Basal Cell Carcinoma is a type of cancerous lesion that most commonly targets sun-exposed areas. It is usually characterized by the formation of a painless lump or bump on the skin. It progresses slowly and destroys the surrounding skin architecture.
What is Basal Cell Carcinoma?
Basal cell carcinoma (BCC) is the most commonly present non-melanocytic skin cancer. It is also named a rodent ulcer or basalioma. It involves the basal layer of your skin in the lower part of your epidermis. The sun-exposed areas of your body are prone to this carcinoma. Therefore, the most commonly involved regions are the head and neck, but it can also involve your trunk.
It presents as a lumpy, bumpy, and pearly lesion with overlying ulceration and small blood vessels (telangiectatic vessels). This tumor spreads slowly and destroys the nearby surroundings of your skin. However, the distant spread of BCC is rare. The prognosis of this tumor is good, and it requires surgical excision.1Balakrishnan, S. (2022). Basal cell carcinoma – Pathology. Journal of Skin and Sexually Transmitted Diseases, 4, 164–170. https://doi.org/10.25259/jsstd_21_2022

How common is Basal Cell Carcinoma?
BCC is the most common skin cancer, and its incidence and frequency are increasing worldwide. It is gender specific because it affects males more than females. The male-female ratio is (2.1:1). It usually involves populations that live in high-altitude areas (Australia and South Africa) with maximum sun exposure than low-altitude areas (low-sun exposure). The incidence of BCC also increases with age. Moreover, it is more common in white people than black.
According to the American Cancer Society (ACS), the estimated incidence of basal cell carcinoma is 80% and is increasing day by day. The incidence of BCC doubles after every 25 years. This skin cancer is not fatal and rarely metastasizes. There is only a 1% chance of metastasis, unlike squamous cell carcinoma.2McDaniel, B. (2022, September 19). Basal cell carcinoma. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK482439/#:~:text=Superficial%20BCCs%20present%20as%20a,pigmented%20variants%20of%20superficial%20BCC.
Sun-Exposed Areas of your Body:
This cancer involves sun-damaged areas of your body. Therefore, it can affect the following areas of your body:
- Scalp
- Face
- Neck
- Nose
- Eyelids
- Ear
- Arms
- Legs
Clinical Variants of Basal Cell Carcinoma
Although there are about 24 different types of BCC, the most common types are:
Nodular BCC:
It is the most common type of BCC (60%). It is characterized by the formation of cystic, pigmented, keratotic, and pearly flesh-colored lesions with overlying telangiectasia.
Micronodular :
This clinical variant has a well-defined border and is usually firm. It looks yellow when stretched, but it does not cause ulceration.
Morpheaform:
It also presents as a waxy, white, or yellow sclerotic plaque with no ulceration. It usually involves the mid-facial part. Clinically, it presents as flat or depressed lesions with a firm consistency.
Superficial:
It is a less common tumor that typically involves the trunk. This carcinoma is bounded by a thread-like margin or whipcord edge. The epidermis of superficial BCC is atrophic and scaly. It clinically presents as a whitish, scaly, well-circumcised patch or plaque on the trunk.
Infiltrative BCC:
It is a marginless tumor and is difficult to diagnose. It infiltrates the basal layer of your skin.
Basosquamous Cell Carcinoma:
It is usually rare and more aggressive. It has an infiltrative growth pattern and features of both basal and squamous cell carcinoma.
Pigmented BCC:
In this variant, the skin cancer is mixed with melanin, which turns the skin darker than the surrounding.3Basal cell carcinoma: symptoms, causes, and treatment — DermNet. (n.d.). https://dermnetnz.org/topics/basal-cell-carcinoma
What causes Basal Cell Carcinoma?
It is a multifactorial disease. It includes the following causative factors:
- Gene mutation in patched tumor suppressor gene (PTCH)
- Exposure to high-frequency UV rays
- Inherited gene defects, as in Gorlin’s syndrome
Who is at risk of having BCC?
Multiple risk factors make you prone to this disease.4van Dam RM, Huang Z, Rimm EB, Weinstock MA, Spiegelman D, Colditz GA, Willett WC, Giovannucci E. Risk factors for basal cell carcinoma of the skin in men: results from the health professionals follow-up study. Am J Epidemiol. 1999 Sep 1;150(5):459-68. doi: 10.1093/oxfordjournals.aje.a010034. PMID: 10472945. These factors include the following:
- People who live in high-altitude areas are directly exposed to Ultraviolet radiation that damages their skin. This population is more prone to having this carcinoma than others.
- Arsenic exposure through ingestion is also considered a risk factor for BCC. This chemical has recently been used to treat various illnesses, including psoriasis and asthma. Ingestion of water that is contaminated with arsenic can cause basal cell carcinoma.
- The incidence of BCC is higher in immunocompromised individuals or those taking medication that suppresses their immune system (immunosuppressants).
- Xeroderma pigmentosum is an autosomal recessive disorder. This disorder is also linked with basal cell carcinoma.
- Nevoid basal cell carcinoma syndrome is an autosomal dominant disorder. People with this syndrome are also more prone to BCC.
- People with a history of Bazex syndrome can also have basal cell carcinoma
- In some studies, it was noted that alcohol consumption followed by excessive sun exposure can cause basal cell carcinoma.
- Excessive use of hydrochlorothiazide can also lead to the formation of basal cell carcinoma because this is a photosensitizer that increases your risk of having BCC.
- People with fair skin, as in albinism, are more prone to this skin cancer.
Symptoms of Basal Cell Carcinoma
In 80% of cases, this tumor affects your body’s head and scalp areas. The characteristic features of BCC are:
- Waxy papules or plaques with central depression
- Translucent
- Slowly growing
- It is painless but sometimes cause itching
- Pearly or shiny appearance
- Rolled edges or borders
- Ulceration
- Bleeding followed by trauma
- Pigmented areas due to melanin
- Overlying small blood vessels (telangiectasia)
How is Basal Cell Carcinoma diagnosed?
It is diagnosed clinically and is confirmed by a biopsy of the skin. Skin biopsy is a confirmatory test. To make a diagnosis, your doctor will take a proper history and do a physical examination.
History:
During history, your doctor will ask you some questions regarding your disease. He will ask you about the complaints that you are facing nowadays. However, other history questions include:
- When did the lesion or lump appear on your skin?
- Did this lesion change its color or size over time?
- Have you had any skin cancer diseases previously?
- Do you have any other medical illness?
Physical Examination:
After taking a history, your doctor will examine your skin lesion. He will examine the color of the lesion, surrounding skin around the lesion, consistency, size, shape, location of the tumor, and tenderness around the lesion. Additionally, he will examine your lymph nodes to check for any lymphatic spread.

Laboratory Investigations:
Laboratory investigations are usually not required but can be advised to check the patient’s health status. These investigations include:
- Complete blood count
- Liver function tests
- Viral markers
- Renal parameters (RPM)
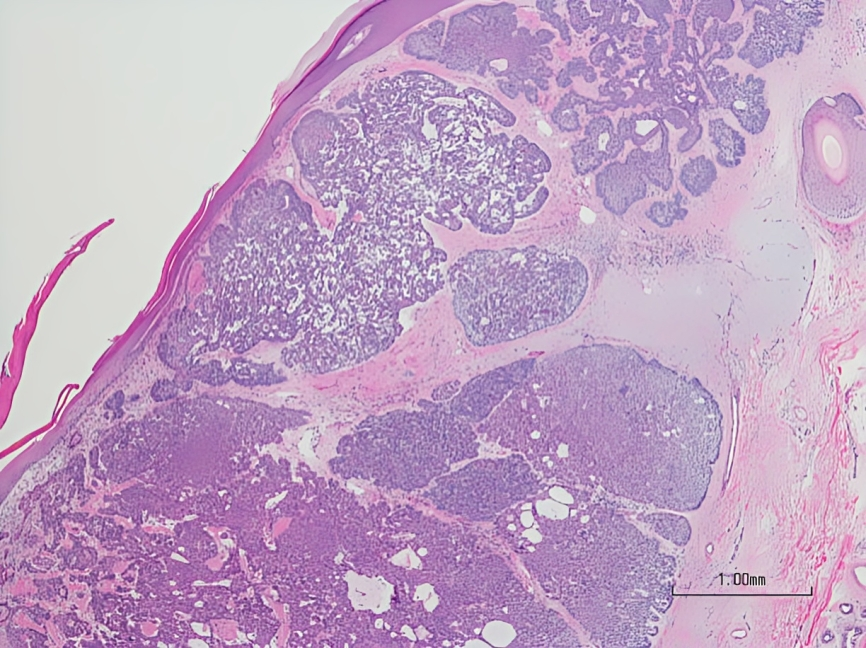
Biopsy:
A biopsy is a surgical procedure performed by a trained surgeon in which the affected and normal part of the skin is excised and sent to the pathologist for histology. Usually, shave biopsy is preferred for basal cell carcinoma. However, a punch biopsy is preferred for pigmented lesions, where the diagnosis is uncertain whether it is pigmented BCC or melanoma.
Imaging:
Imaging studies are rarely advised. However, if your doctor suspects the spread of the disease he can advise you to have an MRI or CT scan to check the spread of the disease.
Staging of Basal Cell Carcinoma
The spread of BCC is rare. Therefore, staging of basal cell carcinoma is the same as squamous cell carcinoma.5Bader, R. S., MD. (n.d.). Basal cell carcinoma: practice essentials, background, pathophysiology. https://emedicine.medscape.com/article/276624-overview#a1The staging is:
Stage 0:
In this stage, cancer is only limited to the epidermis and does not involve the dermis
Stage 1:
Cancer is small, with a size of less than 2 cm, and does not involve lymph nodes
Stage 2:
The size of the lesion is more than 2 cm and does not involve the lymph nodes
Stage 3:
Cancer involves the surrounding structure of the skin, including bone and cartilage, and also in the lymph nodes but does not spread to the organs
Stage 4:
The size of cancer can be small or large but involves other organs and lymph nodes
What are the high-risk BCCs?
The high-risk basal cell carcinomas have the following indicators:
- If the lesion is recurrent or not fully excised
- Lesions in the high-risk areas of the skin include ears, eyes, nose, nasolabial folds, vermillion border, and upper lip.
- A rapidly growing tumor (aggressive)
- Basosquamous tumors
- Tumor in immunocompromised patients
How to treat Basal Cell Carcinoma?
The treatment of basal cell carcinoma depends upon gender as well as the size, site, and type of lesion. The main goal of treating this carcinoma is:
- To completely remove the tumor to avoid recurrence
- Correction of the functional impairment
- To give the best cosmetic results
The definitive treatment of BCC is surgical excision, but some forms of BCC require pharmacotherapy or radiotherapy.
Surgical Excision:
There are various surgical procedures to correct the BCC. It includes Mohs micrographic surgery (MMS), cryosurgery, EDCs, and standard surgical excision. Mohs surgery is considered the best treatment for BCC and the best long-term cure. It is the gold standard treatment for high-risk BCC and recurrent BCC. The recurrence rate of Mohs surgery is about only 1%. During the procedure, the surgeon excises a thin layer of skin and examines it under a microscope to check for cancer cells. This process is repeated until no cancerous cells are detected, ensuring that only cancer-free tissue remains. This meticulous approach allows for complete cancer removal while preserving as much healthy tissue as possible.6Prickett KA, Ramsey ML. Mohs Micrographic Surgery. [Updated 2023 Jul 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441833/
Meanwhile, EDCs (Endocrine disruptors or endocrine-disrupting chemicals) are indicated in low-risk BCC. It is the least expensive and fastest curative method. This procedure can result in scar formation that causes cosmetic disfigurement.
Cryosurgery is another option for treating low-risk BCC. In this therapy, nitrogen is applied to the visible part of the lesion and its surrounding (normal) area. Therefore, this procedure is also indicated for those who prefer to avoid invasive surgery. It can also form a hypertrophic scar.
Radiotherapy:
Radiotherapy is advised in patients in which surgery is not an option or contraindicated. It is used as adjuvant therapy. It has some drawbacks that are:
- Costly
- Long term sessions
- Poor cosmesis
- Increased risk of cancer
- Scars of radiation therapy worsen with time instead of healing, unlike surgical scars.
Topical Therapy:
In this therapy, topical agents are applied over the affected area to treat superficial basal cell carcinoma. The FDA-approved topical agents are 5-fluorouracil (5-FU) and imiquimode 5%. However, the side effects of topical therapy include:
- Pain
- Itching
- Pruritus
- Edema
- Crusting
- Hypo and hyperpigmentation
- Skin erosions
Medical Therapy:
There are some medicines to treat basal cell carcinoma. These medicines are indicated in patients who are untreatable with other conventional therapies. However, the FDA-approved medicines that are used in BCC are vismodegib and sonidegib. The side effects of these medications are:
- Alopecia
- Muscle spasm
- Weight loss
- Diarrhea
- Fatigue
How can I prevent Basal Cell Carcinoma?
It is the most common skin tumor that usually involves the population having fair skin and also has a positive family history of BCC or SCC. Sunlight is considered the prime cause of this carcinoma. Moreover, there are some preventive measures that you can adopt to lower your risk of developing cancer. These include7Nambudiri, V. E. (2024, February 21). Basal cell carcinoma. MSD Manual Professional Edition. https://www.msdmanuals.com/professional/dermatologic-disorders/cancers-of-the-skin/basal-cell-carcinoma
- Avoid exposure to the sun, wear gloves and hats, and cover your body
- Avoid the use of tanning beds
- Apply sunscreen of SPF 30 or 60 or more on the sun-exposed areas of your body if you are planning to go outside activities.
- A regular visit to your doctor
- Taking vitamin B3 regularly can lower the risk of BCC
- Avoid drinking alcohols
Prognosis of Basal Cell Carcinoma
Basal carcinoma is a rare cancer and is not fatal. The potential risk of BCC depends upon its recurrence rate. Moreover, the risk depends upon the location of the cancer and its histological type.8Dika, E., Scarfì, F., Ferracin, M., Broseghini, E., Marcelli, E., Bortolani, B., Campione, E., Riefolo, M., Ricci, C., & Lambertini, M. (2020). Basal Cell Carcinoma: A Comprehensive Review. International journal of molecular sciences, 21(15), 5572. https://doi.org/10.3390/ijms21155572
Risk according to Location:
- Trunk lesions are considered low-risk lesions
- Lesions on the cheeks, neck, forehead, and scalp have an intermediate risk
- The nose, ears, centrofacial areas, and periorificial areas are high-risk areas
Prognosis of the Tumor:
Good Prognosis
- Primary superficial BCC
- Primary Nodular BCC
Intermediate Prognosis
- Recurrent superficial BCC
- Nodular BCC
Poor Prognosis
- Nodular BCC with a size of more than 1 cm in a high-risk location
- Morpheaform BCC
- Infiltrative BCC
- Basosquamous cell carcinoma
Actinic Keratosis Vs. Basal Cell Carcinoma:
Actinic keratosis also develops in sun-exposed areas and most commonly involves the scalp. Moreover, it is characterized by dry, scaly patches followed by sun damage. It is a precancerous lesion.
Basal cell carcinoma involves the basal layer of the skin in sun-damaged areas. It is characterized by waxy, shiny, lumpy, and scaly lesions.
Basal Cell Carcinoma Vs. Melanoma
Unlike basal cell carcinoma (BCC), Melanoma is a highly aggressive form of skin cancer originating from melanocytes, the cells responsible for producing skin pigment. It is known for its potential to spread rapidly to other body parts, making it more dangerous than BCC. Melanoma often appears as a new, unusual-looking mole or changes in an existing mole, typically with irregular borders and multiple colors. While BCC grows slowly and rarely metastasizes, melanoma requires prompt diagnosis and treatment to prevent it from spreading. Early detection is critical, as melanoma can be life-threatening if not caught and treated in its early stages.
Conclusion
To conclude, basal cell carcinoma or basalioma is a lesion involving the basal layer of your skin. It has many variants. Characteristic features of this tumor are waxy papules with depression in the center, bleeding on trauma, ulceration, translucency, and rolled margins. The biopsy of the lesion is a confirmatory test for BCC. Moreover, the treatment and prognosis of basal cell carcinoma depend on the variant of BCC and the stage of the disease. Therefore, primary superficial BCC and primary Nodular BCC have a good prognosis.
Refrences
- 1Balakrishnan, S. (2022). Basal cell carcinoma – Pathology. Journal of Skin and Sexually Transmitted Diseases, 4, 164–170. https://doi.org/10.25259/jsstd_21_2022
- 2McDaniel, B. (2022, September 19). Basal cell carcinoma. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK482439/#:~:text=Superficial%20BCCs%20present%20as%20a,pigmented%20variants%20of%20superficial%20BCC.
- 3Basal cell carcinoma: symptoms, causes, and treatment — DermNet. (n.d.). https://dermnetnz.org/topics/basal-cell-carcinoma
- 4van Dam RM, Huang Z, Rimm EB, Weinstock MA, Spiegelman D, Colditz GA, Willett WC, Giovannucci E. Risk factors for basal cell carcinoma of the skin in men: results from the health professionals follow-up study. Am J Epidemiol. 1999 Sep 1;150(5):459-68. doi: 10.1093/oxfordjournals.aje.a010034. PMID: 10472945.
- 5Bader, R. S., MD. (n.d.). Basal cell carcinoma: practice essentials, background, pathophysiology. https://emedicine.medscape.com/article/276624-overview#a1
- 6Prickett KA, Ramsey ML. Mohs Micrographic Surgery. [Updated 2023 Jul 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441833/
- 7Nambudiri, V. E. (2024, February 21). Basal cell carcinoma. MSD Manual Professional Edition. https://www.msdmanuals.com/professional/dermatologic-disorders/cancers-of-the-skin/basal-cell-carcinoma
- 8Dika, E., Scarfì, F., Ferracin, M., Broseghini, E., Marcelli, E., Bortolani, B., Campione, E., Riefolo, M., Ricci, C., & Lambertini, M. (2020). Basal Cell Carcinoma: A Comprehensive Review. International journal of molecular sciences, 21(15), 5572. https://doi.org/10.3390/ijms21155572