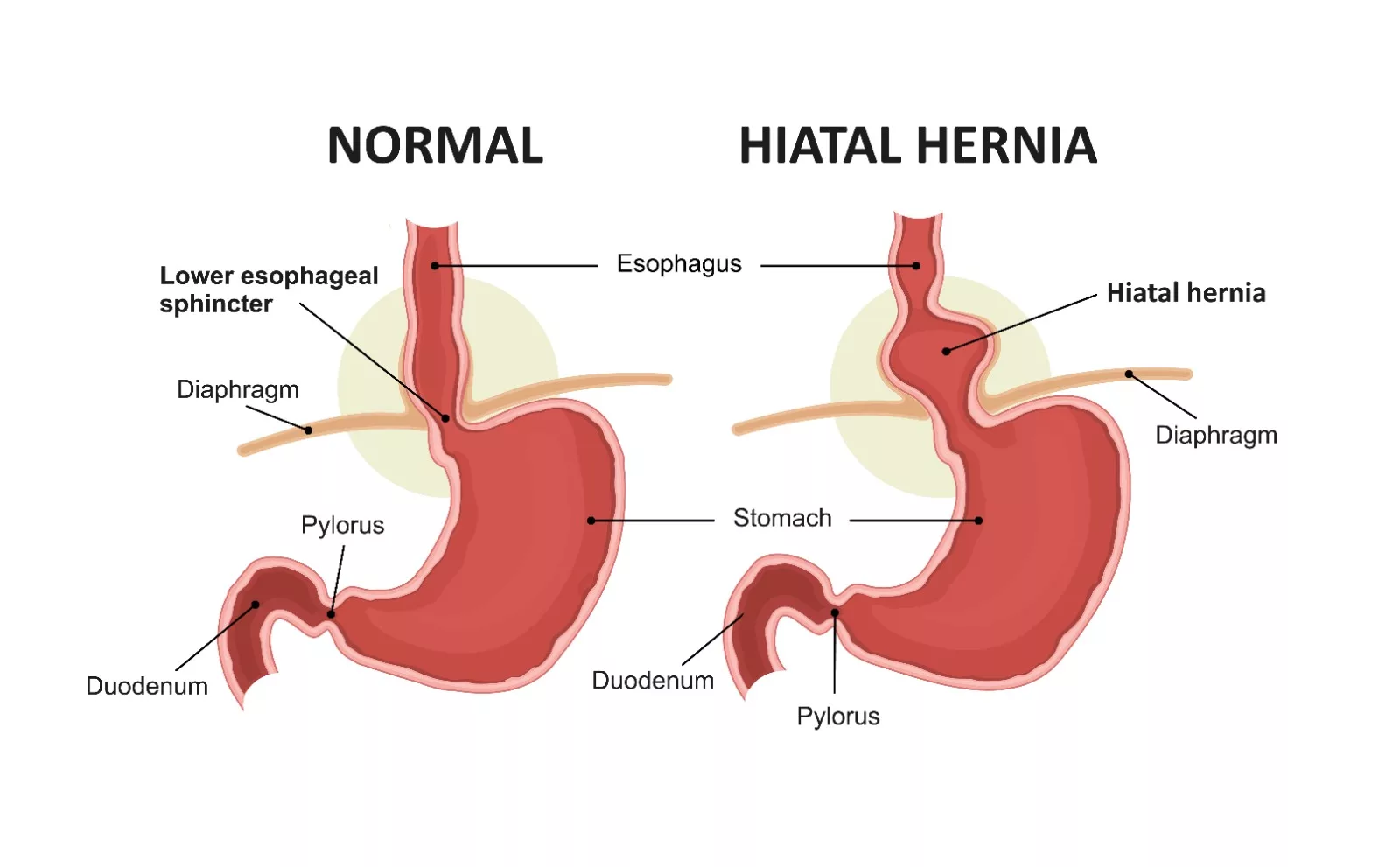
A hiatal hernia is a common condition in which the upper part of the stomach pushes up through the esophageal hiatus—a small opening in the diaphragm—and enters the chest cavity. The diaphragm is a dome-shaped muscle that separates the chest from the abdominal cavity and plays a key role in breathing. Normally, the esophagus (the food pipe) passes through this hiatus before connecting to the stomach. In a hiatal hernia, part of the stomach moves through this opening and into the thoracic cavity.
The development of a hiatal hernia is multifactorial, often linked to increased intra-abdominal pressure, aging, obesity, or trauma. While the condition is common, especially in older adults, it rarely leads to life-threatening complications.
The condition is more prevalent in adults than in children. The prevalence of hiatal hernia is also high in women. Around 55 to 60% of people above 50 years have a hiatal hernia, but only 9% of them have symptoms.1Smith, R.E., S. Sharma, and R.D. Shahjehan, Hiatal hernia, in StatPearls [Internet]. 2024, StatPearls Publishing. This condition is rare in rural regions of Africa but common in Western Europe and North America.2Richter, J.E. and J.H. Rubenstein, Presentation and epidemiology of gastroesophageal reflux disease. Gastroenterology, 2018. 154(2): p. 267-276.
Types of Hiatal Hernia
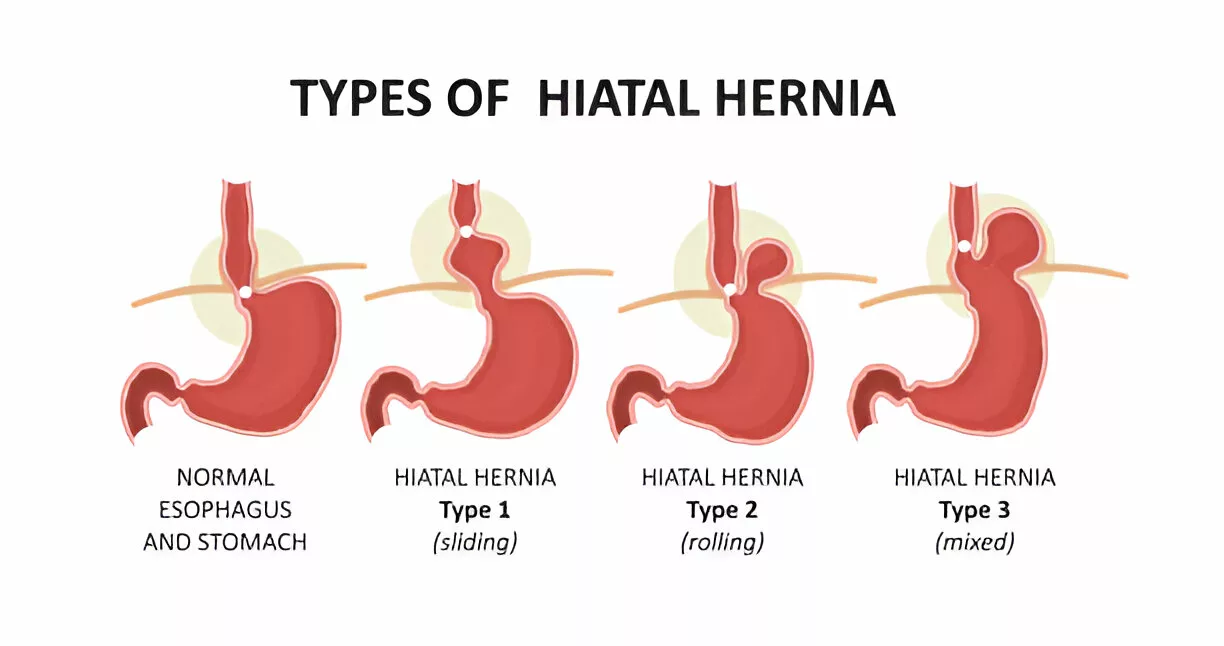
The classification of hiatal hernias helps guide both short-term management and long-term treatment strategies. Hiatal hernias are categorized into four types:
Type 1:
Type 1 is also named the sliding type. It presents more than 95% of hiatal hernias.3Smith, R.E., S. Sharma, and R.D. Shahjehan, Hiatal hernia, in StatPearls [Internet]. 2024, StatPearls Publishing. It occurs when the gastroesophageal junction (the region where the esophagus connects the stomach) migrates in the direction of the hiatus. This type is often associated with gastroesophageal reflux disease (GERD).
Type 2:
It is also called para-esophageal type. In this less common form, the gastroesophageal junction remains in place, but a part of the stomach herniates through the hiatus and sits alongside the esophagus in the chest (mediastinum). It carries a risk of gastric volvulus or strangulation and may require surgical intervention even in the absence of symptoms.
Type 3:
It is a mixture of sliding hernia with para-esophageal hernia. In this type, both the gastro-esophageal junction and a portion of the stomach migrate into the mediastinum.
Type 4:
In this form, the stomach, along with additional abdominal organs such as the colon, spleen, or small intestine, herniates into the thoracic cavity.4Alvarez, L.A., et al., Hiatal Hernia of Stomach and Lesser Omentum in a Cadaver: Is It a Type III or IV? Cureus, 2024. 16(3).
Causes & Risk Factors of Hiatal Hernia
Hiatal hernia can occur in two forms: it can be acquired or congenital. Additionally, the prevalence of this condition increases with age. The most common predisposing factor to the development of hiatal hernia is age-related loss of elasticity and flexibility due to muscle weakness.
Other identified predisposing factors include:
- Obesity
- Coughing
- Pregnancy
- Straining during heavy bowel movement
- Trauma
- Previous surgeries
- Chronic obstructive pulmonary disease (COPD)
- Elevated intra-abdominal pressure5Hyun, J.J. and Y.-T. Bak, Clinical significance of hiatal hernia. Gut and liver, 2011. 5(3): p. 267.
Symptoms of Hiatal Hernia
Small forms of hiatal hernias are usually asymptomatic. In those who are symptomatic, the most common presentation is gastroesophageal reflux disease (GERD). The related symptoms that hiatal hernia patients present are:
Patients often experience these symptoms:
- Heartburn
- Regurgitation
- Dysphagia (difficulty in swallowing)
- Acid reflux (it is the backflow of stomach acid towards the esophagus)
- Abdominal or chest pain
- Indigestion or feeling full shortly after eating
- Sore throat or hoarseness
Heartburn is the most typical clinical manifestation, but some individuals also present some extra-esophageal signs. Extra-esophageal symptoms can be chronic coughs, asthma, chronic laryngitis, dental erosions, dyspnea, pulmonary fibrosis and atrial fibrillation.
Diagnosis of Hiatal Hernia
The physical consideration in hiatal hernia and GERD patients hardly helps to approve the diagnosis. Here is a detailed overview of the diagnostic methods of hiatal hernia:
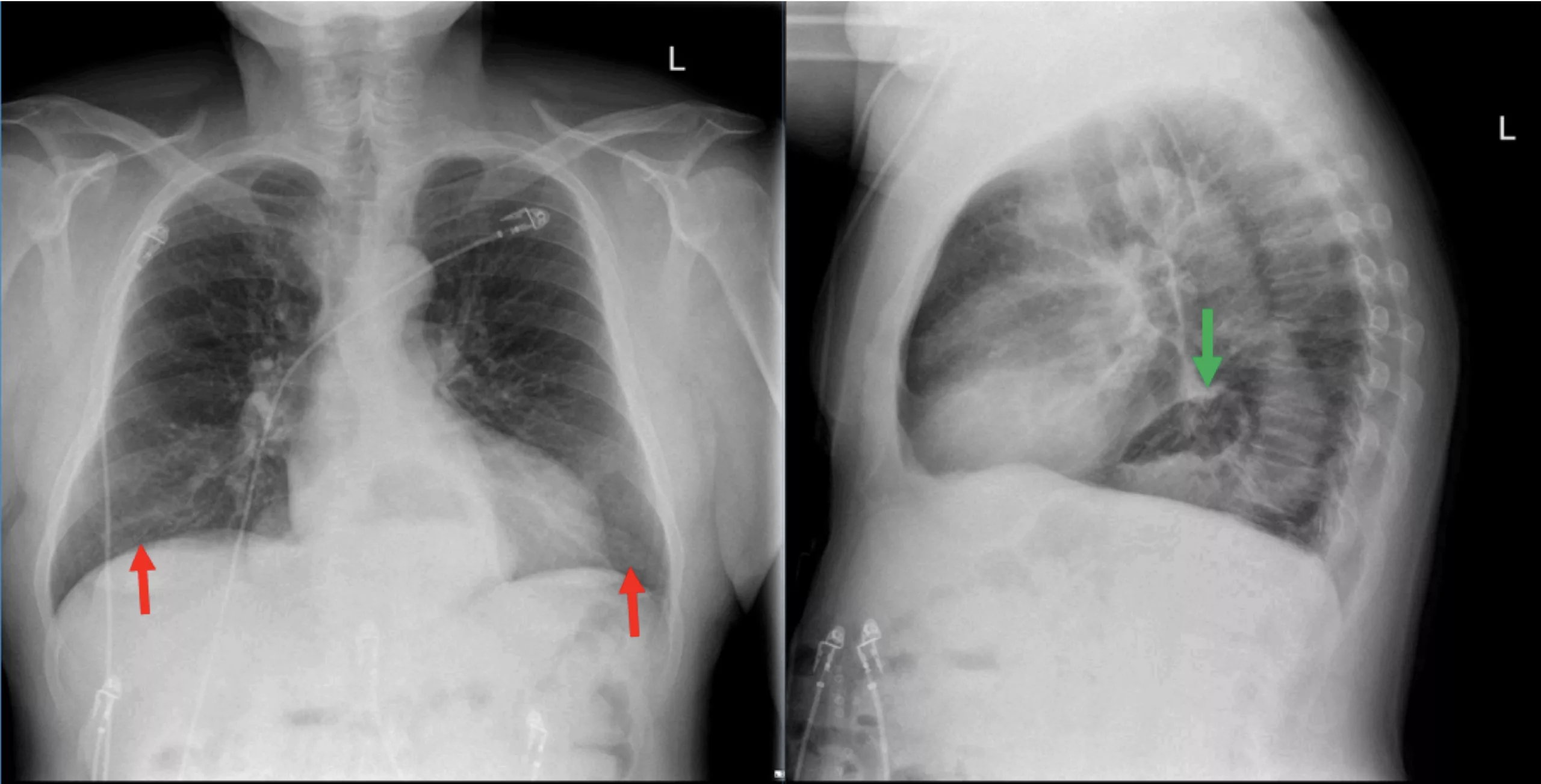
Chest X-Ray (with or without barium):
Standard chest X-rays may incidentally detect a hiatal hernia, particularly if a large portion of the stomach has migrated into the chest. A barium-enhanced X-ray improves visualization of the stomach and esophagus, helping to assess the size and position of the herniated portion.
Esophagram (Barium Swallow Study):
This dynamic imaging test uses real-time X-rays (fluoroscopy) to assess the swallowing mechanism and visualize herniation. After swallowing barium contrast, the distention of the esophagus and the presence of an air-fluid level in the herniated portion may confirm the diagnosis.
Endoscopy:
Endoscopy, or more precisely, gastrointestinal endoscopy, is a primary diagnostic tool for hiatal hernia. It is a process that examines the digestive system using a long and thin tube. The tube is equipped with a tiny camera known as an endoscope. It is passed down your throat while you are sedated and helps visualize the inside of your esophagus, stomach, and duodenum to check for swelling, projecting live images on the screen. A bulging part of the stomach through diaphragm into the chest cavity upon endoscopy confirms the diagnosis of a hiatal hernia.
Barium Swallow or Upper Gastrointestinal Series:
This test is often grouped with esophagram. It involves drinking a barium solution to coat the lining of the upper GI tract, providing clear images of the esophagus, stomach, and duodenum. It’s useful for detecting structural abnormalities and reflux.
Esophageal Manometry:
This test examines if you have any problems with swallowing or reflux. A small tube is inserted into your nostril and then down your throat into the esophagus to measure the pressure that your esophagus muscles make at rest and during swallowing. In hiatal hernia, it may show lower esophageal sphincter (LES) function or a displaced gastroesophageal junction.
pH Monitoring:
The 24-hour pH test is considered the gold standard for detecting acid reflux. A small pH probe is placed in the lower esophagus (typically 5 cm above the LES) for 24 hours. A DeMeester score of 14.7 or higher is considered diagnostic for GERD, which often coexists with hiatal hernia.6Mainie, I., et al., Acid and non-acid reflux in patients with persistent symptoms despite acid suppressive therapy: a multicentre study using combined ambulatory impedance-pH monitoring. Gut, 2006. 55(10): p. 1398-1402.
Computed Tomography:
A CT scan is not usually recommended, but it can help provide additional information. Typically, a hiatal hernia is discovered incidentally during a CT scan performed for another condition.7Roman, S. and P.J. Kahrilas, The diagnosis and management of hiatus hernia. bmj, 2014. 349.
Management & Treatment of Hiatal Hernia
The treatment and management of this condition depend on the type and severity of its symptoms. Medical care may be necessary if the hernia becomes incarcerated or strangulated, as this can compromise blood flow to the stomach and constitute a surgical emergency. Additionally, severe GERD can lead to inflammation, redness, and swelling of the esophagus, known as esophagitis, which may also necessitate medical intervention. The healthcare providers can recommend the following medications:
- Antacids can provide quick relief by weakening or neutralizing stomach acid. However, excessive use of antacids can result in some side effects, such as kidney abnormalities or diarrhoea. They only provide temporary relief; hence, they are not recommended for long-term management.8Sfara, A. and D.L. Dumitrascu, The management of hiatal hernia: an update on diagnosis and treatment]. Medicine and pharmacy reports, 2019. 92(4): p. 321.
- H-2- receptor blockers such as cimetidine, famotidine, and nizatidine can reduce the production of acid.
- Proton pump inhibitors are more potent acid blockers than H-2-receptor blockers. They allow time for the esophageal tissue to heal. These include omeprazole and lansoprazole.
Surgery:
Surgery is typically recommended for symptomatic para-esophageal hernias, complications like obstruction or strangulation, or when medical therapy fails to control GERD symptoms.
The hiatal hernia surgery repairs the condition by drawing your stomach and lower esophagus back under the diaphragm. It closes the hole in the diaphragm where the hernia comes through and tightens the junction between your esophagus and stomach. The most common procedure is Nissen fundoplication, in which the fundus (upper part of the stomach) is wrapped around the lower esophagus to reinforce the LES and prevent reflux. The name is attributed to the upper part of the stomach (fundus). During the surgery, the surgeon wraps the fundus around the lower esophagus and attaches it with stitches or surgical staples.
A partial fundoplication is the process of choice when the motility is poor. Common partial fundoplication is the Toupet procedure, which involves a posterior wrap (270° wrap), and the Dor procedure, which involves an anterior wrap (180–200° wrap). Surgeons believe that when esophageal obstruction is concerned, a partial wrap can also help to prevent the esophageal obstruction.
Surgical approaches include:
- Thoracotomy: An open surgery through the chest wall (rare).
- Laparoscopic repair: Minimally invasive, with small incisions and a camera-guided approach.
Both approaches aim to:
- Reinforce the esophagogastric junction to prevent recurrence.9DeMeester, S.R., Laparoscopic hernia repair and fundoplication for gastroesophageal reflux disease. Gastrointestinal Endoscopy Clinics, 2020. 30(2): p. 309-324.
- Pull the stomach back into the abdomen
- Close the widened hiatus
Self-Care Hiatal Hernia Management
Specific lifestyle changes can also help lessen the severity and frequency of the reflux and manage this condition. These include:
- Quit smoking as it affects your lower esophageal sphincter muscles, making them weaker. Smoking can also cause chronic coughing (it can stress the muscles around your hiatal hernia).
- Avoid lying down immediately after eating.
- Avoid rich, fatty meals that can trigger more enzymes and stomach acid to help digest them.
- Smaller meals can reduce the pressure on your stomach.
- Losing weight can also help.
- Avoid lifting heavy weights.
- Practice good posture while sleeping.
- Patients receiving treatment for hiatal hernia and GERD symptoms should strictly follow their medicines.
Prognosis of Hiatal Hernia
Patients usually recover within two to three days in the hospital, depending upon the type of surgery they had. The success of the surgery can be assessed by evaluating symptom relief and improvement in acid exposure of the esophagus, the occurrence of complications, and the need for reoperation. You will continue to recover at home for two to six weeks while your surgery is healing. Your provider can prescribe a modified diet that begins with liquids, gradually progresses to soft foods, and ultimately transitions to solid foods. Additionally, weight loss is a common occurrence after a hiatal hernia.
Complications
Patients older than 72 years with high frailty can have a higher risk of morbidity after para-esophageal hernia repair.10Wang, T.N., et al., The effect of frailty and age on outcomes in elective para-esophageal hernia repair. Surgical Endoscopy, 2023. 37(12): p. 9514-9522. It means age and frailty are important predictors of morbidity after hernia repair. Complications after surgery can be typically minor in some cases. Complications specific to anti-reflux surgery are:
- Dysphagia
- Hepatosplenic injuries
- Gastro-esophageal injuries
- Pneumothorax11Smith, R.E., S. Sharma, and R.D. Shahjehan, Hiatal hernia, in StatPearls [Internet]. 2024, StatPearls Publishing.
A Quick Review
Hiatal hernia is a common condition. Your doctor may diagnose it accidentally while working up for another reason. In many cases, medication and lifestyle changes are sufficient to manage the condition. However, in more severe cases, the patient may require surgery to repair the hernia. Surgery is usually the most effective in most cases; however, in aged patients, it can cause some complications.
Refrences
- 1Smith, R.E., S. Sharma, and R.D. Shahjehan, Hiatal hernia, in StatPearls [Internet]. 2024, StatPearls Publishing.
- 2Richter, J.E. and J.H. Rubenstein, Presentation and epidemiology of gastroesophageal reflux disease. Gastroenterology, 2018. 154(2): p. 267-276.
- 3Smith, R.E., S. Sharma, and R.D. Shahjehan, Hiatal hernia, in StatPearls [Internet]. 2024, StatPearls Publishing.
- 4Alvarez, L.A., et al., Hiatal Hernia of Stomach and Lesser Omentum in a Cadaver: Is It a Type III or IV? Cureus, 2024. 16(3).
- 5Hyun, J.J. and Y.-T. Bak, Clinical significance of hiatal hernia. Gut and liver, 2011. 5(3): p. 267.
- 6Mainie, I., et al., Acid and non-acid reflux in patients with persistent symptoms despite acid suppressive therapy: a multicentre study using combined ambulatory impedance-pH monitoring. Gut, 2006. 55(10): p. 1398-1402.
- 7Roman, S. and P.J. Kahrilas, The diagnosis and management of hiatus hernia. bmj, 2014. 349.
- 8Sfara, A. and D.L. Dumitrascu, The management of hiatal hernia: an update on diagnosis and treatment]. Medicine and pharmacy reports, 2019. 92(4): p. 321.
- 9DeMeester, S.R., Laparoscopic hernia repair and fundoplication for gastroesophageal reflux disease. Gastrointestinal Endoscopy Clinics, 2020. 30(2): p. 309-324.
- 10Wang, T.N., et al., The effect of frailty and age on outcomes in elective para-esophageal hernia repair. Surgical Endoscopy, 2023. 37(12): p. 9514-9522.
- 11Smith, R.E., S. Sharma, and R.D. Shahjehan, Hiatal hernia, in StatPearls [Internet]. 2024, StatPearls Publishing.

