What is Hookworm Infection?
Hookworm infection is a parasitic disease caused by roundworms that belong to the Ancylostoma and Necator genera. These worms are soil-transmitted helminths that infect humans primarily through contact with contaminated soil. The infection occurs when hookworm larvae penetrate the skin, usually through bare feet, and migrate through the bloodstream to the lungs and then to the small intestine, where they mature into adult worms. These worms can live for several years, feeding on the host’s blood and often causing iron deficiency anemia (IDA) due to chronic blood loss. Excessive blood loss is the most common clinical manifestation of hookworm infection.
The primary human-infecting species are:
- Ancylostoma duodenale
- Necator americanus
Additionally, Ancylostoma ceylanicum can infect humans, cats, and dogs.1ukas A, Hotez PJ, Diemert D, Yazdanbakhsh M, McCarthy JS, Correa-Oliveira R, et al. Hookworm infection. Nature reviews Disease primers. 2016;2(1):1-18.
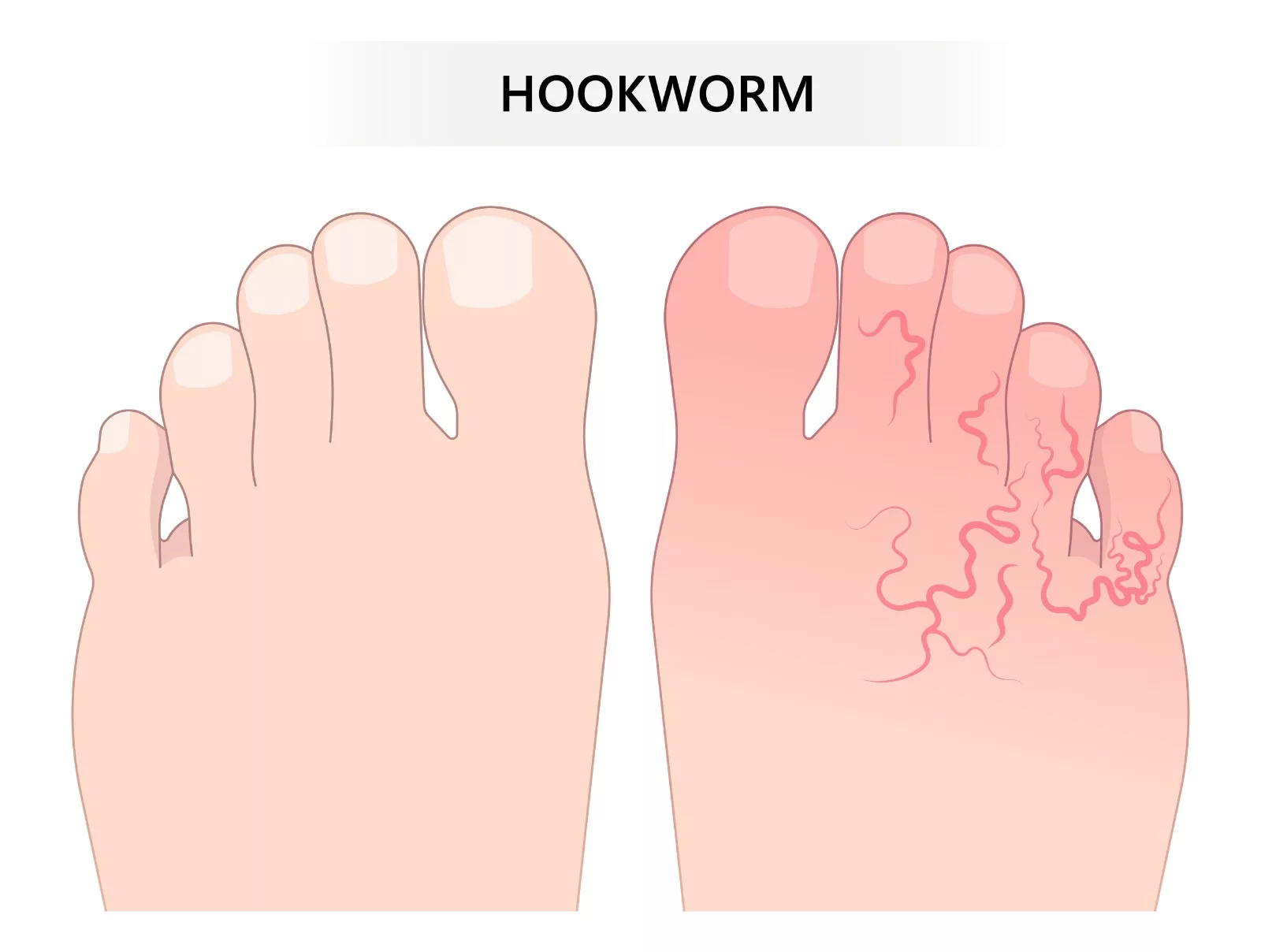
Sometimes, larvae from hookworms that usually infect animals, such as dogs or cats, can enter human skin but cannot fully develop into adult worms. Instead, they migrate just under the skin, causing an itchy, red rash known as cutaneous larva migrans (CLM). This rash often has winding tracks where the larvae have moved, but it does not lead to further health complications.
Who is at Risk for Hookworm Infection?
The high-risk populations for this infection are children and women of childbearing age. It is common in tropical and subtropical areas.2Chapman PR, Giacomin P, Loukas A, McCarthy JS. Experimental human hookworm infection: a narrative historical review. PLoS Neglected Tropical Diseases. 2021;15(12):e0009908.
According to estimates, approximately 450 million people globally suffer from chronic hookworm infection, leading to about 2.1 million disability-adjusted life years (DALYs) lost annually. The infection also imposes a substantial economic burden, resulting in over $100 billion in global economic losses.3Bartsch SM, Hotez PJ, Asti L, Zapf KM, Bottazzi ME, Diemert DJ, et al. The global economic and health burden of human hookworm infection. PLoS neglected tropical diseases. 2016;10(9):e0004922. Many people do not experience symptoms, but basic signs of hookworm infection include diarrhea and fever. Healthcare providers prescribe medications to treat the infection.
Structure of Hookworm
Adult hookworms have a stout, cylindrical body covered by a tough cuticle. Females are larger (10-13 mm) than males (8-11 mm). The anterior end is curved and contains a buccal capsule, which aids in attachment to the host’s intestinal lining. For Ancylostoma duodenale, this capsule contains six sharp teeth, while Necator americanus has cutting plates instead of teeth. Hookworms possess five esophageal glands that play roles in digestion and blood feeding. Sexes are separate and can be distinguished by various features. The most common one is size; males are smaller than females. Females possess a pointed posterior end, while males carry a copulatory bursa at their posterior ends.4Chonkar S. Structure of Adult Hookworm.
Hookworm eggs are oval and have a thin shell, while the larvae undergo two developmental stages: rhabditiform (early, rod-shaped stage) and filariform (slender, infective stage). The larvae possess paired sensory structures (sensilla) near the mouth, which allow them to detect environmental cues and locate hosts.5Fetouh N. Ancylostoma duodenale [Available from: https://animaldiversity.org/accounts/Ancylostoma_duodenale/#60f241a5fe974ccfac41c681a23fbfae.

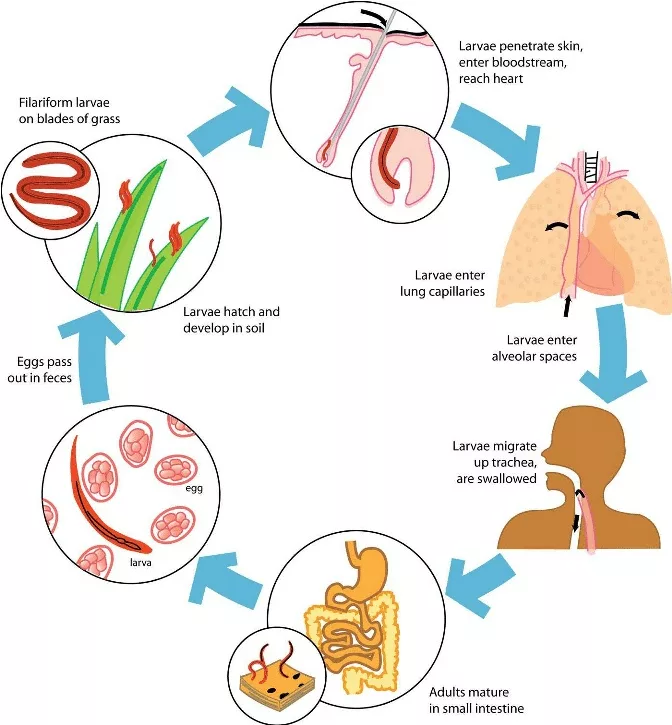
Life Cycle of Hookworm
The life cycle of hookworm involves seven steps. These steps are as follows;
Egg Stage
Hookworm eggs are excreted in the feces of infected hosts. These eggs require warm, moist, and shaded soil to develop. In optimal conditions, the eggs hatch within 1-2 days, releasing larvae.
Rhabditiform Larvae
The hatched larvae, known as rhabditiform larvae, are non-infective and feed on organic material in the soil. During this stage, they undergo two molts as they prepare to transition to the infective stage.
Filariform Larvae
After two molts, the rhabditiform larvae develop into infective juveniles or filariform larvae. The infective larvae can survive in the moist soil for weeks. They are sensitive to desiccation and direct sunlight. An arrest in development characterizes this stage until a new host is reached.
Infection
When a human comes into contact with soil containing infective filariform larvae, the larvae penetrate the skin using proteolytic enzymes and mechanical action. Entry points are often the feet or other exposed areas. Once inside, the larvae enter the bloodstream or lymphatic system and travel to the heart and lungs.
Pulmonary Migration
When they reach the lungs, the juveniles leave the circulatory system. There, in the lungs, the larvae penetrate the alveoli. From there, they move upward through the bronchial tree to the pharynx, where these larvae are swallowed.
Migration & Maturation in the Small Intestine
After being swallowed, the larvae travel to the small intestine. They attach to the intestinal wall using their buccal capsule and begin feeding on blood. Within 3-5 weeks, the larvae mature into adult worms.
Reproduction
Adult hookworms reside in the small intestine, where they attach to the mucosa. Males may detach to seek mates. Female hookworms may lay 10,000 to 30,000 eggs per day during their average lifespan of one year. The cycle continues when the hosts excrete the eggs with feces.6Loukas A, Hotez PJ, Diemert D, Yazdanbakhsh M, McCarthy JS, Correa-Oliveira R, et al. Hookworm infection. Nature reviews Disease primers. 2016;2(1):1-18.
Causes & Transmission of Hookworm Infection
Skin penetration is the most common route of transmission. People can get the infection while walking barefoot on soil contaminated with hookworm eggs. Poor sanitation practices, including outdoor defecation or unimproved sanitation facilities, can contaminate soil. Hookworms can survive in moist and warm climates, so living in tropical and subtropical regions can make you vulnerable to infection. Hookworm infection can also occur by ingesting hookworm larvae in contaminated water or food.
Pathophysiology of Hookworm Infection
When infective larvae enter the human host through percutaneous invasion, it results in a local pruritic, erythematous rash. This rash is also known as ground itch. It typically appears on the hands and feet.
Blood Loss
Multiple factors induce blood loss in the host. Substantial blood loss occurs when adult worms feed directly on the host’s blood. The host’s erythrocytes are digested in the gastrointestinal tract of the hookworm through proteolytic enzymes. Most of the blood loss also occurs as a result of leakage around the attachment site of the hookworm in the gut of the host. Each adult hookworm ingests about 0.03–0.05 mL of blood daily, depending on the species. For example, Ancylostoma duodenale causes more blood loss than Necator americanus. Chronic or heavy infections may result in hypoproteinemia, anasarca (generalized edema), and abdominal distension. A yellowish discoloration of the skin, referred to as chlorosis, is often seen in severe cases.7Loukas A, Hotez PJ, Diemert D, Yazdanbakhsh M, McCarthy JS, Correa-Oliveira R, et al. Hookworm infection. Nature reviews Disease primers. 2016;2(1):1-18.
Iron-Deficiency Anemia (IDA)
Hookworm infections lead to chronic blood loss, resulting in IDA when the host’s iron intake and reserves are insufficient to compensate for the losses. The degree of IDA largely depends on the species of the infecting hookworm. Necator americanus causes less blood loss than Ancylostoma duodenale. Moderate to heavy hookworm infections result in considerable protein losses, leading to hypoproteinaemia. The clinical picture of the infection resembles kwashiorkor in most severe cases. The combination of protein losses, anemia, and chlorosis presents hookworm infection as a yellow-puffy disease.8Loukas A, Hotez PJ, Diemert D, Yazdanbakhsh M, McCarthy JS, Correa-Oliveira R, et al. Hookworm infection. Nature reviews Disease primers. 2016;2(1):1-18.
Signs, Symptoms & Complications of Hookworm Infection
Hookworm infection leads to a variety of symptoms. These symptoms depend on the number of hookworms present in the body, the disease’s severity, and the individual’s overall health.
Skin Reaction
The most common and initial symptom includes an itchy and red rash. This rash occurs at the larval entry site, also called ground itch.

Cutaneous Larva Migrans (CLM):
Infections caused by zoonotic hookworm species (Ancylostoma braziliense and A. caninum) can lead to this condition. It is characterized by serpiginous, erythematous tracks on the skin, severe itching, and localized inflammation. These tracks represent the migration of larvae in the epidermis and are a hallmark of zoonotic hookworm infections.
Anemia Related Symptoms
IDA leads to:
- Weakness
- Extreme fatigue
- Shortness of breath
- Heart palpitations
- Pale skin
- Dizziness
Respiratory Symptoms
When the infective larvae migrate to the lungs, they cause respiratory symptoms, including wheezing, chest pain, cough, and fever in some cases.
Gastrointestinal Symptoms
The gastrointestinal symptoms may include:
- Loss of appetite and subsequent weight loss due to nutrient malabsorption.
- Frequent loose stools due to intestinal irritation.
- Discomfort or abdominal pain.
Nutritional Deficiencies
Chronic infection leads to hypoproteinaemia and hypoalbuminemia, most commonly in children. These deficiencies can affect their cognitive and physical development.
Severe Complications
In case of severe infections, heart failure and widespread fluid retention can also occur.
Diagnosis of Hookworm Infection
Early and accurate diagnosis of the infection is essential for effectively managing the infection.
Clinical Consideration:
Healthcare providers often consider symptoms such as skin rashes, abdominal discomfort, and diarrhea, especially in individuals returning from or living in areas with poor sanitation and endemic hookworm prevalence. Cutaneous larva migrans caused by hookworm larvae migrating under the skin—may also serve as a diagnostic clue, particularly for zoonotic hookworm species.
Laboratory Tests:
If you have symptoms of hookworm infection, your healthcare provider will ask for laboratory tests. These tests include:
Microscopic & Molecular-Based Stool Examination
Stool examination under a microscope for identifying hookworm eggs is the standard method of diagnosing hookworm infection. The laboratory stores the stool sample in a dry, clean, leakproof container. The stool sample is then processed using five microscopic stool examination methods. These methods include direct wet mount microscopy, the kato-katz technique, formol ether concentration, McMaster, and test tube floatation. Examining stool samples within several hours of collection is crucial to prevent eggs from hatching into larvae.9Zeleke AJ, Addisu A, Derso A, Tegegne Y, Birhanie M, Sisay T, et al. Evaluation of hookworm diagnosis techniques from patients in Debre Elias and Sanja Districts of the Amhara Region, Ethiopia. Journal of parasitology research. 2021;2021(1):6682330.
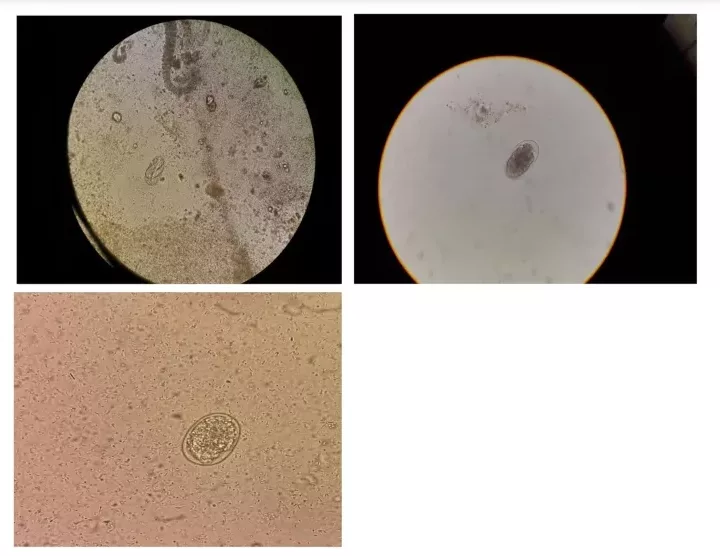
Molecular-based stool examination involves next-generation sequencing, polymerase chain reaction (PCR), and Loop-mediated isothermal amplification (LAMP). These techniques examine stool specimens that are fresh, fixed, or stolen. Confirmation comes with the detection of hookworm larvae in the stool sample. However, the majority of the clinical settings lack the availability of these approaches.10Loukas A, Hotez PJ, Diemert D, Yazdanbakhsh M, McCarthy JS, Correa-Oliveira R, et al. Hookworm infection. Nature reviews Disease primers. 2016;2(1):1-18.
Blood Test
Healthcare providers also conduct blood tests to check for anemia or protein deficiency, the most common complication of the infection. Also, an increase in eosinophils serves as an indicator of the parasitic disease.
Endoscopy:
Endoscopy can be a valuable diagnostic tool for hookworm infection, especially in cases where stool examination yields negative results. Endoscopy allows the direct visualization of hookworms. During endoscopy, hookworms can be visualized and attached to the intestinal mucosa.11Tiremo SN, Shibeshi MS. Endoscopic Diagnosis of Hookworm Disease in a Patient with Severe Iron Deficiency Anemia: A Case Report. International Medical Case Reports Journal. 2023:841-5.
Treatment & Management of Hookworm Infection
The treatment of hookworm infection primarily involves using anthelmintic medications to eliminate the parasites and manage other complications.
Anthelmintic Medications:
The most commonly used anthelmintic medications include albendazole and mebendazole.
Albendazole
Albendazole is commonly prescribed to treat hookworm infections. It works by inhibiting microtubule polymerization in the parasites, leading to the death of adult worms. The usual dosage is 400 mg orally once daily for three to seven days, though the length of treatment may vary based on the severity of the infection.
Mebendazole
Another effective treatment is mebendazole, which also targets the hookworms by disrupting their ability to absorb glucose. The standard dosage is 100 mg daily for three days.12Loukas A, Hotez PJ, Diemert D, Yazdanbakhsh M, McCarthy JS, Correa-Oliveira R, et al. Hookworm infection. Nature reviews Disease primers. 2016;2(1):1-18.
Nutritional Support:
Improving nutritional intake can help in mitigating the effects of the infection. Protein- and iron-rich supplements and foods can help reduce the impact of anemia and support recovery.
Iron Supplementation:
As subsequent blood loss causes IDA, healthcare providers often recommend iron supplements. Vitamin B12 and folic acid are also necessary for red blood cell production during recovery.
Cryotherapy:
In some cases, cryotherapy may be used to target larvae in the skin before they migrate further into the body. This treatment is more commonly used in cases where cutaneous larva migrans (CLM) are present.
Management of Severe Cases:
Healthcare providers offer additional doses of anthelmintic medicines in case of severe infection and complications. In rare cases, doctors consider surgical interventions where medications are insufficient to handle the diseases. Regular follow-up is essential to monitor recovery from the severe infection. Follow-up and monitoring by healthcare providers can eliminate the infection completely.
Alternative Treatment Approaches:
- Levamisole and pyrantel pamoate are alternative drugs for the treatment of hookworm infection. These drugs lead to muscle cell depolarization, spastic paralysis, and ultimately leading to expulsion of worms from the gastrointestinal tract of the patient.13Köhler P. The biochemical basis of anthelmintic action and resistance. International journal for parasitology. 2001;31(4):336-45.
- Tribendimidine is also an emerging treatment for hookworm infection. Research reports show it is highly active against the disease in human and animal studies.14Steinmann P, Zhou X-N, Du Z-W, Jiang J-Y, Xiao S-H, Wu Z-X, et al. Tribendimidine and albendazole for treating soil-transmitted helminths, Strongyloides stercoralis and Taenia spp.: open-label randomized trial. PLoS neglected tropical diseases. 2008;2(10):e322.
- Pore-forming crystal proteins (Cry), particularly Cry5B, can be used against intestinal nematodes.
- Combination therapies (using drugs with different mechanisms of action) can improve the treatment efficacy. However, the use of combination therapies for hookworm infection is limited.15Loukas A, Hotez PJ, Diemert D, Yazdanbakhsh M, McCarthy JS, Correa-Oliveira R, et al. Hookworm infection. Nature reviews Disease primers. 2016;2(1):1-18.
Prevention Strategies & Tips
The Water Sanitation and Hygiene (WASH) program is the most promising strategy for preventing diarrheal diseases. WASH interventions are diverse and include:
- Improvement in water condition (quantity, quality, and access)
- Sanitation (improved latrines and sewer maintenance)
- Hygiene
- Community engagement and awareness
- Periodic community-based health education activities
Some of the developing countries also offer preventive treatment for hookworm infection. This Treatment is known as preventive chemotherapy. Health authorities offer preventive chemotherapy to people who are at high risk of infection, such as children and pregnant women.
Prevention Tips:
- Always wear shoes while walking outdoors, especially where the soil is moist.
- Minimize direct contact between the skin and soil. Most importantly, in areas with poor sanitation.
- Use mats or carpets while sitting on the ground.
- Ensure cooking food properly to help avoid contamination.
- Wash your hands properly after using the restroom.
- Wash your hands properly before handling the food.
- Avoid eating unwashed vegetables and fruits to avoid ingestion of hookworm larvae.
- Avoid using night soil (human feces) as fertilizers, which can lead to soil contamination.
- Use sanitary latrines to prevent the spread of hookworm eggs instead of defecating outdoors or in areas where soil becomes contaminated.
- Regularly deworm pets. Conduct regular fecal testing to ensure that your pets are free from hookworms.
- If your children play in sandboxes, immediately cover them to avoid being used as litter boxes by your pets.
- Take extra precautions while traveling to areas where hookworms are endemic.
- Advocate for better sewage disposable systems.
- Advocate for clean water access in communities.
- Educate communities about the risks of hookworm infection.
- Support and participate in community-wide deworming programs.
Final Remarks
Hookworm infection is a significant health problem in many parts of the world. Poor sanitation practices and living in warm climates can increase the risk of infection among individuals. It can be asymptomatic in many individuals. The potential severe complication is IDA. An accurate and early diagnosis is essential for effective treatment and management of the disease. Anthelmintic medications can play a role in effectively treating the infection. Community health initiatives and preventive measures are essential in controlling and reducing the incidence of hookworm infection. With appropriate medical attention and public health efforts, a complete recovery from the infection is possible.
Refrences
- 1ukas A, Hotez PJ, Diemert D, Yazdanbakhsh M, McCarthy JS, Correa-Oliveira R, et al. Hookworm infection. Nature reviews Disease primers. 2016;2(1):1-18.
- 2Chapman PR, Giacomin P, Loukas A, McCarthy JS. Experimental human hookworm infection: a narrative historical review. PLoS Neglected Tropical Diseases. 2021;15(12):e0009908.
- 3Bartsch SM, Hotez PJ, Asti L, Zapf KM, Bottazzi ME, Diemert DJ, et al. The global economic and health burden of human hookworm infection. PLoS neglected tropical diseases. 2016;10(9):e0004922.
- 4Chonkar S. Structure of Adult Hookworm.
- 5Fetouh N. Ancylostoma duodenale [Available from: https://animaldiversity.org/accounts/Ancylostoma_duodenale/#60f241a5fe974ccfac41c681a23fbfae.
- 6Loukas A, Hotez PJ, Diemert D, Yazdanbakhsh M, McCarthy JS, Correa-Oliveira R, et al. Hookworm infection. Nature reviews Disease primers. 2016;2(1):1-18.
- 7Loukas A, Hotez PJ, Diemert D, Yazdanbakhsh M, McCarthy JS, Correa-Oliveira R, et al. Hookworm infection. Nature reviews Disease primers. 2016;2(1):1-18.
- 8Loukas A, Hotez PJ, Diemert D, Yazdanbakhsh M, McCarthy JS, Correa-Oliveira R, et al. Hookworm infection. Nature reviews Disease primers. 2016;2(1):1-18.
- 9Zeleke AJ, Addisu A, Derso A, Tegegne Y, Birhanie M, Sisay T, et al. Evaluation of hookworm diagnosis techniques from patients in Debre Elias and Sanja Districts of the Amhara Region, Ethiopia. Journal of parasitology research. 2021;2021(1):6682330.
- 10Loukas A, Hotez PJ, Diemert D, Yazdanbakhsh M, McCarthy JS, Correa-Oliveira R, et al. Hookworm infection. Nature reviews Disease primers. 2016;2(1):1-18.
- 11Tiremo SN, Shibeshi MS. Endoscopic Diagnosis of Hookworm Disease in a Patient with Severe Iron Deficiency Anemia: A Case Report. International Medical Case Reports Journal. 2023:841-5.
- 12Loukas A, Hotez PJ, Diemert D, Yazdanbakhsh M, McCarthy JS, Correa-Oliveira R, et al. Hookworm infection. Nature reviews Disease primers. 2016;2(1):1-18.
- 13Köhler P. The biochemical basis of anthelmintic action and resistance. International journal for parasitology. 2001;31(4):336-45.
- 14Steinmann P, Zhou X-N, Du Z-W, Jiang J-Y, Xiao S-H, Wu Z-X, et al. Tribendimidine and albendazole for treating soil-transmitted helminths, Strongyloides stercoralis and Taenia spp.: open-label randomized trial. PLoS neglected tropical diseases. 2008;2(10):e322.
- 15Loukas A, Hotez PJ, Diemert D, Yazdanbakhsh M, McCarthy JS, Correa-Oliveira R, et al. Hookworm infection. Nature reviews Disease primers. 2016;2(1):1-18.