Nutrition – IV fluids or nutritional support may be necessary for patients with poor nutritional status.
- Smoking and Alcohol Cessation – Stopping smoking and alcohol consumption improves healing and reduces complications.
- Preoperative Testing – Blood tests, imaging, and cardiac evaluations ensure the patient is fit for surgery.
Colectomy Procedure
Mainly, there are two categories of this procedure. Both are explained next:
Open Colectomy:
This enables the surgeon to see directly into the colon, so he can maneuver accurately throughout. But it usually requires a longer recovery time. Laparoscopic or robotic-assisted colectomy, however, leaves less scars and requires shorter healing times. Therefore, it is superior to open colectomy. But open colectomy may be a last resort in extreme cases where doctors are still unable to get what they need.
Laparoscopic Colectomy:
Laparoscopic colectomy, in which the doctor makes a number of small incisions on the soft portion of the abdomen and uses specialized equipment. Some of the factors that decide whether to proceed by open or laparoscopic surgery are the patient’s general state of health, how complicated a case is, and individual surgeon talent. Because laparoscopic colectomy produces fewer scars, shorter hospital stays and faster recovery times than open surgery, it has usually replaced that operation. This method, however, has drawbacks. Laparoscopy can help surgeons prevent post-surgical problems and care for the patient better.5Johns Hopkins Medicine. (n.d.). *Colectomy*. Retrieved from [https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/colectomy](https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/colectomy).
Colectomy Recovery Time
Recovery time after this procedure depends upon your health and the kind of colectomy you have. Healing time often extends several weeks, in most cases. Generally speaking, patients who undergo laparoscopic surgery recover more quickly than those who have open surgery. In addition, laparoscopic surgery has less recovery time and fewer complications.
Complications of Colectomy
While this procedure is mostly safe and effective, it carries its own problems.6Soon, I. S., Wrobel, I., deBruyn, J. C., Sauve, R., Sigalet, D. L., Kaplan, B. S., Proulx, M. C., & Kaplan, G. G. (2012). Postoperative complications following colectomy for ulcerative colitis in children. Journal of pediatric gastroenterology and nutrition, 54(6), 763–768. https://doi.org/10.1097/MPG.0b013e318245265c Typical complications include:
Infection:
Infection worsens the prognosis of any surgical procedure. Colectomy also increases the risk of infection in the abdominal cavity. This is another potential complication that highlights the need for close post-operative monitoring. Symptoms of infections include fever, pain, or abnormal secretions. The doctor may prescribe antibiotics according to the bacteria that appears in the culture report. Early intervention stops the infection, thus allowing patients to recover quicker.
Bleeding:
Excessive bleeding may occur during or after surgery. Immediate post-operative bleeding may require blood transfusions or additional surgical intervention. Delayed bleeding, which occurs days after surgery, may need arterial embolization or surgical exploration to locate and control the source of hemorrhage.
Anastomotic Leak:
In colectomy, the remaining healthy sections of the colon are reconnected (anastomosis). If the connection does not heal properly, digestive contents can leak into the abdominal cavity, leading to infection, abscess formation, or peritonitis. Symptoms include severe abdominal pain, fever, and an increased heart rate. Treatment may require antibiotics, drainage, or surgical repair, and in some cases, a temporary colostomy or ileostomy.
Bowel Obstruction:
After this procedure, scar tissue (adhesions) may form, leading to partial or complete bowel obstruction. This can cause symptoms such as severe bloating, abdominal pain, nausea, and vomiting. In some cases, non-surgical management with bowel rest and fluid therapy is sufficient, but severe obstructions may require further surgical intervention.
Changes in Bowel Function:
Patients often experience alterations in bowel habits, such as diarrhea, constipation, or increased frequency of bowel movements. These changes result from modifications in the digestive tract and may persist for weeks or months. Doctors will often recommend a change in diet, such as eating more fiber foods, and taking medication such as laxatives or antidiarrheal to treat these bowel movements.
Hernia:
Some individuals may suffer from a hernia. This happens when this surgery makes the abdominal muscles weak. A bulge near the surgical incision may result from weakening muscles that create pain or discomfort. Sometimes surgery is needed in order to strengthen the muscles of the abdomen and prevent growth of hernias.7Widmar M, Keskin M, Beltran P, Nash GM, Guillem JG, Temple LK, Paty PB, Weiser MR, Garcia-Aguilar J. Incisional hernias after laparoscopic and robotic right colectomy. Hernia. 2016 Oct;20(5):723-8. doi: 10.1007/s10029-016-1518-2. Epub 2016 Jul 28. PMID: 27469592; PMCID: PMC5025379.
Nerve Damage:
Nerve injury is another potential complication of a colectomy. Tissues in the abdominal cavity are manipulated during surgical operation, which may inadvertently affect neighboring nerves. This can result in discomfort, numbness, or tingling as symptoms. Nerve injury is usually very transient, but can sometimes be more prolonged.8Giglia MD, Stein SL. Overlooked Long-Term Complications of Colorectal Surgery. Clin Colon Rectal Surg. 2019 May;32(3):204-211. doi: 10.1055/s-0038-1677027. Epub 2019 Apr 2. PMID: 31061651; PMCID: PMC6494605.
Sexual Dysfunction:
A colectomy may also impact sexual function. Libido and sexual function can also be altered due to hormonal changes or postoperative psychological stress. Managing sexual dysfunction after colectomy involves counselling, medication or other interventions. Open communication should always be maintained with healthcare professionals so as to reduce sexual dysfunction and enhance the quality of life.9Liot, E., Christou, N., De Sousa, S., Klein, J., Pouya, I., Guedj, D., Buchs, N. C., & Ris, F. (2022). Patients’ related sexual outcomes in colorectal surgery. Frontiers in Oncology, 12, 968978. https://doi.org/10.3389/fonc.2022.968978
Colectomy vs. Colostomy
A colectomy involves the removal of all or part of the colon, while a colostomy involves creating an opening (stoma) in the abdominal wall to divert waste into an external pouch. Some colectomy procedures require a temporary colostomy to allow healing, but not all patients undergoing colectomy will need a colostomy. Colostomies are more common in procedures involving the rectum, such as low anterior resection for rectal cancer.
Understanding the potential complications of colectomy can help patients make informed decisions and take necessary precautions for a smoother recovery process.
Summary
A colectomy is a vital surgical procedure that can effectively treat severe digestive tract conditions, including colon cancer, diverticulitis, and inflammatory bowel disease. While it carries potential risks and complications, advancements in surgical techniques, such as laparoscopic colectomy, have improved patient outcomes and recovery times. Understanding the procedure, its risks, and post-operative care can help patients make informed decisions and ensure a smoother recovery process. Consulting a healthcare provider for personalized guidance is essential for achieving the best possible results.
Refrences
- 1National Cancer Institute. Colectomy. In: NCI Dictionary of Cancer Terms [Internet]. Available from: https://www.cancer.gov/publications/dictionaries/cancer-terms/def/colectomy.
- 2Ozgur, I., Liska, D., Cengiz, T. B., Sapci, I., Valente, M. A., Holubar, S. D., Steele, S. R., Bhatt, A., & Gorgun, E. (2022). Colectomy for polyps is associated with a high risk for complications and low risk for malignancy: Time for endoluminal surgery?. American journal of surgery, 223(3), 463–467. https://doi.org/10.1016/j.amjsurg.2021.11.030
- 3Lettieri, P. R., Kunac, A., Oliver, J. B., & Anjaria, D. J. (2022). Sigmoid Colectomy for Sigmoid Volvulus Through a Limited Left Lower Quadrant Transverse Laparotomy Incision Without Laparoscopy. The American surgeon, 88(9), 2233–2234. https://doi.org/10.1177/00031348221093530
- 4UpToDate. (n.d.). Overview of colon resection. Retrieved from https://www.uptodate.com/contents/overview-of-colon-resection?search=colectomy§ionRank=2&usage_type=default&anchor=H644993939&source=machineLearning&selectedTitle=1%7E150&display_rank=1#H644993939
- 5Johns Hopkins Medicine. (n.d.). *Colectomy*. Retrieved from [https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/colectomy](https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/colectomy).
- 6Soon, I. S., Wrobel, I., deBruyn, J. C., Sauve, R., Sigalet, D. L., Kaplan, B. S., Proulx, M. C., & Kaplan, G. G. (2012). Postoperative complications following colectomy for ulcerative colitis in children. Journal of pediatric gastroenterology and nutrition, 54(6), 763–768. https://doi.org/10.1097/MPG.0b013e318245265c
- 7Widmar M, Keskin M, Beltran P, Nash GM, Guillem JG, Temple LK, Paty PB, Weiser MR, Garcia-Aguilar J. Incisional hernias after laparoscopic and robotic right colectomy. Hernia. 2016 Oct;20(5):723-8. doi: 10.1007/s10029-016-1518-2. Epub 2016 Jul 28. PMID: 27469592; PMCID: PMC5025379.
- 8Giglia MD, Stein SL. Overlooked Long-Term Complications of Colorectal Surgery. Clin Colon Rectal Surg. 2019 May;32(3):204-211. doi: 10.1055/s-0038-1677027. Epub 2019 Apr 2. PMID: 31061651; PMCID: PMC6494605.
- 9Liot, E., Christou, N., De Sousa, S., Klein, J., Pouya, I., Guedj, D., Buchs, N. C., & Ris, F. (2022). Patients’ related sexual outcomes in colorectal surgery. Frontiers in Oncology, 12, 968978. https://doi.org/10.3389/fonc.2022.968978

