What is Erysipelas?
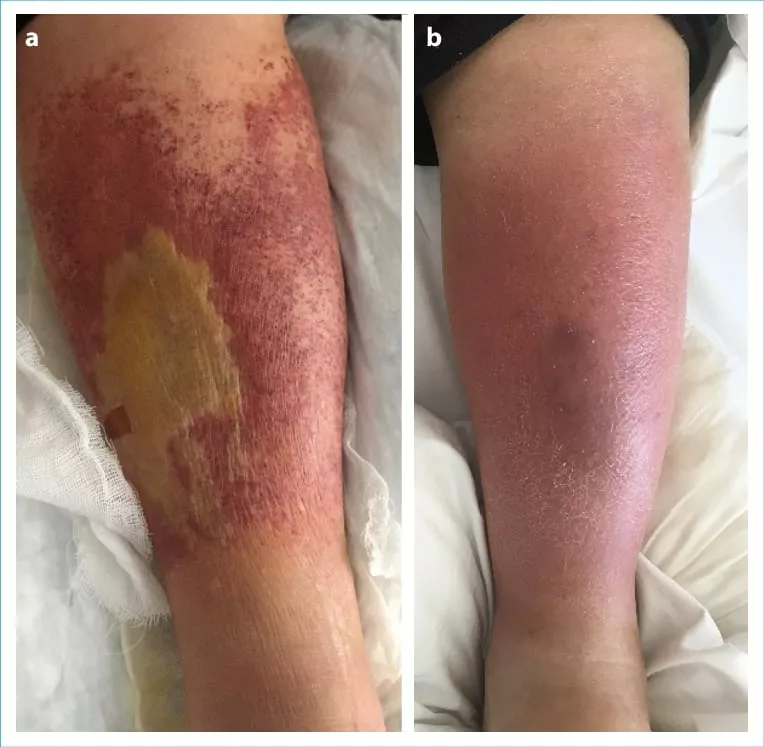
Erysipelas is a painful skin infection that affects the upper layer of the skin (dermis) and extends to the superficial cutaneous lymphatics (vessels that carry waste from tissue back to blood). The three main features that separate erysipelas rash from other skin infections include:
- A well-defined area of the lesion
- The lesion is raised above the surrounding skin
- The bright red appearance of the lesion
Erysipelas commonly affects infants, children, and elderly people. It primarily affects the lower extremities and the face, but it can occur anywhere in the body. It is also called St. Anthony’s Fire because of its intense red rash. Erysipelas spreads rapidly and is rarely fatal. The complications from erysipelas are local rather than systemic complications.1Michael Y, Shaukat NM. Erysipelas. [Updated 2023 Aug 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532247/\. Erysipelas tend to reappear if you have impaired local circulation or if there are some risk factors causing erysipelas.2Celestin, R., Brown, J., Kihiczak, G., & Schwartz, R. A. (2007). Erysipelas: a common, potentially dangerous infection. Acta dermatovenerologica Alpina, Pannonica, et Adriatica, 16(3), 123–127.
Erysipelas Vs. Cellulitis
Erysipelas and cellulitis are both bacterial skin infections but differ in their depth and severity. While making a diagnosis, symptoms of erysipelas may overlap with cellulitis. However, unlike erysipelas, cellulitis does not have well-defined borders and is slower to develop. Erysipelas respond positively to antibiotics like penicillin or erythromycin, while cellulitis may need broad-spectrum antibiotics. Proper diagnosis and timely treatment are crucial to prevent complications such as abscesses or sepsis.
Causes of Erysipelas
Erysipelas is a bacterial infection of the skin. The primary bacteria causing erysipelas is Group A Streptococci. This bacteria causes facial infection, while non-group A bacteria is involved with infection affecting the lower extremities. The most common site this bacteria affects is the leg, while the face, arms, and upper thigh are the other most common sites for developing erysipelas.3Bonnetblanc, J. M., & Bédane, C. (2003). Erysipelas: recognition and management. American Journal of Clinical Dermatology, 4(3), 157–163. https://doi.org/10.2165/00128071-200304030-00002.
This bacteria is generally present on your skin and other areas without causing any harm, but when it penetrates your skin through a cut, it can cause infection, leading to erysipelas. Commonly, the bacteria enter the body via the Athlete’s foot (fungal infection of the toes). Still, skin breaks, surgical cuts, animal bites, and ulceration are other ways by which this bacteria can enter your body. Bacteria can also spread from the skin and other areas and go to nasal passages after nasal and throat infections.
What are the symptoms of the Erysipelas?
The symptoms of the erysipelas are sudden in onset. You may begin noticing red swollen patches on your skin. The condition also forms sores and blisters called (erysipelas lesions). The infection usually appears in the skin of the lower limb, but when the face is involved, it can present with butterfly distribution on your cheeks and nose bridge. Some of the common symptoms you can experience with erysipelas are;
- The lesions are bright red and swollen
- The skin appears sharp with raised borders
- Lesions are painful, warm, and tender to touch
- Lesions may turn into blisters and, in severe cases, may turn into necrosis.
Other symptoms of erysipelas include;
- High temperature
- Chills and shivers
- Nausea or vomiting
- Headache
- Nearby lymph nodes may become swollen and tender
You may feel tired or unwell due to the body’s immune response to infection.

Risk factors of Erysipelas
The risk factors of erysipelas share with those of cellulitis and include;
- Lymphedema4Inghammar, M., Rasmussen, M., & Linder, A. (2014). Recurrent erysipelas–risk factors and clinical presentation. BMC Infectious Diseases, 14, 270. https://doi.org/10.1186/1471-2334-14-270
- Nephrotic conditions
- Pregnancy
- Conditions causing compromised immune system
- Diabetes
- Alcohol intake
- Obesity
- Eczema
- Human immunodeficiency virus (HIV)
- Recent nasopharyngeal infection
- Preexisting Chronic skin conditions that may break the skin and increase the chances of getting erysipelas (eczema, psoriasis, fungal infection)
- Injury (trauma, surgical cuts)
- Lymphatic obstruction
Diagnosis of Erysipelas
The diagnosis of the erysipelas is mainly based on clinical findings.5Bratton, R. L., & Nesse, R. E. (1995). St. Anthony’s Fire: diagnosis and management of erysipelas. American family physician, 51(2), 401–404 Generally, a doctor will diagnose the condition by looking at the appearance of your skin and the symptoms you may present. Additionally, he may ask about past and recent medical conditions and surgical procedures to get information about the cuts or incisions that may contribute to the development of the infection. He may order you to get some blood tests done to distinguish it from other conditions and to assess bacteria in the blood (bacteremia) if you have any systemic symptoms.
The blood tests may show the following;
- High white blood cell count (indicating bacterial infection or tissue damage)
- Increased C-reactive proteins (due to inflammation)
- Culture may show the presence of bacteria
What is the treatment for Erysipelas?
Oral antibiotics are the main treatment for erysipelas. The infection shows a quick and favorable response to the antibiotics. The common antibiotic doctors suggest for erysipelas is Penicillin.6Stevens, D. L., & Bryant, A. E. (2016). Impetigo, Erysipelas and Cellulitis. In J. J. Ferretti (Eds.) et al., Streptococcus pyogenes: Basic Biology to Clinical Manifestations. University of Oklahoma Health Sciences Center. The Doctor may suggest it as a sole therapy.
The recommended duration for antibiotic treatment is five days, but it may extend to ten days if the improvement is slow. Generally, a person with erysipelas may go home on oral antibiotics. Still, sometimes hospitalization is required for patients showing symptoms of necrotizing infection, immunocompromised conditions (diabetes, young children, or elderly person), and poor compliance to the treatment or a failing response to the treatment. Moreover, treating erysipelas as early as possible is important to prevent additional complications from the infection. The administration of Benzathine penicillin shows improvement when used as a preventative treatment for the recurrence of erysipelas in the future.
Supportive Treatment:
Supportive treatment, along with the medical treatment for the condition, includes;
- Hydration
- Compression stockings for swollen leg
- Elevation of the swollen leg
- Cold pack application to reduce local discomfort
- Fever medication
- Surgical debridement is performed to clean the pus when an abscess or pus is present.
- Physical Therapy in the late stages of the recovery to regain functional independence
Is the treatment for Erysipelas for the face different from other sites?
The treatment of erysipelas is the same for all infected sites, such as the face, leg, or other body parts. The same antibiotics are prescribed for all infected sites. However, extra effort is required when the case is severe. For example, if the infection causes leg swelling, then you should elevate your leg and apply a cold pack to reduce the swelling and discomfort.
The Prognosis And Outlook For Erysipelas
Usually, the outcome or prognosis of erysipelas is good. The condition is easily treatable and manageable and shows good results with antibiotics. It is managed in an outpatient setting; however, a hospital stay is needed for patients with compromised immunity, children between 3-6 years of age, and the elderly over 60 years of age. Close monitoring and observation are followed for persons who are likely to show non-compliance to treatment due to any psychological or social issues.
Complications Of Erysipelas
Up to twenty percent of patients with erysipelas show recurrence of the condition. This may be due to the persistence of risk factors and also because erysipelas damage the lymphatic system (therefore, impaired drainage of toxins), which increases the likelihood of recurrence.
The other complications may be serious but rarely fatal, including;
- Necrotic and abcessing lesion7Titou, H., Ebongo, C., Bouati, E., & Boui, M. (2017). Risk factors associated with local complications of erysipelas: a retrospective study of 152 cases. The Pan African Medical Journal, 26, 66. https://doi.org/10.11604/pamj.2017.26.66.11096
- Pneumonia
- Meningitis (Inflammation of brain tissue layers)
- Septic arthritis (Infective joint inflammation)
- Lymphedema
- Chronic leg swelling
- Septicemia (Infection of blood)
- Joint infection
- Bone infection
Prevention
Erysipelas is not always avoidable. However, taking measurable steps can help reduce the recurrence risks of this condition. Taking preventative treatment is important for prevention. Moreover, regular checkups with the doctor are crucial, as he would ensure the infection does not return or spread to other areas. Also, good hygiene is important, such as keeping the skin clean and moisturized. This will prevent cracks in the skin and prevent the entry of bacteria into the skin. Avoid scratching your skin, and seek treatment when experiencing any skin condition like athlete’s foot; if any wound or cut is present, try to clean it regularly to prevent the risk of infection.
These measures will help prevent the recurrence of erysipelas. The condition’s symptoms will disappear in a few days, but your skin will take a few weeks to reach its normal state. Also, there is no scarring (retained mark) from this condition.
Erysipelas Vs. Erysipeloid
Erysipeloid, also named Rosenbach disease, is a skin infection caused by the penetration of Erysipelothrix rhusiopathiae bacteria. Like erysipelas, the infection causes red, swollen lesions with raised and well-defined borders. However, the infection is localized to the hands and fingers, whereas erysipelas affects the face, legs, and other sites. The lesions from the erysipeloid may be asymptomatic (showing no symptoms) or cause fever, pain, and itching.8(Veraldi, S., Girgenti, V., Dassoni, F., & Gianotti, R. (2009). Erysipeloid: a review. Clinical and experimental dermatology, 34(8), 859–862. https://doi.org/10.1111/j.1365-2230.2009.03444.x).
Infection with this bacteria occurs when a person comes into direct contact with the meat of an infected animal, fish, poultry, etc. The bacteria enter the skin through a cut or wound from an infected animal and cause an infection. The condition is commonly associated with fishermen, butchers, farmers, cooks, and veterinary doctors, putting them at risk of developing erysipeloid skin conditions.
Clinical Features of Erysipeloid
Erysipeloid is commonly a localized and self-resolving condition that shows the following features;
- Well-defined red to violet lesions with smooth and shiny edges. It may expand over several days to curved borders with small blisters.
- Lesions are tender and warm to the touch
- Pain or burning sensation is present on the affected site
- The lesion mostly appears on the hands, fingers, or any exposed area of the body
- Some may experience general body pain, fever, or chill
The doctor diagnoses erysipeloid by looking at the skin lesions and asking about the occupation. He may also request various tests to diagnose and determine the extent of the infection. The condition is self-limiting and resolves itself within 2-4 weeks. However, treatment with antibiotics speeds up the healing process. The treatment protocol for erysipeloids is the same as for erysipelas. Oral antibiotic Penicillin is effective in treating this condition. Early treatment is important for quick management and prevention of serious complications of the condition.
Is Erysipelas a contagious skin condition?
Erysipelas is not a contagious condition. The infection occurs when bacteria make their way to the skin through a cut, wound, or other skin condition and develop the condition.
Conclusion
Erysipelas is a skin infection caused by group A streptococci bacteria. The symptoms are bright red rashes with well-defined borders that are raised above the surrounding healthy skin. Penicillin is the best antibiotic for this condition. Early diagnosis and treatment are important to avoid complications arising from erysipelas. The recurrence of erysipelas is common; hence, doctors advise preventative treatment to prevent its recurrence.
Refrences
- 1Michael Y, Shaukat NM. Erysipelas. [Updated 2023 Aug 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532247/\.
- 2Celestin, R., Brown, J., Kihiczak, G., & Schwartz, R. A. (2007). Erysipelas: a common, potentially dangerous infection. Acta dermatovenerologica Alpina, Pannonica, et Adriatica, 16(3), 123–127.
- 3Bonnetblanc, J. M., & Bédane, C. (2003). Erysipelas: recognition and management. American Journal of Clinical Dermatology, 4(3), 157–163. https://doi.org/10.2165/00128071-200304030-00002.
- 4Inghammar, M., Rasmussen, M., & Linder, A. (2014). Recurrent erysipelas–risk factors and clinical presentation. BMC Infectious Diseases, 14, 270. https://doi.org/10.1186/1471-2334-14-270
- 5Bratton, R. L., & Nesse, R. E. (1995). St. Anthony’s Fire: diagnosis and management of erysipelas. American family physician, 51(2), 401–404
- 6Stevens, D. L., & Bryant, A. E. (2016). Impetigo, Erysipelas and Cellulitis. In J. J. Ferretti (Eds.) et al., Streptococcus pyogenes: Basic Biology to Clinical Manifestations. University of Oklahoma Health Sciences Center.
- 7Titou, H., Ebongo, C., Bouati, E., & Boui, M. (2017). Risk factors associated with local complications of erysipelas: a retrospective study of 152 cases. The Pan African Medical Journal, 26, 66. https://doi.org/10.11604/pamj.2017.26.66.11096
- 8(Veraldi, S., Girgenti, V., Dassoni, F., & Gianotti, R. (2009). Erysipeloid: a review. Clinical and experimental dermatology, 34(8), 859–862. https://doi.org/10.1111/j.1365-2230.2009.03444.x).