Ecthyma is a rare skin infection that causes serious disease in people with weak immunity. Ecthyma, a severe form of impetigo, is known as “deep” or “ulcerative impetigo” due to its deeper skin penetration, typically caused by Streptococcus or Pseudomonas bacteria.
What is Ecthyma?
This is an uncommonly seen skin manifestation of an underlying infection in your body. Ecthyma is derived from Greek and means “break out”, “ulcer”, or “pustule”, which are characteristic skin symptoms associated with it. It demands prompt management and care as it can result in serious complications without treatment.1Prieto-Granada, C. N., Alice Z.C. Lobo, & Mihm, M. C. (2018). Skin Infections. Elsevier EBooks, 542–647. https://doi.org/10.1016/b978-0-323-44585-6.00020-
What causes Ecthyma?
Ecthyma is the reaction of your skin tissue to an infection, especially when your immunity is too low to fight back successfully. It is mostly caused by infectious agents, such as species from the following:2Ecthyma | DermNet. (2022). Dermnetnz.org. https://dermnetnz.org/topics/ecthyma
| Bacteria |
|
| Fungi |
|
| Viruses |
|
Risk Factors for Ecthyma
It mostly develops in people who have compromised immune systems. They cannot fight off the infectious agents in their skin or other parts of their tissues. It is also more common in living conditions that promote the growth of bacteria:3Yassaee, M. (2023, June 13). Ecthyma Gangrenosum Clinical Presentation: History, Physical Examination. Medscape.com; Medscape. https://emedicine.medscape.com/article/1053997-clinical
- Medical conditions like diabetes and cancer
- Hot, humid weather
- Crowded living spaces
- Having poor hygiene
- Contact with people who have bacterial skin infections
- Taking medication that weakens your immune system
- Previous skin trauma, e.g., insect bites, dermatitis
- Being a neglected child or elderly person
- Serving in the military
Types of Ecthyma
There are no official types. However, several skin disorders, including ulcerative and pustular lesions, are common in it.
Classic Ecthyma
It is usually caused by Streptococcus or Staphylococcus bacteria. Even though it is more severe than regular impetigo, it causes less skin damage than ecthyma gangrenosum.
Ecthyma Gangrenosum
Ecthyma gangrenosum is much more serious. Pseudomonas bacteria cause it in immunocompromised people like those who have diabetes, cancer, or HIV. This is associated with a systemic disorder causing skin infection and cell death. It heals with scarring.
Moreover, it is a serious disorder because of how early it progresses and how Pseudomonas is resistant to many antibiotics. Without prompt treatment, it causes more complications as well as death. 4Ecthyma gangrenosum | DermNet. (2022). Dermnetnz.org. https://dermnetnz.org/topics/ecthyma-gangrenosum
Ecthyma Contagiosum
Contagious ecthyma is a viral disease in cattle. It is also called “orf”. It is sometimes transmitted to humans who come in contact with the infected animals. Orf is caused by Parapoxviruses. It is a rare condition after the eradication of smallpox from the world. However, outbreaks can still occur in less developed countries.5Wajahat Efridi, Jain, H., Sathe, N. C., & Ahmed, K. (2023, November 30). Orf Viral Infection. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK562191/
Symptoms of Ecthyma
It is a progressive disease. Lesions vary in size and location. They are around 0.5-3 cm in size and occur on various body parts:
- Hands and feet
- Limbs
- Buttocks
- Inguinal region
- Genital area
First, a small area of skin becomes inflamed. A blister or pustule develops in this region, which feels itchy. After that, a crust forms over it. An ulcer is formed under this crust.
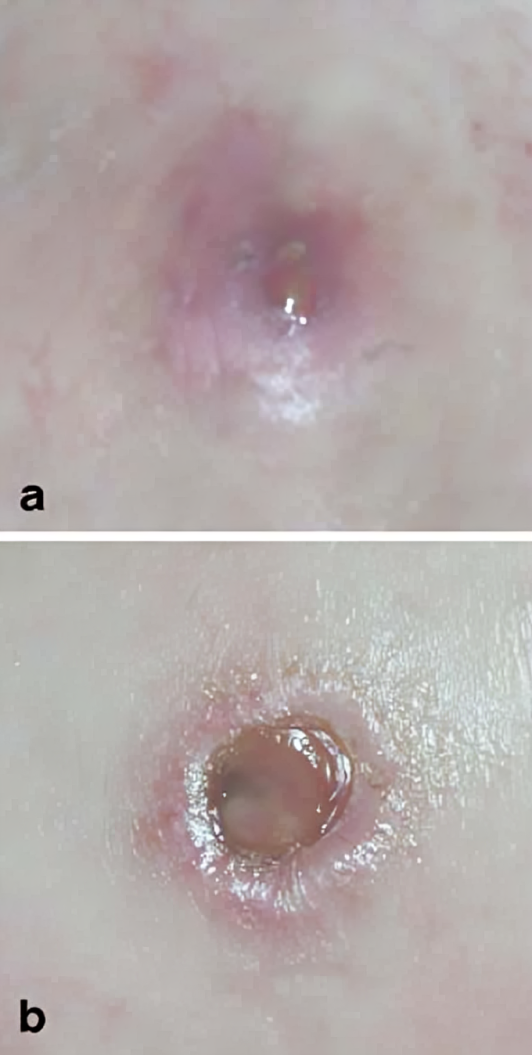
The crust is hard and painful to remove as it is closely attached to the skin. However, once removed, it reveals a swollen, red ulcer underneath. It often involves nearby lymph nodes and causes pain. Symptoms can include:
- Crusty, well-demarcated lesions
- Indurating ulcers
- Oozing and pus
- Open wounds
- Pain and discomfort
- Itching and scratching
- Lymphadenopathy
In ecthyma gangrenosum, the lesions are gangrenous and necrotic. They occur more commonly in areas with skin folds.6Ecthyma. (2020). Mount Sinai Health System. https://www.mountsinai.org/health-library/diseases-conditions/ecthyma#:~:text=The%20main%20symptom%20of%20ecthyma,away%2C%20a%20crusty%20ulcer%20appears.
Complications of Ecthyma
It has several complications, all varying in severity depending on the extent of the disease and the type of causative organism:
- Scarring
- Cellulitis
- Lymphangitis
- Lymphadenitis
- Gangrene
- Post-streptococcal glomerulonephritis
- Septic shock and death
How is Ecthyma Diagnosed?
This is not a common disease. Doctors will suspect you have it if you have a regular, crusty skin rash and give a history pointing to any form of ecthyma. They also look for red flags like gangrenous wounds, which indicate ecthyma gangrenosum.
History & Physical Exam
Doctors can suspect you have this condition based on any risk factors in your medical history, especially if you have a known history of being immunocompromised. They will also ask questions to determine the severity of your disease to start the right antibiotic treatment until your lab results are released.
A thorough skin and physical exam is also necessary for diagnosing it. Different kinds of ecthyma occur in different places. Deep impetigo often appears on your lower extremities. However, ecthyma gangrenosum occurs in skin folds like your inguinal and perianal regions. Contagious ecthyma (caused by a virus) is usually visible as nodules on your hands.
Lab Investigations
The doctors will run a complete panel of lab investigations to determine the cause of your ecthyma. This includes finding out what organism causes it and, if you have an undiagnosed disease, the underlying medical conditions.
Gram Stain
A Gram test identifies the presence of bacteria by dyeing their walls. A doctor will check fluid samples from the pustules on your skin under a microscope for bacteria. Streptococcus and Staphylococcus stain “positively” and appear red or pink. Pseudomonas stains “negatively” and looks blue or violet. Different antibiotics treat infections caused by different organisms, so Gram stain also helps doctors provide you with the right treatment.
Blood Culture
Blood cultures help detect any bacteria or fungi in your bloodstream. Depending on your history, the doctors will check for different infectious organisms. In addition, bacteremia usually points to more severe disease. This helps doctors give you more rigorous treatment to cure you of ecthyma.
General blood tests help find out the underlying cause. For instance:
- Complete blood count (for infections and cancer)
- Resting and fasting blood sugar levels, HBA1C (for diabetes)
- Serum electrolytes
- Tests for common infectious agents for immunodeficiency, such as: HIV, Hepatitis, Tuberculosis
Skin Biopsy
A doctor will take a sample of your skin, 4 to 5 mm deep into its layers. They will then place it in a formalin solution and perform different tests on it. Usually, the results show the type of organism causing the eczema, white blood cells, and debris from damage to the skin.
Tissue Biopsy
Ecthyma gangrenosum can require tissue biopsy. Deeper tissues are sampled and studied. They often show necrosis and hemorrhage.
Urine Culture
In case of suspicion of a Pseudomonas infection, urine samples are also obtained.
Treatment of Ecthyma
As it is mostly caused by bacteria, it is treated with antibiotics. In addition, your doctor will guide you about general measures to heal your skin faster and prevent its recurrence.
Supportive Care
The affected areas are cleaned with soap and water. Doctors will advise you to practice better hygiene and reduce risk factors in your life. They will also ask you to adopt a better diet, especially during treatment:
- Using separate towels and personal hygiene products
- Showering daily with antiseptic soap
- Using soothing, non-irritating emollients to avoid scratching the lesions
- Using insect repellants to avoid more trauma to the skin
In addition, hospitalized patients are monitored carefully. Regulating blood pressure and maintaining proper oxygen saturation improves patient outcomes in ecthyma gangrenosum. If you have sepsis, doctors will admit you to the Intensive Care Unit for round-the-clock care.
Antibiotics
Antibiotics are medicines that kill or stop the growth of living organisms like bacteria and fungi. Depending on the causative agent, various antibiotics are used to treat ecthyma.7Davis, L. S. (2021, November 8). Ecthyma Treatment & Management: Medical Care, Surgical Care, Prevention. Medscape.com; Medscape. https://emedicine.medscape.com/article/1052279-treatment
Topical
Topical antibiotics are applied directly to the skin. They kill the bacteria on the skin, stop further skin damage, and prevent bacteria from penetrating deeper tissues. They need to be applied at least thrice a day after crusts have been cleaned.

A variety of topical antibiotics can be applied to your lesions if it is caused by Streptococcus:
- Mupirocin
- Fusidic acid
- Retapamulin
- Ozenoxacin
- Minocycline
- Bacitracin
Topical antibiotics can improve mild cases. Doctors will administer them alongside oral and IV antibiotics for deeper skin infections and systemic diseases, such as ecthyma gangrenosum.
Oral
Your doctor will recommend oral medications if the condition doesn’t improve with topical antibiotics and is associated with other symptoms of infection, like fever.
Streptococcal ecthyma is treated with oral penicillin, such as dicloxacillin. The medication is usually administered for at least a week. In the case of Staphyocuss aureus, cephalexin is also given, as this bacteria is highly resistant to basic antibiotics.
Many other options are available for advanced disease, drug resistance, and allergies to penicillin. Your doctors may combine a few drugs to treat superimposed infections:
- Cefaclor
- Cefprozil
- Cefuroxime
- Azithromycin
- Clarithromycin
- Roxithromycin
- Erythromycin
- Co-trimoxazole
- Clindamycin
- Linezolid
- Minocycline
- Doxycycline
Ecthyma gangrenosum requires more extensive treatment. It has life-threatening complications and can result in death, so treatment is prompt. Empiric therapy is started right away if doctors suspect you have it, including drugs like:
- Piperacillin/tazobactam
- Cefepime
- Levofloxacin
- Imipenem
Intravenous
For widespread systemic infections, the antibiotics are administered through an intravenous route. This way, drugs are injected directly into your bloodstream to kill the organisms. Sometimes, vancomycin is used if the bacteria have become resistant to all other antibiotics and are causing serious disease.
Adjuvant Treatment Options
Other than antibiotics, other drugs and treatment methods may also be used to help you recover from ecthyma, especially if it is serious:
- Antifungal agents, e.g., itraconazole, ketoconazole, etc, are used if a fungal agent is a suspected causative organism
- Antiviral drugs are given if the infection is caused by a virus, e.g., sometimes treated with cidofovir.
- Patients with serious ecthyma gangrenosum with neutropenia often have neutropenia (abnormally low neutrophils). Neutrophils help the body fight against bacteria. A granulocyte colony-stimulating factor can be given to improve neutropenia.
- Laser therapy may reduce the appearance of scars once your wounds have healed.
Surgery
Surgery is used to drain deep abscesses of pus and debridement of necrotic tissue in ecthyma gangrenosum. It is often the last resort when your lesions keep spreading and are not responding to any medications. Plastic surgery may also improve the cosmetic appearance of extensive scarring.8Gonnelli, D., N. Degardin, T. Guidicelli, J. Londner, G. Magalon, & Bardot, J. (2012). Rôle du chirurgien plasticien dans la prise en charge de l’ecthyma gangrenosum chez l’enfant : exemple clinique. Annales de Chirurgie Plastique et Esthétique/Annales de Chirurgie Plastique Esthétique, 57(4), 405–408. https://doi.org/10.1016/j.anplas.2010.07.008
Is Ecthyma Contagious?
Ecthyma caused by Streptococcus and Staphylococcus bacteria and orf vrius is highly infectious. It can spread among humans from skin-to-skin contact or contact with secretions and scraping from the skin wounds. Ecthyma gangrenosum is less contagious but much more serious than either of them.
Prognosis for Ecthyma
Ecthyma caused by gram-positive bacteria that respond well to antibiotics has an excellent prognosis. Similarly, contagious ecthyma also has a good prognosis. However, ecthyma gangrenosum has a poor prognosis in immunodeficient people, as 1 in 5 people is estimated to die of the disease and its complications. The mortality rate is as high as 77% in some populations.9Shah, M., & Crane, J. S. (2023, June 28). Ecthyma Gangrenosum. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK534777/
Ecthyma vs Impetigo
It is a more serious skin infection than impetigo. It is also called “deep” or “ulcerative” impetigo because ecthyma infiltrates the dermis and causes ulcers, while impetigo is limited to the stratum corenum of the skin. There are many differences between the two.
| Ecthyma | Impetigo |
| Caused most commonly by Streptococcus pyogenes | Most commonly caused by Staphylococcus aureus |
| Formation of ulcers is characteristic | Pustules rarely become ulcerative |
| Dark colored crusts | Honey colored crusts |
| Scarring is more common | Scarring is unlikely |
| This can lead to major complications | Rarely leads to major complications |
Conclusion
In conclusion, ecthyma refers to a number of ulcerative, crusty skin rashes caused by infectious agents. The most common cause is Streptococcus bacteria. Doctors treat it with antibiotics, supportive measures, and sometimes surgery. The choice of antibiotics depends on the causative organism. Ecthyma gangrenosum, a severe form caused by Pseudomonas, can be fatal without prompt treatment. Ecthyma has a good prognosis.
Refrences
- 1Prieto-Granada, C. N., Alice Z.C. Lobo, & Mihm, M. C. (2018). Skin Infections. Elsevier EBooks, 542–647. https://doi.org/10.1016/b978-0-323-44585-6.00020-
- 2Ecthyma | DermNet. (2022). Dermnetnz.org. https://dermnetnz.org/topics/ecthyma
- 3Yassaee, M. (2023, June 13). Ecthyma Gangrenosum Clinical Presentation: History, Physical Examination. Medscape.com; Medscape. https://emedicine.medscape.com/article/1053997-clinical
- 4Ecthyma gangrenosum | DermNet. (2022). Dermnetnz.org. https://dermnetnz.org/topics/ecthyma-gangrenosum
- 5Wajahat Efridi, Jain, H., Sathe, N. C., & Ahmed, K. (2023, November 30). Orf Viral Infection. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK562191/
- 6Ecthyma. (2020). Mount Sinai Health System. https://www.mountsinai.org/health-library/diseases-conditions/ecthyma#:~:text=The%20main%20symptom%20of%20ecthyma,away%2C%20a%20crusty%20ulcer%20appears.
- 7Davis, L. S. (2021, November 8). Ecthyma Treatment & Management: Medical Care, Surgical Care, Prevention. Medscape.com; Medscape. https://emedicine.medscape.com/article/1052279-treatment
- 8Gonnelli, D., N. Degardin, T. Guidicelli, J. Londner, G. Magalon, & Bardot, J. (2012). Rôle du chirurgien plasticien dans la prise en charge de l’ecthyma gangrenosum chez l’enfant : exemple clinique. Annales de Chirurgie Plastique et Esthétique/Annales de Chirurgie Plastique Esthétique, 57(4), 405–408. https://doi.org/10.1016/j.anplas.2010.07.008
- 9Shah, M., & Crane, J. S. (2023, June 28). Ecthyma Gangrenosum. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK534777/

