What is Herpetic Whitlow?
Herpetic whitlow is a painful skin condition characterized by the formation of vesicles and blisters on fingernails. This contagious disease is caused by the herpes simplex virus (HSV) infection. The dermal disease is usually self-limiting but may require antiviral medication for complete resolution. Reports suggest it has a global incidence of 2.4 cases/100,000 people per year.1Betz, D., & Fane, K. (2023). Herpetic whitlow. In StatPearls [Internet]. StatPearls Publishing.

Herpetic Whitlow Stages
Herpetic Whitlow typically progresses through several stages, from initial infection to resolution. Understanding these stages can help recognize and manage the condition effectively.
Pain And Burning
The prodromal stage of infection is characterized by fever and malaise. Later, there is pain, burning, and tingling sensations on the fingertip. Some patients also report changes in skin color, i.e., reddening. This stage lasts for 1 to 2 days.
Vesicle/Blister Formation
In the next stage, groups of clear vesicles/blisters form on a red base, having a diameter of 1-3mm. The vesicles are erythematous (red), edematous (pus-filled) and painful.
Ulceration Of Blisters
5-6 days after infection, the vesicles coalesce to form honey-like bullae, which then ulcerate. The ruptured blisters release a clear or yellowish exudate. The lesions can spread to different areas of the skin (nail bed, etc.).
Scabbing & Crustation
Some days later, the blisters start to scab and crust. Scabbing marks the start of the healing, and the whitlow usually self-resorbs within 10-14 days. However, in some cases, healing may take 2-4 weeks.
Herpetic Whitlow Causes
Whitlow’s finger develops when the herpes simplex virus (HSV) enters the finger skin through an open/cut region. Both strains of the HSV, HSV-1, and HSV-2, can cause herpetic whitlow. HSV-1 is the causative agent for cold sores, while HSV-2 is the culprit for genital herpes.
Herpetic Whitlow Symptoms
In almost all cases, symptoms do not appear suddenly. It takes 2-20 days after infection for the first symptoms to develop. The most commonly reported symptoms of herpetic whitlow include:
Blisters:
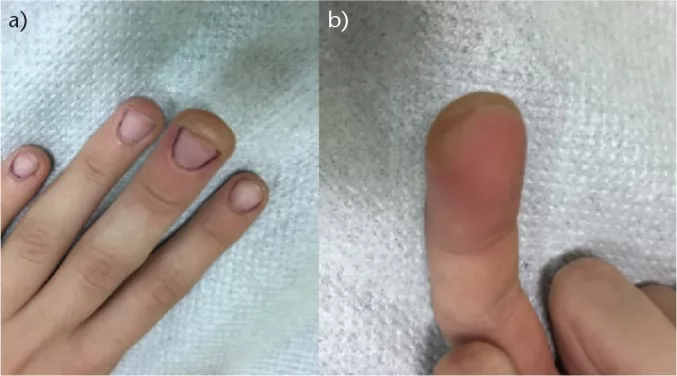
Fluid-filled vesicles form on the skin surrounding your fingernail. The vesicles exist in small groups and may affect any finger. The raised bumps generally have clear or yellow fluid/exudate inside. The blisters cause burning/tingling pain and may limit movement.
Color change:
The skin under the blisters may change color. Patients report fingernail skin to be red to purple. In a case study, a swollen, purple, and blistered thumb was diagnosed as herpetic whitlow.2Cohen, B. A. (2023). Swollen, purple, blistered thumb leads to diagnosis of herpetic whitlow. Contemporary Pediatrics, 40(5), 36-38.
Swelling:
Swollen fingers are commonly seen in whitlow.
Fever and swollen lymph nodes: Several patients also report fever and swelling of lymph nodes associated with Whitlow’s finger.

Is Herpetic Whitlow Contagious?
Yes, like other herpes infections (genital herpes and cold sores), herpetic whitlow is contagious. You can contract the disease if open skin (cut) or sore on a finger comes in contact with the sore/blister of an infected person. Transmission is common from one person to another.
You can self-transmit an HSV infection elsewhere to your fingers. If an open cut on your finger skin comes in contact with the affected skin of the face (HSV-1) or genitals (HSV-2), whitlow ensues. The virus in your facial and genital skin moves through the open wounds.3Whitley, R. J., & Roizman, B. (2023). Epidemiology, clinical manifestations, and diagnosis of herpes simplex virus type 1 infection. In UpToDate. Retrieved June 19, 2024, from https://www.uptodate.com/contents/epidemiology-clinical-manifestations-and-diagnosis-of-herpes-simplex-virus-type-1-infection?search=herpetic%20whitlow&source=search_result&selectedTitle=1%7E20&usage_type=default&display_rank=1#H13886328
Risk Groups For Herpetic Whitlow
Certain individuals and professionals are at greater risk of developing Whitlow’s finger due to frequent contact of hands/fingers with oral mucosa and genital skin. The list includes:
- Thumb suckers (children)
- Patients with weak immunity (such as HIV/AIDS patients, individuals on chemotherapy and immunosuppressants, etc.)
- Dentists, dental hygienists, respiratory therapists
- Wrestlers, boxers (because they have close contact with each other’s facial skin)

Herpetic Whitlow Diagnosis
Your healthcare provider will physically examine the lesions and correlate them with the history and symptoms. The unique location and signs of the disease make it easier to diagnose. However, the doctor may order a viral culture test or a PCR test to confirm the diagnosis.
A viral culture test helps identify the type of virus present in the skin lesion, while a PCR test looks for genes from the virus (herpes). Both tests take a small sample off the lesion using a swab.
Herpetic Whitlow Differential Diagnosis
Few conditions in presentation resemble herpetic whitlow. Impetigo and blistering dactylitis appear similar to whitlow. However, the condition most commonly mistaken for whitlow is paronychia.
Herpetic Whitlow Vs. Paronychia
Paronychia is a skin condition in which an abscess forms in the nail fold. Unlike the viral whitlow, paronychia develops due to a bacterial infection. It usually involves the fingernails (proximal and lateral fingernails) and is one of the most common hand infections.4Feder HM Jr, Long SS. Herpetic whitlow. Epidemiology, clinical characteristics, diagnosis, and treatment. Am J Dis Child. 1983 Sep;137(9):861-3. doi: 10.1001/archpedi.1983.02140350035009. PMID: 6613951.

Herpetic Whitlow Vs. Felon
A felon finger is another infectious condition that falls under the differential diagnosis of herpetic whitlow. Felon presents as pain, redness, and swelling of the pad of the fingertip (infection of fingertip pulp). A bacterial infection causes felons. The closed-space infection can lead to severe throbbing pain.5Nardi NM, McDonald EJ, Syed HA, et al. Felon. [Updated 2024 Apr 30]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430933/
Herpetic Whitlow Treatment
In almost all cases, the disease resolves on its own. The vesicles start to heal as soon as the body produces antibodies in response to the virus. However, immunocompromised patients may need medical aid.
Treatment is divided into symptomatic management and viral load management. Doctors generally prescribe over-the-counter painkillers (naproxen, ibuprofen, etc.) for pain management. You will need to take antiviral medications to reverse the viral infection’s effects. Mostly, topical antivirals are sufficient to bring about the desired results. But sometimes, oral antivirals are also needed.
Studies show that acyclovir is pretty effective, leads to complete resolution of symptoms, and causes no recurrence of the disease.6Brkljac, M., Bitar, S., & Naqui, Z. (2014). A case report of herpetic whitlow with positive Kanavel’s cardinal signs: a diagnostic and treatment difficulty. Case Reports in Orthopedics, 2014. Healthcare workers advise patients to apply bandage compressions along with topical antivirals (acyclovir) a couple of times a day.7Schwandt NW, Mjos DP, Lubow RM. Acyclovir and the treatment of herpetic whitlow. Oral Surg Oral Med Oral Pathol. 1987 Aug;64(2):255-8. doi: 10.1016/0030-4220(87)90100-9. PMID: 2957639.
Home Management
Once diagnosed, you should immediately cover the wound with a non-stick bandage. This maneuver protects and prevents the spread of infection (secondary infection). A bandage on the blisters also acts as a mild compress that promotes early rupturing and, consequently, early healing.8Patel, Asha & Romanelli, Paolo & Roberts, Brenda & Kirsner, Robert. (2007). Treatment of Herpes Simplex Virus Infection. Advances in skin & wound care. 20. 408-12. 10.1097/01.ASW.0000280199.58260.62.
How Can I Prevent Whitlow’s Finger?
Individuals in high-risk groups (HSV infected, dentists, etc.) must take extra precautions to keep whitlow at bay. You can adopt the following simple steps to keep yourself safe:
- Wear gloves while working in close proximity to the patient (or when hands come in contact with people’s mouths).
- Frequently wash hands with anti-bacterial soaps.
- Stop the finger (thumb) sucking habits of your children.
- Mothers should wash their hands before feeding adolescents.
Final Word
Herpetic whitlow is a viral infection of the fingernail that usually affects those with weak immunity. Caused by the Herpes simplex virus (HSV), whitlow can develop in cold sores (HSV-1) and genital herpes (HSV-2) patients. The virus spreads from the infected skin through a cut/open wound in the finger skin. It causes finger swelling, painful blisters, and vesicles that crust and heal within a few weeks. Patients rarely need antiviral medicines (such as acyclovir) because the disease resolves itself, and you can prevent it by wearing gloves and washing hands frequently.
Refrences
- 1Betz, D., & Fane, K. (2023). Herpetic whitlow. In StatPearls [Internet]. StatPearls Publishing.
- 2Cohen, B. A. (2023). Swollen, purple, blistered thumb leads to diagnosis of herpetic whitlow. Contemporary Pediatrics, 40(5), 36-38.
- 3Whitley, R. J., & Roizman, B. (2023). Epidemiology, clinical manifestations, and diagnosis of herpes simplex virus type 1 infection. In UpToDate. Retrieved June 19, 2024, from https://www.uptodate.com/contents/epidemiology-clinical-manifestations-and-diagnosis-of-herpes-simplex-virus-type-1-infection?search=herpetic%20whitlow&source=search_result&selectedTitle=1%7E20&usage_type=default&display_rank=1#H13886328
- 4Feder HM Jr, Long SS. Herpetic whitlow. Epidemiology, clinical characteristics, diagnosis, and treatment. Am J Dis Child. 1983 Sep;137(9):861-3. doi: 10.1001/archpedi.1983.02140350035009. PMID: 6613951.
- 5Nardi NM, McDonald EJ, Syed HA, et al. Felon. [Updated 2024 Apr 30]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430933/
- 6Brkljac, M., Bitar, S., & Naqui, Z. (2014). A case report of herpetic whitlow with positive Kanavel’s cardinal signs: a diagnostic and treatment difficulty. Case Reports in Orthopedics, 2014.
- 7Schwandt NW, Mjos DP, Lubow RM. Acyclovir and the treatment of herpetic whitlow. Oral Surg Oral Med Oral Pathol. 1987 Aug;64(2):255-8. doi: 10.1016/0030-4220(87)90100-9. PMID: 2957639.
- 8Patel, Asha & Romanelli, Paolo & Roberts, Brenda & Kirsner, Robert. (2007). Treatment of Herpes Simplex Virus Infection. Advances in skin & wound care. 20. 408-12. 10.1097/01.ASW.0000280199.58260.62.

