Fulminant hepatic failure or FHF is a serious condition in which your liver suddenly shuts down, without any history of liver disease. Affecting around 1-6 people per million annually,1Bernal, W., & Wendon, J. (2013). Acute liver failure. New England Journal of Medicine, 369(26), 2525-2534 FHS is extremely rare. But here’s the real danger: if you don’t seek treatment in time, it can become deadly. Due to its sudden development and aggressive progression, the importance of early recognition and intervention cannot be over-emphasized.
Fulminant Hepatic Failure vs. Acute Liver Failure
While most people use these two terms interchangeably, there is a technical difference between Acute Liver Failure (ALF) and Fulminant Hepatic Failure (FHF) that you should know:
Acute liver failure is a broad entity that refers to the sudden cessation of liver function in people who have never had any liver disease. It is recognized by an International Normalization Ratio (INR) of more than 1.5 and the development of hepatic encephalopathy within 26 weeks of symptoms onset. It is further categorized into Fulminant and subfulminant hepatic failure:
1. Fulminant hepatic failure is a type of ALF in which encephalopathy develops within 8 weeks of symptom onset.2Ng, W., Norton, I. D., & Jones, D. (2004). 13. FULMINANT HEPATIC FAILURE. In Principles of medical biology (pp. 361–382). https://doi.org/10.1016/s1569-2582(04)15013-7
2. Subfulminant hepatic failure is a relatively less aggressive type of ALF in which encephalopathy takes longer than 8 weeks to set in.
Pathophysiology: How Does Fulminant Hepatic Failure Occur?
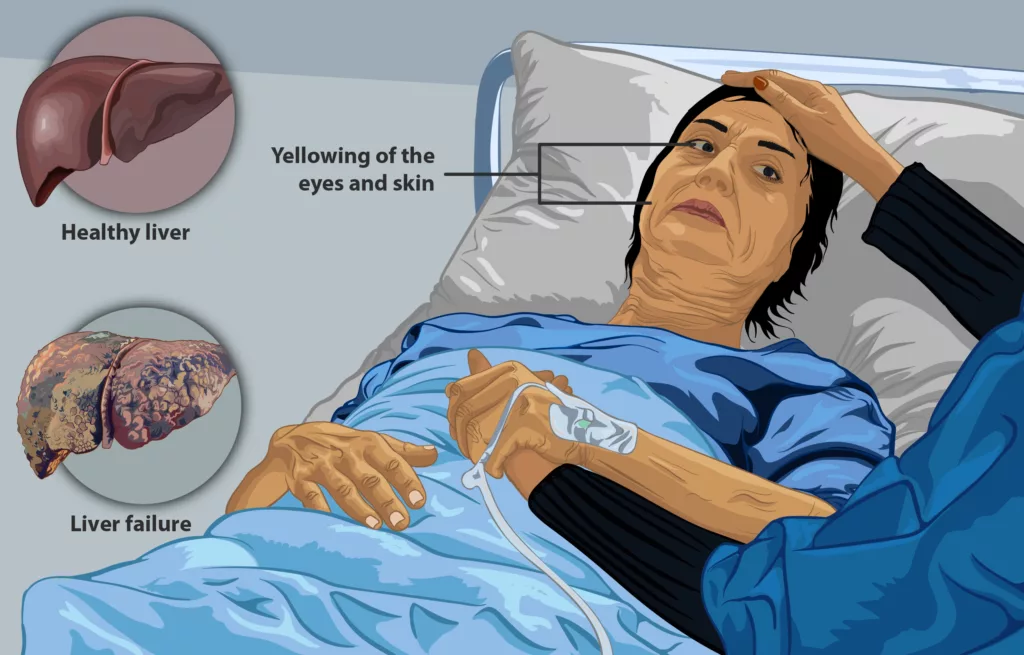
Our liver is responsible for several vital functions, including detoxification, protein synthesis, coagulation, and bile production. In FHF, when our liver cells encounter any insult due to viruses or toxins, all these vital processes stop working. This causes the accumulation of toxic substances such as ammonia, in the blood, leading to mental dysfunction or hepatic encephalopathy. The failure of coagulation results in clotting issues (Coagulopathy) like easy bruising and uncontrolled bleeding. Furthermore, impaired production of bile gives rise to the build-up of bilirubin which manifests as yellowing of skin and sclera – medically referred to as ‘jaundice’. Apart from this, since toxins spread throughout the body, they also affect other organs such as the kidneys, heart, or the brain.
What are the characteristics of Fulminant Hepatic Failure?
The cardinal characteristics of fulminant hepatic failure are:
- Hepatic encephalopathy: it’s the development of confusion, personality changes, disorientation, and coma, secondary to a build-up of toxins in the blood.
- Jaundice: It’s the appearance of a yellowish hue in your skin and eyeballs, due to bilirubin accumulation.
- Coagulopathy or impaired clotting: It is the inability of the liver to produce clotting factors. Our bodies exhibit it as quick bruising, excessive blood loss, and fatal internal bleeding.
These characteristics often escalate rapidly, highlighting the critical role of early diagnosis and treatment.
How Common is Fulminant Hepatic Failure?
The prevalence of FHF varies from region to region, depending upon local disease patterns, status of sanitation, and access to healthcare. If we talk about the developed countries, it affects 1-6 people per million every year.3Bernal, W., & Wendon, J. (2013). Acute liver failure. New England Journal of Medicine, 369(26), 2525-2534. In the developing world where access to healthcare may still be a privilege, and viral infections are quite endemic, the incidence of FHF is even higher.
Moreover, we should know that out of all liver transplants being done globally, 6-8% are solely due to FHF. Again, it highlights how serious a condition FHF is, and how liver transplantation is a life-saver.4Polson, J., & Lee, W. M. (2005). AASLD position paper: The management of acute liver failure. Hepatology, 41(5), 1179-1197
What are the Causes of Fulminant Hepatic Failure?
Out of various causes of FHF, drug-induced liver injury is the most common one in the developed world, contributing to 60-70% of the cases.5Stravitz, R. T., & Lee, W. M. (2019). Acute liver failure. The Lancet, 394(10201), 869-881. In developing nations, especially in sub-Saharan Africa and South Asia, the prime culprit is viral hepatitis. Determining the underlying cause is an important step in deciding the course of treatment and predicting the prognosis:
Viral Hepatitis
Hepatitis A and E are the most common causes of FHF in third-world countries. Since they spread through contaminated food or water, the prevalence is quite high in regions with poor sanitation. Hepatitis B, though less common, can also cause FHF. Similarly, Hep B-positive individuals who get co-infected with hep D are also vulnerable.
Drug-Induced Liver Injury
Overdoses of Acetaminophen (popular brand names Tylenol and Paracetamol) are the prime culprits of FHF in developed countries. Reports confirm that it contributes to 56,000 emergency visits, 2600 hospitalizations, and 500 deaths annually in the US. Other medications like anti-seizure drugs, some antibiotics, and herbal treatments have also been found to trigger FHF.
Autoimmune Hepatitis
Sometimes our immune system gets out of control and starts attacking cells of our liver. It produces inflammation and can aggravate to shut our liver down. This condition is called Autoimmune hepatitis. It’s more common in women and often requires immunosuppressive treatment.
Toxins and Poisons
Amanita Phalloides, commonly known as the Death Cap mushroom, is infamous for causing FHF. It produces hepatotoxins that cause serious liver damage within hours of ingestion.

Other poisonous substances that lead to FHF include:
- Industrial chemicals such as carbon tetrachloride, vinyl chloride
- Heavy metals like arsenic, lead and mercury
- Several pesticides, including organochlorines
Genetic and Metabolic Disorders
- Wilson’s disease is a rare genetic disorder linked to faulty copper metabolism in the body. In this disease, the consequent copper accumulation in the liver leads to FHF.
- Reye’s syndrome is another cause of FHF, which is marked by brain and liver swelling. It arises secondary to the consumption of aspirin, particularly in children affected by viral illnesses.
Pregnancy-Related Complications
- HELLP syndrome is a rare pregnancy complication that typically manifests as hemolysis, elevated liver enzymes, and a low platelet count. While we do not know the cause of HELLP yet, it also gives rise to FHF.
- Another pregnancy-related cause of FHF is the Acute Fatty Liver of Pregnancy.6Mazzola, A., Magro, B., Perdigao, F., Charlotte, F., Atif, M., Goumard, C., Scatton, O., & Conti, F. (2021). Acute liver failure and HELLP syndrome: A clinical case and literature review. Clinics and Research in Hepatology and Gastroenterology, 45(2), 101498. https://doi.org/10.1016/j.clinre.2020.07.005
Both these conditions are a medical emergency and may even require prompt delivery of the baby in severe cases.
What are the symptoms of Fulminant Hepatic Failure?
The symptoms of fulminant hepatic failure vary from mild discomfort to life-threatening complications.
In the beginning, there might be just mild symptoms like:
- Malaise and fatigue
- Nausea, vomiting
- Loss of appetite
- Jaundice
- Pruritus
- Right Upper Quadrant Pain

But as the toxins accumulate in your bloodstream, they start affecting your brain, producing neurological symptoms of hepatic encephalopathy, like:
- Confusion
- Irritability
- Mood swings
- Difficulty concentrating
- Memory issues
- Asterexis or flapping tremors of the hands – a classical sign of hepatic encephalopathy
These symptoms often progress rapidly to:
- Coma or profound neurological deficits
- Fluid build-up in the abdomen is known as ascites. It causes discomfort and swelling
- Unprovoked bleeding or bruising
Complications of Fulminant Hepatic Failure
Fulminant hepatic failure results in severe complications, most of which require urgent medical attention. These include:
- Cerebral edema: It’s swelling of the brain secondary to toxins accumulation. It can increase intracranial pressure and the likelihood of brain herniation.7Vaquero, J., Chung, C., & Blei, A. T. (2019). Brain edema in acute liver failure: A window to the pathogenesis of hepatic encephalopathy. Annals of Hepatology, 18(4), 720–730. https://doi.org/10.1016/S1665-2681(19)32153-2
- Sepsis: It’s a widespread infection, that occurs secondary to a faulty immune system
- Hepatorenal Syndrome: It refers to severe liver failure accompanied by kidney dysfunction, due to extreme narrowing of our renal arteries.
- Cardiovascular instability: It manifests as low blood pressure, compromised blood supply to the organs, and disrupted heart rhythms.
- Multiorgan failure: As our liver shuts down, other organs (including kidneys, the heart, and the brain) may also fail, producing multi-organ failure.
When Should You Seek Medical Attention?
Remember, fulminant hepatic failure is a medical emergency. You must seek immediate medical care if you or someone you know experiences:
- Severe confusion, irritability, or drowsiness
- Easy bruising or unexplained blood loss
- Rapid-onset jaundice
The sooner you seek treatment, the higher your chances of survival.
How is Fulminant Hepatic Failure Diagnosed?
Fulminant hepatic failure is diagnosed by combining clinical evaluation, lab investigations, and imaging.
Clinical History & Examination:
First, the doctor will assess your medical history. He will especially ask you about:
- Recent medication or alcohol use.
- Potential exposure to viral infections or hepatotoxic substances (such as certain mushrooms or organic solvents)
- Symptoms like jaundice, confusion, or unexplained bleeding.
- A family history of liver disease, particularly genetic conditions like Wilson’s disease, is also considered.
Then, the doctor will examine you thoroughly to look for any evidence of pre-existing liver disease. He will also assess the severity of hepatic encephalopathy.
Laboratory tests:
Your doctor might ask for these lab tests to further identify the cause and guide treatment for FHF. The typical results of lab tests in the case of FHF are:
- Liver Function Tests (LFTs): Elevated ALT, AST, and bilirubin levels
- Coagulation Profile: Prolonged prothrombin time (PT) and INR
- Ammonia Levels: Elevated
- Blood Glucose levels may be critically low
- Complete blood count (CBC) often reveals thrombocytopenia
- Blood Culture & Viral Serologies: Used to detect infections, including hepatitis viruses, CMV, or HSV in immunosuppressed patients.
Imaging:
You might have to undergo the following imaging studies:
- Ultrasound: to identify structural abnormalities or the presence of ascites.
- MRI: to rule out other causes of liver dysfunction, such as tumors. It also provides a clearer picture in case of massive ascites or obesity, or if transplantation is being planned.
- CT Brain: to rule out other causes for the decline in mental function such as intracranial masses.
Liver Biopsy:
People with FHF are already at a higher risk for spontaneous bleeding. So, doctors rarely perform a liver biopsy on these patients. But if at all, a transjugular biopsy may be considered a safer alternative, especially in cases of diagnostic uncertainty.
Treatment Options for Fulminant Hepatic Failure
The treatment options for fulminant hepatic failure can be categorized into supportive measures, targeted therapies, and definitive treatment options. Doctors mainly focus on urgent intervention to stabilize the patient, treat the underlying cause, and prevent deadly complications.
Supportive Care:
- Patients with grade 2 encephalopathy should be transferred to the Intensive Care Unit (ICU). The staff should continuously monitor the patient’s vital signs, baseline labs, and neurological status. Also, intubation is necessary to protect the airway in patients with advanced encephalopathy.
- If there is evidence of any hemodynamic instability, the medical staff should pay careful attention to fluid management.
- As patients with FHF often have clotting abnormalities, fresh frozen plasma (FFPs), recombinant factor VIIa, and platelet transfusion may be considered.
Targeted Therapy:
These include antidotes and other substances that directly act against the causative agents, like:
- N-acetylcysteine (NAC) for acetaminophen poisoning
- Intravenous penicillin G for mushroom poisoning
- Intravenous mannitol or hypertonic saline to reduce brain swelling
- Intravenous glucose to prevent or treat hypoglycemia
- A high-calorie, low-protein diet to limit ammonia production, hence alleviate hepatic encephalopathy
Definitive Treatment: Liver Transplantation
The definitive treatment for irreversible FHF is liver transplantation, with a proven success rate of 80% if performed timely.8Trey, C., & Davidson, C. S. (1970). The management of fulminant hepatic failure. Progress in Liver Diseases, 3, 282-298.
Fulminant Hepatic Failure Criteria for Liver Transplant:
There is often a scarcity of available organs, raising ethical concerns and questioning treatment decisions for patients of irreversible FHF. This is why King’s College developed criteria to help determine which patients require urgent transplantation. According to these criteria, doctors should consider a patient for liver transplantation if they meet three or more of the following:
- Age less than 10 or greater than 40 years
- FHF due to non-A, non-B, non-C hepatitis, halothane hepatitis, or idiosyncratic drug reactions
- Jaundice for more than a week before the onset of encephalopathy
- Prothrombin time (PT) longer than 50 seconds
- Serum bilirubin levels higher than 300 mmol/L (17.5 mg/dL)
Also, patients with a PT longer than 100 seconds should be prioritized for immediate transplantation.
Living Donor Transplants:
Doctors may also consider transplanting a portion of a healthy liver from a living donor, in specific scenarios.
Artificial Liver Support Systems:
Due to the unavailability of donated livers, patients often have to wait a long time for liver transplantation. In such cases, the patients can get temporary support from artificial liver systems. These systems act by filtering toxins and by stabilizing metabolic function. They can further be categorized into biological and nonbiological systems.
- Biological or bioartificial contain hepatocyte-filled cartridges. Scientists are exploring them for their role in liver regeneration.
- Non-biological liver systems assist in removing toxins but do not have any role in liver regeneration. Examples are plasmapheresis and hemodialysis.
One well-studied artificial support system is MARS or the Molecular Adsorbent Recirculating System. It uses an albumin-impregnated membrane to remove toxins from the blood. According to scientific evidence, it helps reduce hyperalbuminemia and encephalopathy and improves short-term results.9Yarrarapu SNS, Sanghavi DK. Molecular Absorbent Recirculating System. [Updated 2023 May 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK555939/
Prometheus and single-pass albumin dialysis (SPAD) are other emerging treatment options, but they are still being investigated.
Prevention of Fulminant Hepatic Failure
To prevent FHF, we need to adopt a few important measures – some at the individual level and others at a communal or state level:
- Vaccinate yourself against viral hepatitis
- You should always consult licensed healthcare providers before you start any new medication. Also, never take any medication beyond the recommended dose.
- Public health and municipal bodies, particularly in developing countries, should work to improve sanitation and provide access to clean water. These measures would limit hep A and E spread, and prevent FHF secondary to viral hepatitis.
Fulminant Hepatic Failure Mortality & Prognosis
Years back, people looked at fulminant hepatic failure as a near-certain death sentence. At that time, liver transplantation wasn’t an option and the mortality rates exceeded 80%.10Ferenci, P. (2005). Hepatic encephalopathy. Gastroenterology Clinics of North America, 34(3), 641-659.
But this isn’t the case anymore. Today, orthotopic liver transplantation (OLT) and advancements in intensive care have improved survival rates up to 60%.
Having said this, you may witness prognosis varying from case to case, depending upon the underlying cause and severity of complications.
For example, FHF due to acetaminophen toxicity shows a better prognosis, as compared to FHF secondary to Wilson’s disease or unknown causes. Similarly, the presence of complications such as cerebral edema, severe coagulopathy, and renal failure also signal a poor prognosis.
Key prognostic markers include:
- Arterial pH levels: A lower pH level or metabolic acidosis is linked with a poor outcome.
- Coagulation profile: Prognosis is also compromised in case of prolonged prothrombin time (PT).
- Grade of encephalopathy: Doctors have seen a higher risk of mortality with advanced stages.
Unfortunately, patients having a slower disease course exhibit poor outcomes as compared to those who progress from jaundice to encephalopathy within two weeks (patients with hyperacute liver failure).At the end of the day, early diagnosis, intensive medical management, and timely liver transplantation remain the most effective strategies to improve survival in FHF patients.
FHF in Children vs. Adults: Key Differences
There are distinct differences between fulminant hepatic failure in children as compared to that in adults:
- While encephalopathy is the hallmark of FHF in adults, children might not show signs of encephalopathy until late or at all, in half of the cases.
- The cause of FHF in children is often unknown, with drug-induced liver damage being much rarer. This is contrary to FHF in adults, where drug-induced liver injury remains the most common cause.
- In addition to the investigations required for diagnosing FHF in adults, children also need to undergo metabolic or genetic testing. This is done to proactively diagnose underlying mitochondrial conditions, which may not improve with a liver transplant.
- There is also a difference in both about key prognostic markers. King’s College criteria directs us to prioritize children younger than 2.5 years, who have elevated INR, bilirubin, and WBC count. It’s because they face a higher risk of death without timely transplantation.11Dhawan, A., Cheeseman, P., & Mieli-Vergani, G. (2004). Approaches to acute liver failure in children. Pediatric transplantation, 8(6), 584–588. https://doi.org/10.1111/j.1399-3046.2004.00292.x
Conclusion
In conclusion, fulminant hepatic failure or FHF is a serious condition characterized by jaundice, encephalopathy, and coagulation abnormalities. It’s rare yet life-threatening and necessitates urgent identification and treatment. Common causes of FHF include acetaminophen toxicity and viral hepatitis. Diagnosis involves clinical evaluation, laboratory tests, and imaging studies. While liver transplantation remains the gold standard treatment, we can’t undermine the role of supportive care. Preventative strategies include vaccination against viral hepatitis, safer use of medication, and public health measures such as improved sanitation. Without treatment, mortality rates are high. However, timely intervention does improve survival rates significantly.
Refrences
- 1Bernal, W., & Wendon, J. (2013). Acute liver failure. New England Journal of Medicine, 369(26), 2525-2534
- 2Ng, W., Norton, I. D., & Jones, D. (2004). 13. FULMINANT HEPATIC FAILURE. In Principles of medical biology (pp. 361–382). https://doi.org/10.1016/s1569-2582(04)15013-7
- 3Bernal, W., & Wendon, J. (2013). Acute liver failure. New England Journal of Medicine, 369(26), 2525-2534.
- 4Polson, J., & Lee, W. M. (2005). AASLD position paper: The management of acute liver failure. Hepatology, 41(5), 1179-1197
- 5Stravitz, R. T., & Lee, W. M. (2019). Acute liver failure. The Lancet, 394(10201), 869-881
- 6Mazzola, A., Magro, B., Perdigao, F., Charlotte, F., Atif, M., Goumard, C., Scatton, O., & Conti, F. (2021). Acute liver failure and HELLP syndrome: A clinical case and literature review. Clinics and Research in Hepatology and Gastroenterology, 45(2), 101498. https://doi.org/10.1016/j.clinre.2020.07.005
- 7Vaquero, J., Chung, C., & Blei, A. T. (2019). Brain edema in acute liver failure: A window to the pathogenesis of hepatic encephalopathy. Annals of Hepatology, 18(4), 720–730. https://doi.org/10.1016/S1665-2681(19)32153-2
- 8Trey, C., & Davidson, C. S. (1970). The management of fulminant hepatic failure. Progress in Liver Diseases, 3, 282-298.
- 9Yarrarapu SNS, Sanghavi DK. Molecular Absorbent Recirculating System. [Updated 2023 May 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK555939/
- 10Ferenci, P. (2005). Hepatic encephalopathy. Gastroenterology Clinics of North America, 34(3), 641-659.
- 11Dhawan, A., Cheeseman, P., & Mieli-Vergani, G. (2004). Approaches to acute liver failure in children. Pediatric transplantation, 8(6), 584–588. https://doi.org/10.1111/j.1399-3046.2004.00292.x

