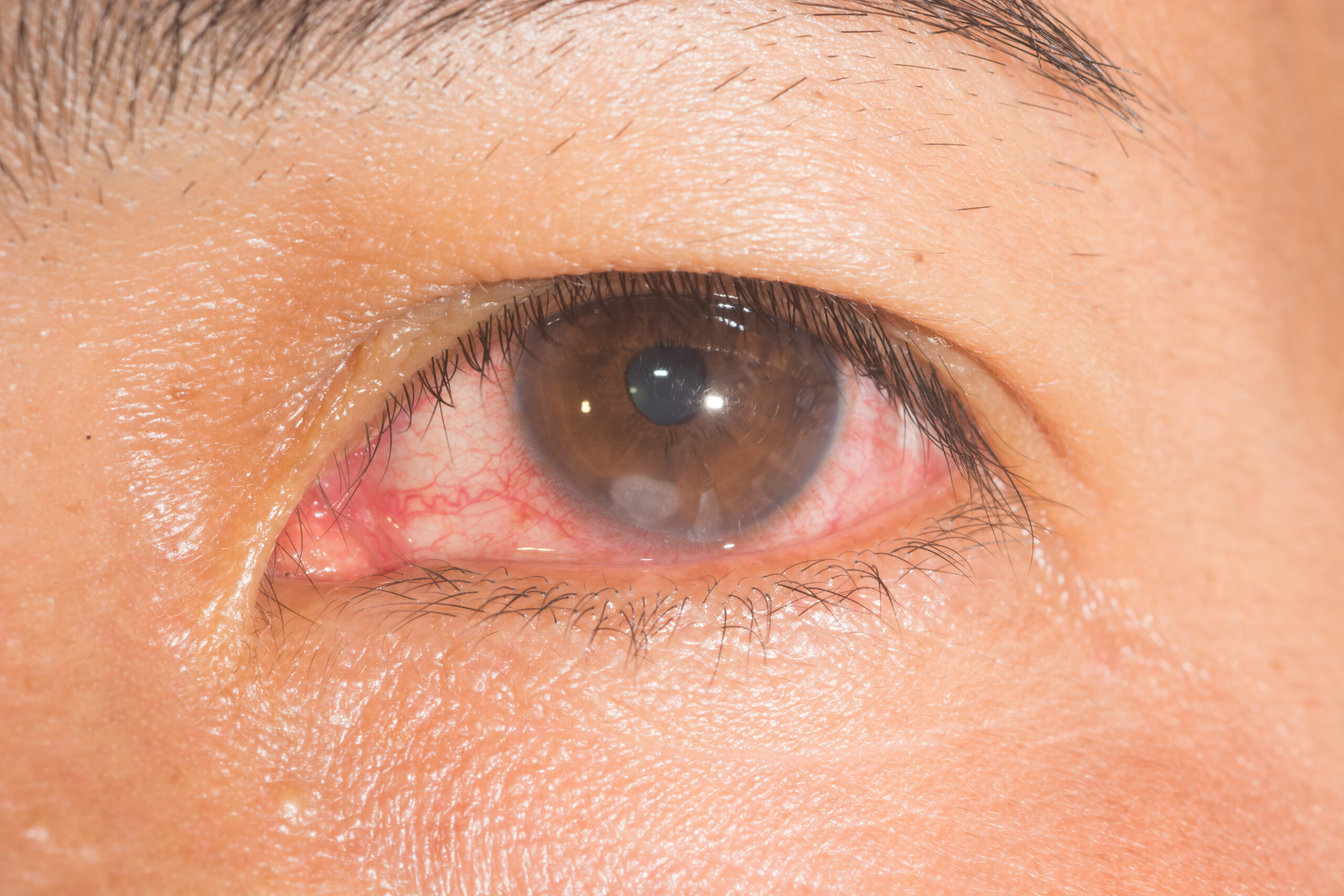
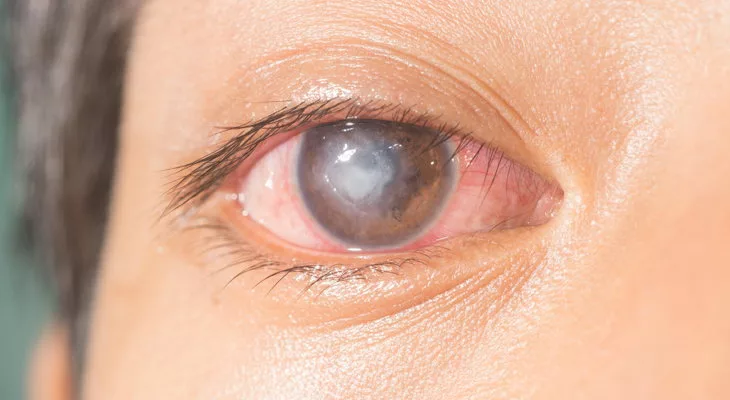
Corneal ulcer, also known as keratitis, is a painful open sore that develops on the clear outer surface of the eye, termed the cornea. It is typically caused by infection or injury, leading to severe complications such as vision loss or blindness if left untreated. The cornea is a critical part of the eye and plays a vital role in focusing light onto the retina. It comprises multiple layers of cells and is kept clear by a continuous flow of tears. When the cornea becomes damaged, it is vulnerable to infections, which can lead to corneal ulcers.1American Academy of Ophthalmology. (n.d.). *Corneal ulcer*. Retrieved December 19, 2024, from [https://www.aao.org/eye-health/diseases/corneal-ulcer](https://www.aao.org/eye-health/diseases/corneal-ulcer)

It’s crucial to seek prompt medical attention if you suspect you have a corneal ulcer to prevent the spread of infection and to protect your eye.
Causes Of Corneal Ulcer
The common causes of a corneal ulcer include:
- Bacterial infections: Bacteria such as staphylococcus and streptococcus can cause corneal ulcers. These infections can occur due to various factors, including poor hygiene, exposure to polluted materials, and contact lens use.2Loh K, Agarwal P. Contact lens related corneal ulcer. Malays Fam Physician. 2010 Apr 30;5(1):6-8. PMID: 25606178; PMCID: PMC4170392.
- Viral infections: Viruses play a role in causing corneal ulcers. Some of the most common viruses associated with corneal ulcers include herpes simplex virus (HSV), varicella-zoster virus (VZV), and adenovirus. These viruses can cause corneal infections that can lead to the development of corneal ulcers.3American Academy of Ophthalmology. (n.d.). Corneal Infections. Retrieved March 13, 2023, from https://www.aao.org/eye-health/diseases/corneal-infections
- Fungal infections: Fungi such as Aspergillus and Fusarium can cause corneal ulcers. These infections are more common in people with weak immune systems or those who work in environments with a lot of mold or fungus.
- Physical injuries: Trauma to the eye, such as a scratch or abrasion, can cause a corneal ulcer.
- Dry eyes: Dry eyes can cause damage to the cornea. Various factors, such as age and Sjogren syndrome, can cause this.
- Chemical Injury: Harmful substances such as acids or alkalis, when coming into direct contact with the eye, cause damage to the cornea, leading to redness, severe pain, and blurred vision.
- Immune system disorders: Immune system disorders are conditions in which the body’s immune system is not operating effectively, increasing the risk of infection and other health issues.
What are the symptoms of a corneal ulcer?
A corneal ulcer can cause a wide range of symptoms, depending on the severity of the infection and the underlying cause. The ulcer can appear as a grey or white spot on the cornea.
Some common corneal ulcer symptoms include:
- Eye pain: This is often the first symptom of a corneal ulcer and can range from mild discomfort to a significantly painful experience. The pain may be constant or worsen with eye movement or light or dust particle exposure.
- Redness: The affected eye may appear red and swollen due to inflammation and increased blood flow to the infected area.
- Pus-like discharge: pus-like discharge from the eye can signify a corneal ulcer.
- Tearing: The eye may produce more tears than normal as a response to the pain and irritation caused by the ulcer.
- Blurred vision: The ulcer can cause a clouding or hazy appearance in the affected eye.
- Discharge: The eye may produce a yellowish or greenish discharge.
- Light sensitivity: Some people may experience increased sensitivity to light and may have trouble tolerating bright lights or sunlight.
Other symptoms may also be present in some cases, such as a sensation of a foreign object in the eye or eyelid edema (swelling).4MSD Manuals. (n.d.). *Corneal ulcer*. Retrieved December 19, 2024, from [https://www.msdmanuals.com/home/eye-disorders/corneal-disorders/corneal-ulcer#Causes_v26622311](https://www.msdmanuals.com/home/eye-disorders/corneal-disorders/corneal-ulcer#Causes_v26622311)
How is a Corneal Ulcer Diagnosed?
Diagnosing a corneal ulcer involves several steps, beginning with a thorough eye examination conducted by an ophthalmologist or optometrist. The clinician uses a slit lamp, a specialized microscope with high-intensity light, to closely examine the cornea for signs of damage, infection, or irregularities.5Garg P, Rao GN. Corneal ulcer: diagnosis and management. Community Eye Health. 1999;12(30):21-3. PMID: 17491983; PMCID: PMC1706003.
A fluorescein stain test is often performed by applying a dye to the eye’s surface. Under blue light, this dye highlights areas of corneal damage, making it easier to detect ulcers and measure their size and shape.
In cases where the cause of the ulcer is unclear or if the condition does not respond to initial treatment, a sample of corneal tissue or eye fluid may be collected. This sample is sent for microbiological analysis to identify the specific organism (bacteria, fungus, or virus) responsible for the ulcer. This helps in tailoring the treatment to the exact cause.
Prompt diagnosis and treatment are critical to prevent complications, such as scarring, vision loss, or, in severe cases, loss of the eye.
How are Corneal Ulcers Treated?
Treatment of corneal ulcers will depend on the cause and severity of the ulcer. Common treatments include:
- Antimicrobial Therapy: Depending on the findings of the microbiological analysis, appropriate antimicrobial therapy, such as eye drops, ointments, or oral medicine, may be provided to treat the infection and prevent it from spreading.6McLeod SD, Kolahdouz-Isfahani A, Rosamian K, et al. The role of smears, cultures, and antibiotic sensitivity testing in the management of suspected infectious keratitis. Ophthalmology. 1996;103:23–8. doi: 10.1016/s0161-6420(96)30738-0.
- Pain management: Pain relievers, such as ibuprofen or acetaminophen, can help manage eye pain associated with corneal ulcers.
- Bandage contact lenses: These special contact lenses can help protect the affected eye and promote the healing of the ulcer.
- Corticosteroid eye drops: These can reduce inflammation and swelling and help promote the healing of the ulcer.7Palioura S, Henry CR, Amescua G, Alfonso EC. Role of steroids in the treatment of bacterial keratitis. Clin Ophthalmol. 2016 Jan 27;10:179-86. doi: 10.2147/OPTH.S80411. PMID: 26869751; PMCID: PMC4734801.
- Monitoring Progress: Routine follow-up appointments with the eye specialist are necessary to monitor the progress of the treatment and ensure healing.
- Surgical Intervention: In extreme circumstances, surgery may be required to remove damaged tissue and improve recovery.
Healing Stages of corneal ulcers:
Healing of a corneal ulcer typically occurs in several stages. These stages include:
- Inflammation: In the first stage, the eye becomes red and inflamed as the immune system rapidly responds to an infection or injury. During this stage, the body produces replacement cells to repair damaged tissues. Epithelialization is the process of forming new cells. It helps to re-establish the integrity of the cornea.
- Stromal healing: During this stage, the deeper layers of the cornea begin to heal. Blood vessels may grow in the area to provide oxygen and nutrients, which can cause the ulcer to appear cloudy.
- Scarring: As the healing process continues, scar tissue forms. Scar tissue can cause the cornea to become cloudy and distorted. It can also affect vision.
- Remodeling: In the final stage, the cornea continues to repair itself. Clear tissue replaces scar tissue, and the cornea returns to normal shape and function.
It’s imperative to follow the treatment plan provided by an ophthalmologist to ensure proper healing and prevent complications.
What precautions can you take to prevent corneal ulcers?
You can take several steps to reduce your risk of developing corneal ulcers. These steps are listed below:
- Protect your eyes from infection: Wear protective eyewear during sports or other activities that could cause eye injury or surgery.
- Have proper hygiene: Wash your hands every time and avoid touching your eyes with unclean hands to limit infection.
- Avoid wearing contact lenses overnight: This increases the risk of infection and can lead to a corneal ulcer, which prevents Acanthamoeba keratitis.
- Get regular eye checkups: Regular eye exams can help detect early signs of a corneal ulcer or other eye problems, allowing prompt treatment.
- Manage overall health conditions: Chronic health conditions such as autoimmune diseases or diabetes can affect and weaken the cornea and increase the risk of corneal ulcers. It is, therefore, necessary to take care of these conditions to prevent corneal ulcers.
- Avoid sharing personal items: Avoid sharing towels, contact lenses, or eye makeup with others to reduce the risk of infection.
Following these guidelines can help reduce your risk of developing a corneal ulcer and maintain healthy eyes and overall health.8Arbabi EM, Kelly RJ, Carrim ZI. Corneal ulcers in general practice. Br J Gen Pract. 2018 Jan;68(666):49-50. Doi: 10.3399/bjgp17X694385. PMID: 29284643; PMCID: PMC5737312.
Conclusion
In conclusion, corneal ulcer is a serious eye condition that can cause significant damage to the cornea if not treated on time. It is imperative to seek medical attention immediately if you suspect you have a corneal ulcer, as it can cause permanent vision loss if not treated promptly.
Refrences
- 1American Academy of Ophthalmology. (n.d.). *Corneal ulcer*. Retrieved December 19, 2024, from [https://www.aao.org/eye-health/diseases/corneal-ulcer](https://www.aao.org/eye-health/diseases/corneal-ulcer)
- 2Loh K, Agarwal P. Contact lens related corneal ulcer. Malays Fam Physician. 2010 Apr 30;5(1):6-8. PMID: 25606178; PMCID: PMC4170392.
- 3American Academy of Ophthalmology. (n.d.). Corneal Infections. Retrieved March 13, 2023, from https://www.aao.org/eye-health/diseases/corneal-infections
- 4MSD Manuals. (n.d.). *Corneal ulcer*. Retrieved December 19, 2024, from [https://www.msdmanuals.com/home/eye-disorders/corneal-disorders/corneal-ulcer#Causes_v26622311](https://www.msdmanuals.com/home/eye-disorders/corneal-disorders/corneal-ulcer#Causes_v26622311)
- 5Garg P, Rao GN. Corneal ulcer: diagnosis and management. Community Eye Health. 1999;12(30):21-3. PMID: 17491983; PMCID: PMC1706003.
- 6McLeod SD, Kolahdouz-Isfahani A, Rosamian K, et al. The role of smears, cultures, and antibiotic sensitivity testing in the management of suspected infectious keratitis. Ophthalmology. 1996;103:23–8. doi: 10.1016/s0161-6420(96)30738-0.
- 7Palioura S, Henry CR, Amescua G, Alfonso EC. Role of steroids in the treatment of bacterial keratitis. Clin Ophthalmol. 2016 Jan 27;10:179-86. doi: 10.2147/OPTH.S80411. PMID: 26869751; PMCID: PMC4734801.
- 8Arbabi EM, Kelly RJ, Carrim ZI. Corneal ulcers in general practice. Br J Gen Pract. 2018 Jan;68(666):49-50. Doi: 10.3399/bjgp17X694385. PMID: 29284643; PMCID: PMC5737312.