What is Kwashiorkar?
Kwashiorkor is a type of malnutrition linked with severe protein deficiency. It causes fluid retention, leading to a visibly distended and protruded abdomen and bilateral extremity swelling. This condition usually impacts children in impoverished regions with food scarcity.
Infants (aged below 12 months) and children under five years often coincide with the weaning period, and they more commonly observe Kwashiorkor. Its predominance is largely associated with instances of starvation in poverty-stricken areas around the globe.1Benjamin, Onecia, and Sarah L. Lappin. “Kwashiorkor.” StatPearls [Internet]. StatPearls Publishing, 2021.
Among the multiple difficulties humankind is facing these days, malnutrition tops the list, and the results are horrific. Malnutrition alone surpasses the toll of tuberculosis, malaria, and cancer combined, making it a matter of paramount concern.
Moreover, malnutrition is an underlying condition that predisposes individuals to other diseases. By weakening the immune system, it creates an opportunity for pathogens to proliferate and attack the body.2Trowell, Hugh C. “Kwashiorkor.” Scientific American 191.6 (1954): 46-51.

Causes of Kwashiorkor:
Kwashiorkor has multifaceted causes, with protein deficiency being the most significant factor. Several contributing factors include:
Poverty & Food Scarcity
Firstly, Kwashiorkor is an extreme form of malnutrition and predominantly affects the population residing in developing countries where food scarcity and high poverty rates prevail. In contrast, kwashiorkor is rarely present in developed countries. The highest rate of this disease is witnessed in areas of Africa near the equatorial line, where the rate of poverty is notably high. Closely linked to the socio-economic condition of that area, kwashiorkor is influenced by drought and damage to the crop, which further leads to this disease.3Alvarez, Jose Luis, et al. “Putting child kwashiorkor on the map.” CMAM Forum Technical Brief. 2016.
Poor Sanitation
Secondly, Kwashiorkor is prevalent in landscapes with poor sanitation facilities and subpar hygiene practices. The population is more susceptible to gastrointestinal problems, which can impair the body’s ability to absorb nutrients, increasing the risk of malnutrition.
High Risk of Infection
Thirdly, the risk of infectious diseases is very high in those nations because of weak immune systems. In such an environment, children are the most vulnerable.
Wrong Choice of Food
Moreover, Kwashiorkor usually occurs when children are weaning from breastfeeding to a complementary diet. They are usually given food rich in carbohydrates but lacking the required quantity of proteins. Insufficient protein intake, along with limited access to diverse foods, worsens this condition. Due to food scarcity and food insecurity, individuals do not get enough protein intake.
Lack of Healthcare Facilities
Lastly, lack of access to proper healthcare facilities leads to cases of malnutrition. No timely medical intervention and the delay in the identification and treatment of malnutrition become a contributing factor toward severe cases of kwashiorkor.
Risk Factors:
Kwahiorkar has the following risk factors:
Age & Dietary Practices
Children under five years old transitioning from breastfeeding to complementary diets are most vulnerable. Those consuming carbohydrate-rich but protein-deficient foods face a higher risk.
Nutritional Deficiencies
Individuals lacking essential vitamins and minerals in their diet are at increased risk of Kwashiorkor. Dietary antioxidants and exposure to aflatoxins from contaminated food further contribute to susceptibility.
Parasitic Infections:
Parasitic infections such as malaria, measles, and HIV can exacerbate malnutrition, including Kwashiorkor, by compromising immune function and nutritional status.4Vonasek, Bryan J., et al. “Risk factors for mortality and management of children with complicated severe acute malnutrition at a tertiary referral hospital in Malawi.” Paediatrics and International Child Health 40.3 (2020): 148-157.
Symptoms of Kwashiorkor:
Here are some of the distinctive symptoms of this severe form of malnutrition. By understanding these signs, we gain valuable insights into the complex impacts this condition has on the body.
Edema
Fluid becomes trapped in body tissues, affecting any part, with peripheral pitting edema commonly observed in kwashiorkor, particularly in the ankles and feet.
Bloated Abdomen
A distended and swollen abdomen due to ascites is a characteristic feature of kwashiorkor. A lot of fluid is accumulated in the abdominal cavity. The intestinal or bowel loops are also dilated. Hepatomegaly, or an increase in the size of the liver, is also seen.
Hair Flag Sign
Hair becomes dry, brittle, and thin, which can be easily plucked. Additionally, they become sparse and start losing their pigment.
Dermatitis
It is often called “flaky paint” or “peeling paint” dermatosis. It has dark peeling skin with scales and red patches, usually in the armpits, groin, limbs, and ears. Under these patches are atrophic depigmented areas that resemble a healing burn wound.
Enlarged Liver
Hepatomegaly is another sign. The liver becomes significantly enlarged and can be palpated. It is due to the infiltration of fats, especially triglycerides.
Reduced Muscle Mass
In infants and children, loss of subcutaneous muscle mass is observed. It is evident by the folds of the skin. There is marked muscle atrophy.
Dehydration
There is a loss of body fluids. Dehydration in patients suffering from kwashiorkor is one of the main reasons for the high fatality rate.
Loss of Appetite
Anorexia may occur, which leads to less consumption of food.
Fatigue & Lethargy
Some early signs of this condition include fatigue, irritability, and lethargy. Additionally, some psychic changes and apathy (lack of interest and enthusiasm) can be present.
Reduced Growth
Children may not grow properly and remain stunted. Growth retardation is particularly seen in younger children, which affects their overall stature.
Moon Facies
Round faces with prominent cheeks are sometimes seen in kwashiorkor.
Complications of Kwashiorkor:
Beyond the initial symptoms, Kwahiorkar has some broader complications and symptoms. Here is a comprehensive understanding of its impact.
- Hypoglycemia: Low blood sugar levels result in energy depletion. There is a decrease in glucose production and an increase in clearance.
- Hypovolemia or Hypovolemic Shock: Albumin levels are greatly reduced, and the person becomes intravascularly depleted. Due to less blood volume, circulatory collapse occurs.
- Hypothermia: Body temperature can drop dangerously low because of a thin subcutaneous fat layer. It causes cold stress and metabolic slowdown.
- Electrolyte Imbalance: A prominent abnormality is the body’s disturbance of water and electrolytes. Disrupted protein metabolism manifests as edema.
- Organ Dysfunction: The function of the major vital organs of the human body is disrupted, like the heart and liver. A person can have hepatomegaly, fatty liver, and cardiomegaly.
- Compromised Immune System: The patient becomes more susceptible to diseases and infections as malnutrition can impair the immune system.
- Liver Cirrhosis: The liver can have chronic damage, and it slowly becomes dysfunctional. This ultimately leads to liver failure.
- Pancreatic Atrophy: The reduced size of the pancreas contributes to digestive complications and enzyme deficiency.
- Gastrointestinal Mucosa Atrophy: The shrinkage of the mucosal lining of the small intestine enhances the chances of bacterial growth.
- Starvation and Death: Mortality rates are high. Prolonged malnutrition and starvation ultimately lead to death.

Diagnosis:
Healthcare providers typically recommend a series of laboratory studies to diagnose protein-energy malnutrition. These include:
- Complete Blood Cell (CBC) count
- Electrolyte level measurements (potassium, calcium, phosphate, magnesium)
- Blood urea nitrogen assessment
- Examination of serum albumin and prealbumin (transthyretin) levels
- Evaluation of micronutrient levels: Zinc, iron, vitamin D
Key Laboratory Findings in Kwashiorkor
When diagnosing kwashiorkor, healthcare providers focus on specific laboratory findings to better understand the condition:
- Hypoalbuminemia and hypoproteinemia affect essential amino acids, transferrin, and lipoprotein levels.
- Elevated plasma cortisol and growth hormone levels indicate hypoglycemia. Laboratory tests may reveal decreased insulin secretions and insulin-like growth factor levels.
- Both kwashiorkor and marasmus may exhibit metabolic acidosis and iron deficiency anemia.
- Electrolyte depletion, particularly potassium and magnesium.
- Presence of ketonuria: Protein deficiency may lower urea levels in urinary excretion, leading to ketonuria.5Hadi Atassi, Thomas L Abell, Romesh Khardori. “Protein-Energy Malnutrition Workup.” Medscape. Publishing 2019
Treating Kwashiorkor:
Treatment may vary from individual to individual. The World Health Organization (WHO) provides guidelines for treating malnutrition, especially kwashiorkor.
Treat Hypoglycemia
Healthcare providers gradually administer a rehydrating solution with glucose to manage hypoglycemia during the initial stages of treatment.
Correcting Hypothermia
External warmth is provided using blankets and heaters to help malnourished individuals maintain body temperature.
Managing Dehydration
To manage dehydration, doctors usually administer the RESOMAL (REhydration SOlution for MALnutrition) formula orally or through a tube to correct dehydration and maintain body electrolytes, especially fluid and sodium balance, in the Kwashiorkor patient.
Managing Electrolyte Imbalance
Healthcare workers prioritize maintaining electrolyte imbalance. It can be life-threatening, especially in the initial hours of refeeding.
Treating & Preventing Infections
As kwashiorkor patients have weak immunity, they contract many infectious diseases. Therefore, treating any existing infections with antibiotics is a priority. Furthermore, healthcare providers should protect patients from additional exposure to diseases and illnesses.
Administer Micronutrient Deficiencies
Correction of severe vitamin and mineral deficiencies is necessary before commencing refeeding therapy to mitigate potential serious side effects.
Cautious Feeding
The doctors gradually commence the diet in these patients so they do not develop refeeding syndrome, a potentially fatal condition caused by rapid refeeding after a prolonged period of undernutrition. To accommodate metabolic changes, they reintroduce food slowly and specifically focus on protein intake.
Encourage Catch-up Growth After Stability
Once the healthcare team achieves nutritional stability, they should strategically increase caloric intake to about 140% of the recommended value, utilizing WHO-provided ready-made liquid formulas.
Sensory Stimulation & Emotional Support
Children with kwashiorkor develop apathy. They become irritable, fatigued, and lethargic over time; therefore, solving mental issues should be a priority so they can bounce back. It is important to reboot their emotional, intellectual, and social skills. The child’s mother can play a crucial role in recovery.
Post-Recovery Follow-up
Before discharging the patient from the hospital, the medical staff should provide parents or guardians with a comprehensive follow-up plan. It should cover everything about the child’s nutritional needs and emotional needs. Medical staff should educate them about breastfeeding, hygiene, sanitation, and disease prevention. Before discharge from the hospital, the medical staff should ensure access to food supplies.6Training course on the inpatient management of severe acute malnutrition: facilitator’s guide.” (2021)
Prevention:
The Global Action Plan on Child Waste by WHO outlines ways to prevent kwashiorkor. Here are some recommendations.7Collins, Steve. “Reflections on the United Nations Draft Global Action Plan on wasting.” Field Exchange 62 (2020): 21. GLOBAL ACTION PLAN ON CHILD WASTING. A framework for action to accelerate progress in preventing and managing child wasting and the achievement of the Sustainable Development Goals
Educational & Social Protection
Some nations in the world lack proper knowledge about breastfeeding and the general feeding requirements of mothers and children in the early years. To address this issue, it is important to provide them with adequate and correct knowledge about nutrition to prevent malnutrition and kwashiorkor.
Nutritional Support
WHO has been actively working to provide nutrient-rich food to developing countries. Furthermore, as part of their efforts, they have introduced crops rich in protein and micronutrients such as vitamins and minerals in the affected areas. They have even produced nutrient-rich food using locally available resources, such as peanuts and skimmed milk, and introduced them to the patients.
Disease Control
Diseases and illnesses play an important role in building a community. In this regard, diseases such as chronic diarrhea cause a significant loss of calories and increase nutritional requirements. This vicious cycle depletes community resources and increases poverty. Therefore, stakeholders should pay special attention to sanitation and hygiene and conduct countrywide immunization programs. 8Collins, Steve. “Reflections on the United Nations Draft Global Action Plan on wasting.” Field Exchange 62 (2020): 21. GLOBAL ACTION PLAN ON CHILD WASTING. A framework for action to accelerate progress in preventing and managing child wasting and the achievement of the Sustainable Development Goals
Kwashiorkor and Marasmus
Severe acute malnutrition causes both kwashiorkor and marasmus, and they show clinical symptoms but are different in some aspects.
| Kwashiorkor | Marasmus | |
| Cause | Protein-deficient malnutrition. | Deficiency of Carbohydrates, proteins, and fats. |
| Depletion of micronutrients | Deficiency of antioxidants, minerals, and vitamins is more. | Less deficiency of micronutrients. |
| Appearance | Presents with swelling on ankles and feet and a protuberant belly. | Severe wasting and has a skeletal appearance. |
| Subcutaneous fat | Patients usually maintain their subcutaneous fat. | Loss of subcutaneous fat. |
| Weight loss | There may be some or no weight loss. | Weight loss is significant. |
| Fatty Liver | Fatty liver is the main characteristic. | No such observation. |
| Nutritional requirements | Protein is the key nutrient required. | Patients need proteins, carbohydrates, and fats. |
| Prevalence | In rural, poverty-stricken areas. | In rural, poverty-stricken areas. |
| Fatality and death | Fatal if left untreated. | Higher rate of fatality. |
| Administering antibiotics | Antibiotics improve the condition. | No effect. 9Alou, Maryam Tidjani, et al. “Difference between kwashiorkor and marasmus: Comparative meta-analysis of pathogenic characteristics and implications for treatment.” Microbial Pathogenesis 150 (2021): 104702. |
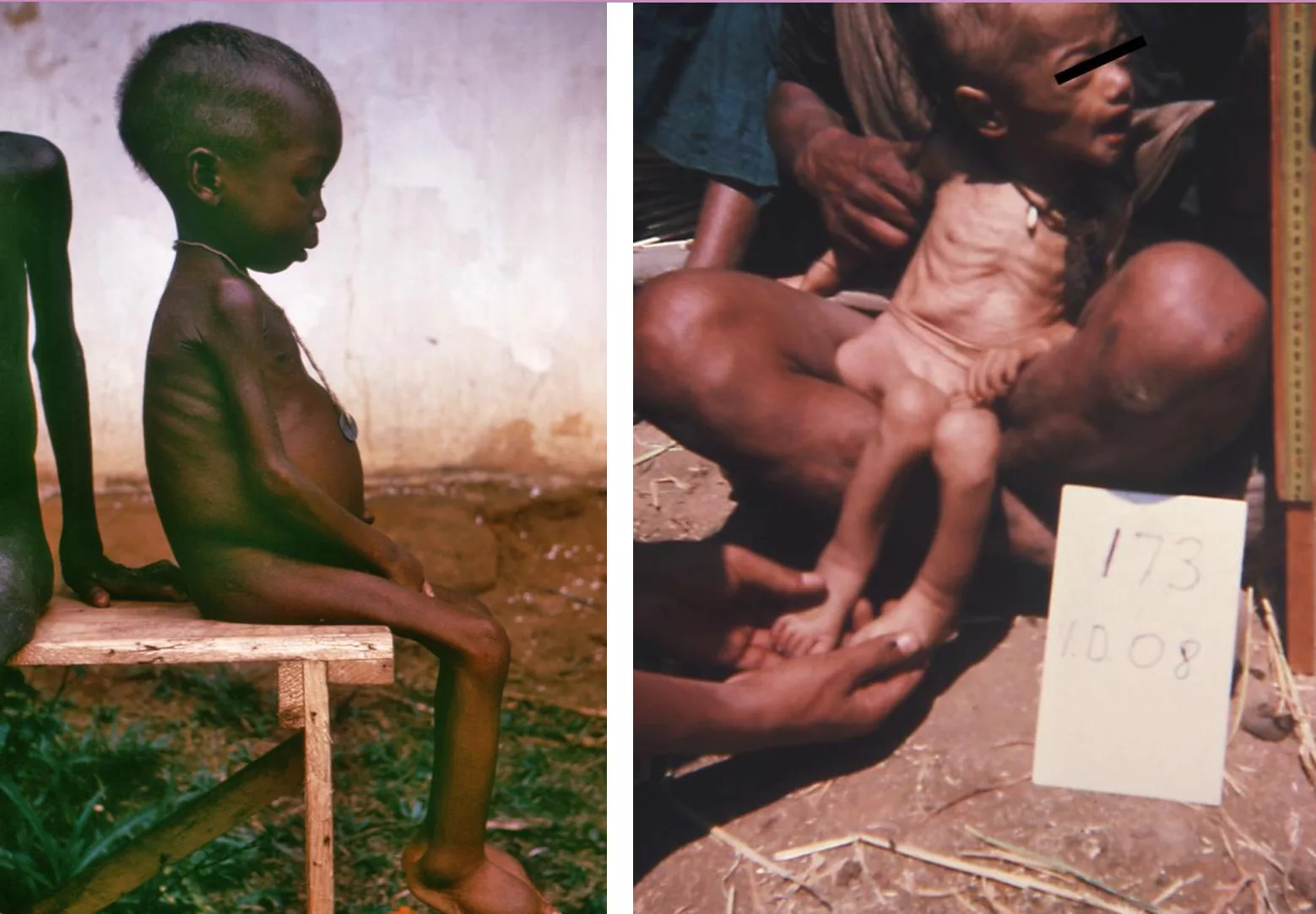
Right: Nepalese child exhibiting signs of extreme malnutrition, known as marasmus, in 1975.
Mortality & Morbidity Patterns in kwashiorkor
A study conducted in Zambia from 2009 to 2013 shed light on the high fatality rate associated with kwashiorkor. Kwashiorkor was the major malnutrition-deficient disease in the case study, with almost 62% of people suffering from it. Diarrhea and pneumonia were the main co-morbidities associated with kwashiorkor. Additionally, children infected with HIV had an 80% higher risk of mortality than children not infected with HIV.10Munthali, Tendai, et al. “Mortality and morbidity patterns in under-five children with severe acute malnutrition (SAM) in Zambia: a five-year retrospective review of hospital-based records (2009–2013).” Archives of Public Health 73.1 (2015): 1-9.
Conclusion
Kwashiorkor is a major challenge in developing countries where poverty is high. However, efforts in nutritional education, providing different food forms, and implementing other preventive measures can reduce the risk. Early diagnosis and timely intervention can prove to be effective. All healthcare providers can work towards alleviating the burden of Kwashiorkor across the globe, particularly in children.
Refrences
- 1Benjamin, Onecia, and Sarah L. Lappin. “Kwashiorkor.” StatPearls [Internet]. StatPearls Publishing, 2021.
- 2Trowell, Hugh C. “Kwashiorkor.” Scientific American 191.6 (1954): 46-51.
- 3Alvarez, Jose Luis, et al. “Putting child kwashiorkor on the map.” CMAM Forum Technical Brief. 2016.
- 4Vonasek, Bryan J., et al. “Risk factors for mortality and management of children with complicated severe acute malnutrition at a tertiary referral hospital in Malawi.” Paediatrics and International Child Health 40.3 (2020): 148-157.
- 5Hadi Atassi, Thomas L Abell, Romesh Khardori. “Protein-Energy Malnutrition Workup.” Medscape. Publishing 2019
- 6Training course on the inpatient management of severe acute malnutrition: facilitator’s guide.” (2021)
- 7Collins, Steve. “Reflections on the United Nations Draft Global Action Plan on wasting.” Field Exchange 62 (2020): 21. GLOBAL ACTION PLAN ON CHILD WASTING. A framework for action to accelerate progress in preventing and managing child wasting and the achievement of the Sustainable Development Goals
- 8Collins, Steve. “Reflections on the United Nations Draft Global Action Plan on wasting.” Field Exchange 62 (2020): 21. GLOBAL ACTION PLAN ON CHILD WASTING. A framework for action to accelerate progress in preventing and managing child wasting and the achievement of the Sustainable Development Goals
- 9Alou, Maryam Tidjani, et al. “Difference between kwashiorkor and marasmus: Comparative meta-analysis of pathogenic characteristics and implications for treatment.” Microbial Pathogenesis 150 (2021): 104702.
- 10Munthali, Tendai, et al. “Mortality and morbidity patterns in under-five children with severe acute malnutrition (SAM) in Zambia: a five-year retrospective review of hospital-based records (2009–2013).” Archives of Public Health 73.1 (2015): 1-9.