Trichinosis, also known as trichinellosis, is a parasitic infection caused by nematodes of the genus Trichinella. Humans contract the infection by consuming raw or undercooked meat contaminated with Trichinella larvae. Trichinella is an intestinal roundworm primarily seen in insufficiently cooked or raw food. Pork and its products are also the main sources of infection. This infection possesses the risk of being deadly, but commonly, it is a self-limiting disorder. Common complications include myocarditis, encephalitis, and respiratory failure.1Furhad S, Bokhari AA. Trichinosis. 2019. Globally, an estimated 10,000 cases occur annually, with higher prevalence in regions where raw or undercooked meat consumption is common.2Rawla P, Sharma S. Trichinella spiralis Infection. StatPearls [Internet]: StatPearls Publishing; 2023. Sir Richard Owen and Sir James Paget first discovered trichinosis in 1835 while observing a mass of worms lining the diaphragm of a cadaver.3Furhad S, Bokhari AA. Trichinosis. 2019.
Life Cycle and Transmission of Trichinella Species
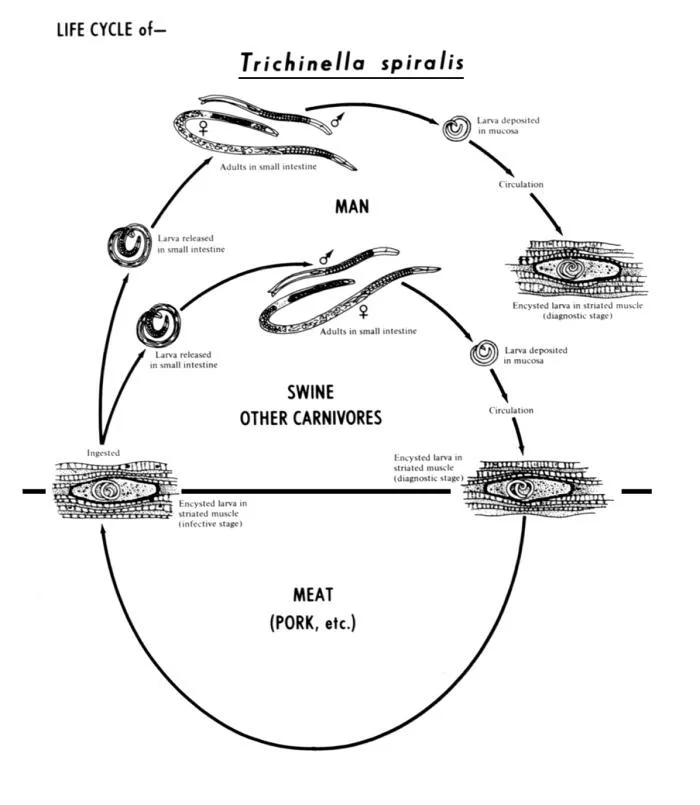
There are several species of Trichinella. These include T. spiralis (Most Common), T.nativa, T. psuedospiralis, T. britovi, T.murelli, T.pupuae, T. zimbabwensis, and T. nelson. Encysted larvae and adult worms typically develop within a single vertebrate host. In the life cycle of Trichinella, an infected animal acts as both the definitive host (where adult worms reproduce) and the intermediate host (where larvae encyst). The life cycle requires a second host to propagate, as the encysted larvae must be consumed by another animal. The commonly studied T. spiralis life cycle involves pigs, rodents, and humans.4Bruschi F. Trichinella and trichinellosis: Elsevier; 2021.
Trichinellosis has a life cycle that consists of the following stages:
Domestic Stage:
The domestic cycle involves domestic animals such as pigs, rodents, and sometimes horses. Pigs often become infected by consuming infectious larvae in raw meat, such as from rats.
Sylvatic Stage:
The sylvatic cycle occurs in wildlife, affecting animals such as wild boars, bears, and moose. Wildlife can transmit the parasite when consumed by domestic animals or humans.5yM Vaidya R, Zende J, Waghmare R, Moon S, Kale L. Trichinellosis/Trichinosis: Life Cycle, Transmission, Symptoms.
T. spiralis typically infects domestic animals, while other Trichinella species are more common in wildlife. Poor management of domestic and wild animals facilitates the transfer of parasites from wildlife to domestic animals through urban wildlife, such as rats and mice. Infected animals include wild boars, bears, and foxes.6Rawla P, Sharma S. Trichinella spiralis Infection. StatPearls [Internet]: StatPearls Publishing; 2023.
Gastrointestinal Phase:
HHumans acquire infection by consuming raw or undercooked meat contaminated with encysted larvae. Once ingested, the larvae emerge from their nurse cells in the stomach and invade the intestinal mucosa. They molt four times and develop into adults within 30 hours. After five days of mating, predomination occurs, and females produce live offspring larvae. The size of newborn male larvae is 1.2 mm, and the female is 2.2 mm in length. The female worms can produce up to 1500 larvae in their life of six weeks.
Systemic Phase:
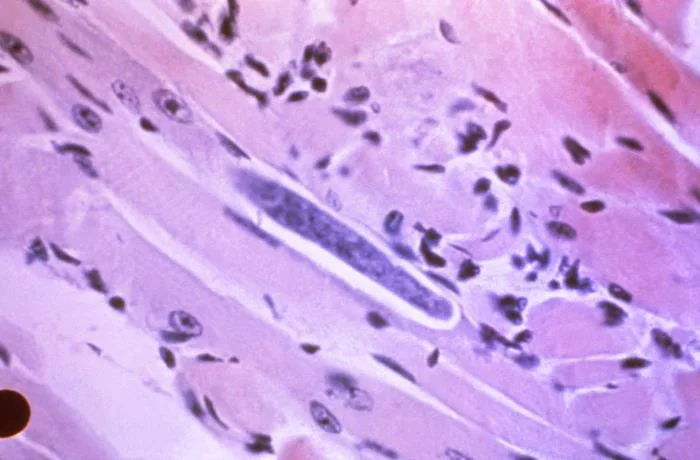
After being released, the larvae penetrate the intestinal barrier and enter the lymphatic vessels and bloodstream. They migrate to striated muscles, where they become encysted in active muscles such as the tongue, diaphragm, and intercostal muscles. Here, the larvae develop into the infective stage within nurse cells. The life cycle continues when the infected host is consumed by another animal.7Mousa ESI, Elgendy AM, Mohamed SM, SF H. An Overview about Trichinosis; Morphology, Pathogenesis, and Presentation.8yM Vaidya R, Zende J, Waghmare R, Moon S, Kale L. Trichinellosis/Trichinosis: Life Cycle, Transmission, Symptoms.
Causes of Trichinosis
Trichinella spiralis species is the most common cause of human disease. After getting trichinosis by eating infected meat, people cannot pass the parasite directly to another person. Infected meat comes from wild animals such as wolves, bears, wild boar, seals, cougars, and walruses. Domestic horses and pigs become infected when they feed on garbage containing infected meat scraps. You can not get trichinosis from beef, chicken, and other meats, as these animals do not eat meat. If beef or other kinds of meat were ground in a grinder previously used to grind the infected meat, it could also become a cause of the infection. You can also get trichinosis by eating improperly stored meats. Unclean kitchen utensils used to prepare meats also cause this infectious disease.9Chelsea Marie WAP, Jr. Trichinosis 2022 [Available from: https://www.msdmanuals.com/home/infections/parasitic-infections-nematodes-roundworms/trichinosis.
Symptoms
The symptoms of trichinosis vary, and the severity of these symptoms depends on the number of larvae ingested through food. In some cases, symptoms are absent; in others, they last for even months.
Mild Symptoms:
In mild cases, trichinosis may present with non-specific flu-like symptoms, including:
- Fatigue
- Low-grade fever
- Muscle aches
Gastrointestinal (Enteric) Phase:
Symptoms typically develop within 1–2 days after ingesting infected meat and include:
- Diarrhea
- Nausea
- Fever
- Vomiting
- Abdominal pain and cramps
- Heartburn and dyspepsia (less common)
- Eosinophilia (elevated eosinophils in blood tests)10NOACK O. TRICHINOSIS
Systemic Phase:
This phase occurs 1–2 weeks after ingestion as larvae migrate to tissues and muscles. Symptoms include:
- Fever
- Weakness and fatigue
- Myalgia (muscle pain)
- Periorbital swelling (swelling around the eyes)
- Headache
- Rashes
- Itchy skin
- Conjunctival redness (red eyes)
- Edema (swelling in other body parts)11yM Vaidya R, Zende J, Waghmare R, Moon S, Kale L. Trichinellosis/Trichinosis: Life Cycle, Transmission, Symptoms.

Severe Symptoms:
In most severe cases, the symptoms can be:
- Encephalitis
- Meningitis
- Myocarditis
- Pneumonia
- Ataxia12yM Vaidya R, Zende J, Waghmare R, Moon S, Kale L. Trichinellosis/Trichinosis: Life Cycle, Transmission, Symptoms.
- Cerebral venous thrombosis13Evans RW, Pattern B. Trichinosis associated with superior sagittal sinus thrombosis. Annals of Neurology. 1982;11(2):216-7.
Trichinosis can also be fatal, depending on the severity of the infection. Death can occur after four to six weeks of severe infection.14Gottstein B, Pozio E, Nöckler K. Epidemiology, diagnosis, treatment, and control of trichinellosis. Clinical microbiology reviews. 2009;22(1):127-45.
Diagnosis
The diagnosis of trichinosis is primarily clinical and later supported by laboratory and molecular findings.
Clinical Evaluation:
Your clinician can diagnose the condition by doing a physical exam. The initial diagnosis began with a detailed history of symptoms such as myalgia, fever, eosinophilia, periorbital edema, and gastrointestinal symptoms. A more critical aspect of the diagnosis is determining the history and exposure to the parasite.
Laboratory Tests:
Laboratory tests that help in diagnosing trichinosis are blood and serological tests.
Blood Tests:
Blood tests include eosinophil count, leukocyte count, muscle enzymes, and antibody testing.
Eosinophil Count
An elevated eosinophil count is one of the main laboratory findings of trichinosis. They appear in between the second and fifth weeks of infection in almost every case. However, a massive decrease in eosinophil levels during an acute infectious stage predicts a severe outcome.
Elevated Levels of Muscle Enzymes in Blood
Myositis also appears between the second and fifth weeks of infection in 75 to 90% and can persist for up to four months. The elevated enzymes include aldolase, lactate dehydrogenase, and phosphokinase.
Leukocytosis
Polymorphonuclear leucocytosis is also a typical feature of trichinosis. It also appears early at the onset of the infection, between the second and fifth weeks of infection.
Immunodiagnosis
Anti-trichinella antibodies in the blood serum are also an important indication. An early increase in immunoglobulin E levels is observed in most of the cases.15Mohamed SMAG, Taha AAR, Hamed EFA, Fawzy EM. Diagnostic Modalities of Trichinellosis. NeuroQuantology. 2022;20(16):2706.
Serological Examination:
Serological testing is a cornerstone of diagnosis.
- Anti-Trichinella Antibodies: The presence of specific antibodies in blood serum, such as immunoglobulin E (IgE) and IgG, is a significant indicator of infection. IgE levels rise early, while IgG is detected more reliably with techniques such as ELISA.
- ELISA: Enzyme-linked immunosorbent assay (ELISA) is a widely used method to detect IgG antibodies in serum. However, it may yield false negatives during early stages, as antibodies take three to five weeks to develop. Serial testing may be required for confirmation.16Yayeh M, Yadesa G, Erara M, Fantahun S, Gebru A, Birhan M. Epidemiology, diagnosis and public health importance of Trichinellosis. Online Journal of Animal and Feed Research. 2020;10(3):131-9.
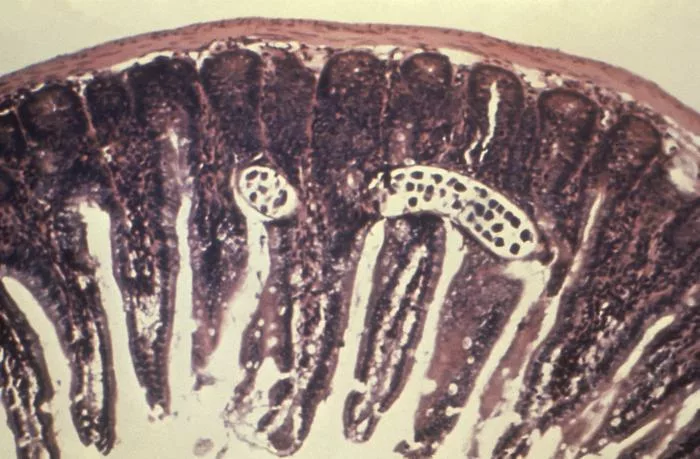
Muscle Biopsy:
Muscle biopsy helps identify the Trichinella larvae within muscle tissues. Findings of muscle biopsy also include inflammatory changes and encysted larvae. However, this process is most effective only after two weeks of infection when the larvae migrate into the muscle fibers.17Mohamed SMAG, Taha AAR, Hamed EFA, Fawzy EM. Diagnostic Modalities of Trichinellosis. NeuroQuantology. 2022;20(16):2706.
Imaging Techniques:
The imaging techniques usually used to diagnose trichinosis are X-rays, computed tomography, and electrocardiogram (ECG). X-rays show calcific densities in the muscles, and CT scans look for neurological dysfunction. ECG shows features of ischemia, myocarditis, pericarditis, etc.18Rawla P, Sharma S. Trichinella spiralis Infection. StatPearls [Internet]: StatPearls Publishing; 2023.
Molecular Techniques:
Advanced methods like polymerase chain reaction (PCR) are capable of detecting Trichinella DNA in muscle tissues. While not commonly used due to its complexity and cost, multiplex PCR offers a simpler and more economical approach for differentiating Trichinella species, making it useful in research and epidemiological studies.19Yayeh M, Yadesa G, Erara M, Fantahun S, Gebru A, Birhan M. Epidemiology, diagnosis and public health importance of Trichinellosis. Online Journal of Animal and Feed Research. 2020;10(3):131-9.
Treatment and Management
The available treatment methods are the following:
Anti-parasitic Medicines:
The most commonly used anthelmintics include mebendazole and albendazole. These are considered a cornerstone treatment of trichinosis as they target the larvae.
Mebendazole
The recommended dose of mebendazole is 200 mg to 400 mg thrice a day for three days. If required, another dose of 400 to 500 mg should be given thrice a Day for an additional ten days. It disrupts the mechanism of glucose uptake in parasites.
Albendazole
The recommended dose of this medicine is 400 mg twice a day for 10 to 14 days. It works by inhibiting the polymerization of tubulin, disrupting the parasite’s ability to absorb glucose and leading to its death. If administered early, albendazole can prevent muscular invasion of the larvae and prevent disease progression.20Furhad S, Bokhari AA. Trichinosis. 2019.
Prednisone
In most severe cases, doctors recommend coadministration of these anti-parasitic medicines with prednisone. The administered dose of prednisone is 30 mg to 60 mg daily for 10 to 14 days.21Rawla P, Sharma S. Trichinella spiralis Infection. StatPearls [Internet]: StatPearls Publishing; 2023.
However, albendazole and mebendazole are not safe for children below 2 years and pregnant women. So, practitioners consider alternative medicines.
Alternative Treatment:
The alternative option for children and pregnant women is Pyrantel. They administer it as a single dose of 10 to 20 mg/kg of the body weight. Primary chemotherapy for severe cases is prednisone, administered at a dose of 30 mg per day for 10 to 15 days. However, pyrantel does not affect muscle or newborn larvae. It only affects the intestinal larvae.22Furhad S, Bokhari AA. Trichinosis. 2019.
Supportive Care:
In addition to the anti-parasitic drugs, supportive care can help in managing the symptoms of the condition.
Non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and naproxen can help in relieving muscle pain in patients. Corticosteroids such as prednisone can reduce inflammation in severe cases of infection and can also manage allergic reactions.23Chelsea Marie WAP, Jr, Trichinosis 2022 [Available from: https://www.msdmanuals.com/home/infections/parasitic-infections-nematodes-roundworms/trichinosis.
Healthcare providers should monitor patients for the potential side effects associated with the treatment. Most patients completely recover, while some experience complications.
Complications
In some cases, patients experience complications after treatment. These complications include:
- Stillbirths
- Vertical infection of the fetus
- Menstrual irregularities
- Weight loss
- Hearing disorders
- Nail and hair loss
- Aphonia
- Hoarseness
- Muscle stiffness
- Skin desquamation
- Heart failure
- Failure of the Central Nervous System (CNS)
- Hypokalemia
- Myocarditis
- Encephalitis
- Pneumonitis
- Adrenal gland insufficiency
- Obstruction of blood vessels
Some long-term complications that can persist up to 10 years post-treatment include:
- Neuropathies
- Conjunctivitis
- Generalized myalgia24Furhad S, Bokhari AA. Trichinosis. 2019.
Prevention
- Lack of education can be a potential source of trichinosis. Meats from horses, wild animals, exotic cuisines, and cultural practices can be a transmission factor. Education can decrease clinical cases. Healthcare providers should educate patients about the risk of transmission. People should know that only salting and smoking the meat is not enough to kill the trichinella cysts.25Furhad S, Bokhari AA. Trichinosis. 2019.
- This infectious disease can be prevented by thoroughly cooking meats. Cooked meats should reach a minimum of 160 F internal temperature. This temperature can kill the larvae of Trichinella.
- Properly clean the meat grinders and other kitchen utensils to prepare the meats.
- After preparing the meat, wash your hands with soap.
- If you want to freeze the meat, make sure that the meat is less than six inches in size.26Chelsea Marie WAP, Jr, Trichinosis 2022 [Available from: https://www.msdmanuals.com/home/infections/parasitic-infections-nematodes-roundworms/trichinosis. Also, the freezing temperature for pork meat is -15 C. However, freezing can not kill the larvae of Trichinella in the meats of wild animals.
- Prevention of trichinosis requires interprofessional teamwork.27Rawla P, Sharma S. Trichinella spiralis Infection. StatPearls [Internet]: StatPearls Publishing; 2023.
Final Remarks
Trichinosis is a significant health problem in areas where people consume undercooked pork and wild game. This infectious disease presents a range of symptoms that vary according to the stage of infection. Most of the cases are mild and resolve simultaneously. Awareness of symptoms, timely diagnosis, and proper treatment are critical for preventing the severity of the infection. Promoting safe food practices and conducting educational initiatives can significantly decrease the incidence of this disease. By fostering a collaborative approach among healthcare providers, food safety communities, and regulators, we can enhance patient outcomes and reduce the global burden of trichinosis.
Refrences
- 1Furhad S, Bokhari AA. Trichinosis. 2019.
- 2Rawla P, Sharma S. Trichinella spiralis Infection. StatPearls [Internet]: StatPearls Publishing; 2023.
- 3Furhad S, Bokhari AA. Trichinosis. 2019.
- 4Bruschi F. Trichinella and trichinellosis: Elsevier; 2021.
- 5yM Vaidya R, Zende J, Waghmare R, Moon S, Kale L. Trichinellosis/Trichinosis: Life Cycle, Transmission, Symptoms.
- 6Rawla P, Sharma S. Trichinella spiralis Infection. StatPearls [Internet]: StatPearls Publishing; 2023.
- 7Mousa ESI, Elgendy AM, Mohamed SM, SF H. An Overview about Trichinosis; Morphology, Pathogenesis, and Presentation.
- 8yM Vaidya R, Zende J, Waghmare R, Moon S, Kale L. Trichinellosis/Trichinosis: Life Cycle, Transmission, Symptoms.
- 9Chelsea Marie WAP, Jr. Trichinosis 2022 [Available from: https://www.msdmanuals.com/home/infections/parasitic-infections-nematodes-roundworms/trichinosis.
- 10NOACK O. TRICHINOSIS
- 11yM Vaidya R, Zende J, Waghmare R, Moon S, Kale L. Trichinellosis/Trichinosis: Life Cycle, Transmission, Symptoms.
- 12yM Vaidya R, Zende J, Waghmare R, Moon S, Kale L. Trichinellosis/Trichinosis: Life Cycle, Transmission, Symptoms.
- 13Evans RW, Pattern B. Trichinosis associated with superior sagittal sinus thrombosis. Annals of Neurology. 1982;11(2):216-7.
- 14Gottstein B, Pozio E, Nöckler K. Epidemiology, diagnosis, treatment, and control of trichinellosis. Clinical microbiology reviews. 2009;22(1):127-45.
- 15Mohamed SMAG, Taha AAR, Hamed EFA, Fawzy EM. Diagnostic Modalities of Trichinellosis. NeuroQuantology. 2022;20(16):2706.
- 16Yayeh M, Yadesa G, Erara M, Fantahun S, Gebru A, Birhan M. Epidemiology, diagnosis and public health importance of Trichinellosis. Online Journal of Animal and Feed Research. 2020;10(3):131-9.
- 17Mohamed SMAG, Taha AAR, Hamed EFA, Fawzy EM. Diagnostic Modalities of Trichinellosis. NeuroQuantology. 2022;20(16):2706.
- 18Rawla P, Sharma S. Trichinella spiralis Infection. StatPearls [Internet]: StatPearls Publishing; 2023.
- 19Yayeh M, Yadesa G, Erara M, Fantahun S, Gebru A, Birhan M. Epidemiology, diagnosis and public health importance of Trichinellosis. Online Journal of Animal and Feed Research. 2020;10(3):131-9.
- 20Furhad S, Bokhari AA. Trichinosis. 2019.
- 21Rawla P, Sharma S. Trichinella spiralis Infection. StatPearls [Internet]: StatPearls Publishing; 2023.
- 22Furhad S, Bokhari AA. Trichinosis. 2019.
- 23Chelsea Marie WAP, Jr, Trichinosis 2022 [Available from: https://www.msdmanuals.com/home/infections/parasitic-infections-nematodes-roundworms/trichinosis.
- 24Furhad S, Bokhari AA. Trichinosis. 2019.
- 25Furhad S, Bokhari AA. Trichinosis. 2019.
- 26Chelsea Marie WAP, Jr, Trichinosis 2022 [Available from: https://www.msdmanuals.com/home/infections/parasitic-infections-nematodes-roundworms/trichinosis.
- 27Rawla P, Sharma S. Trichinella spiralis Infection. StatPearls [Internet]: StatPearls Publishing; 2023.