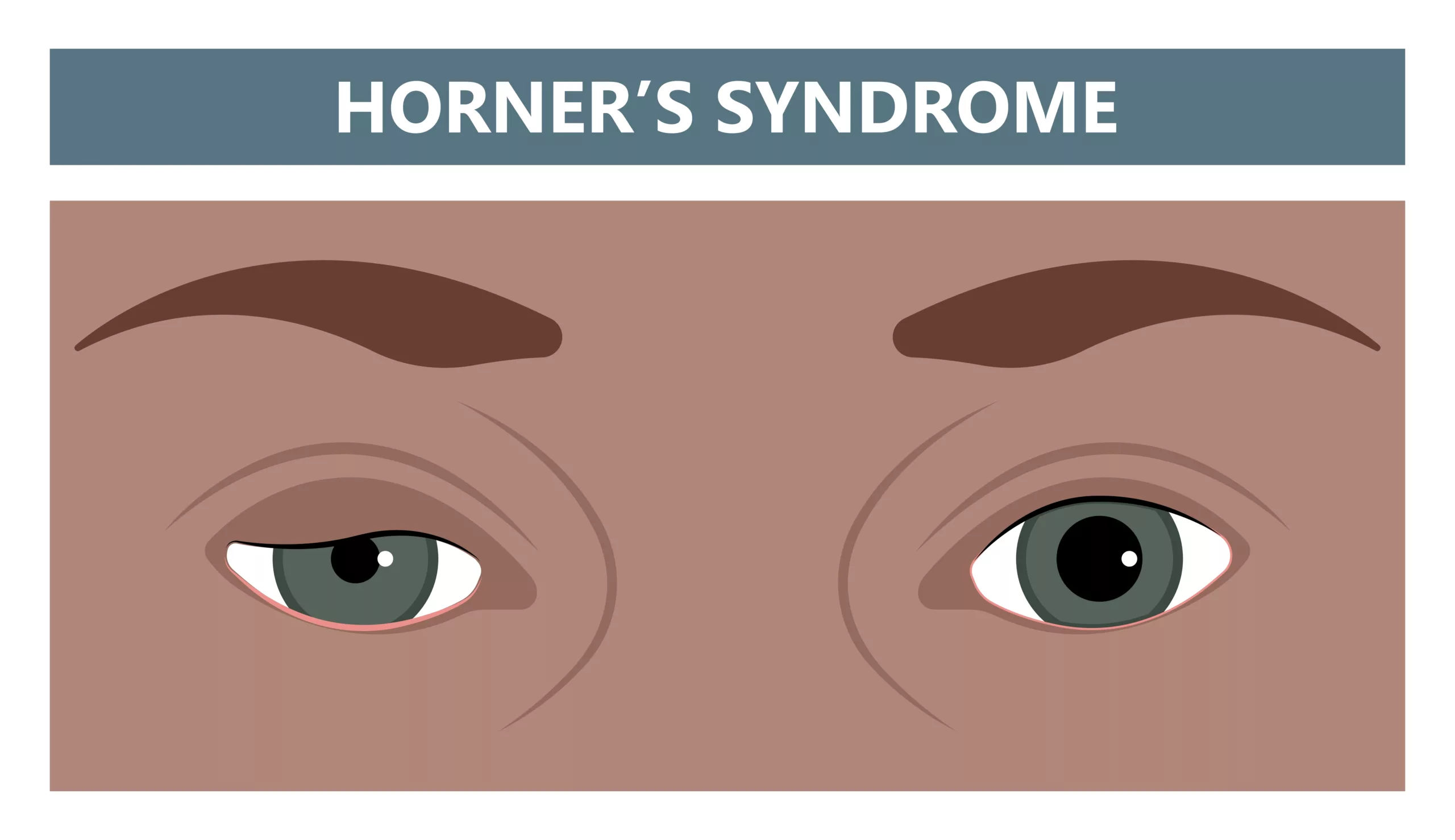
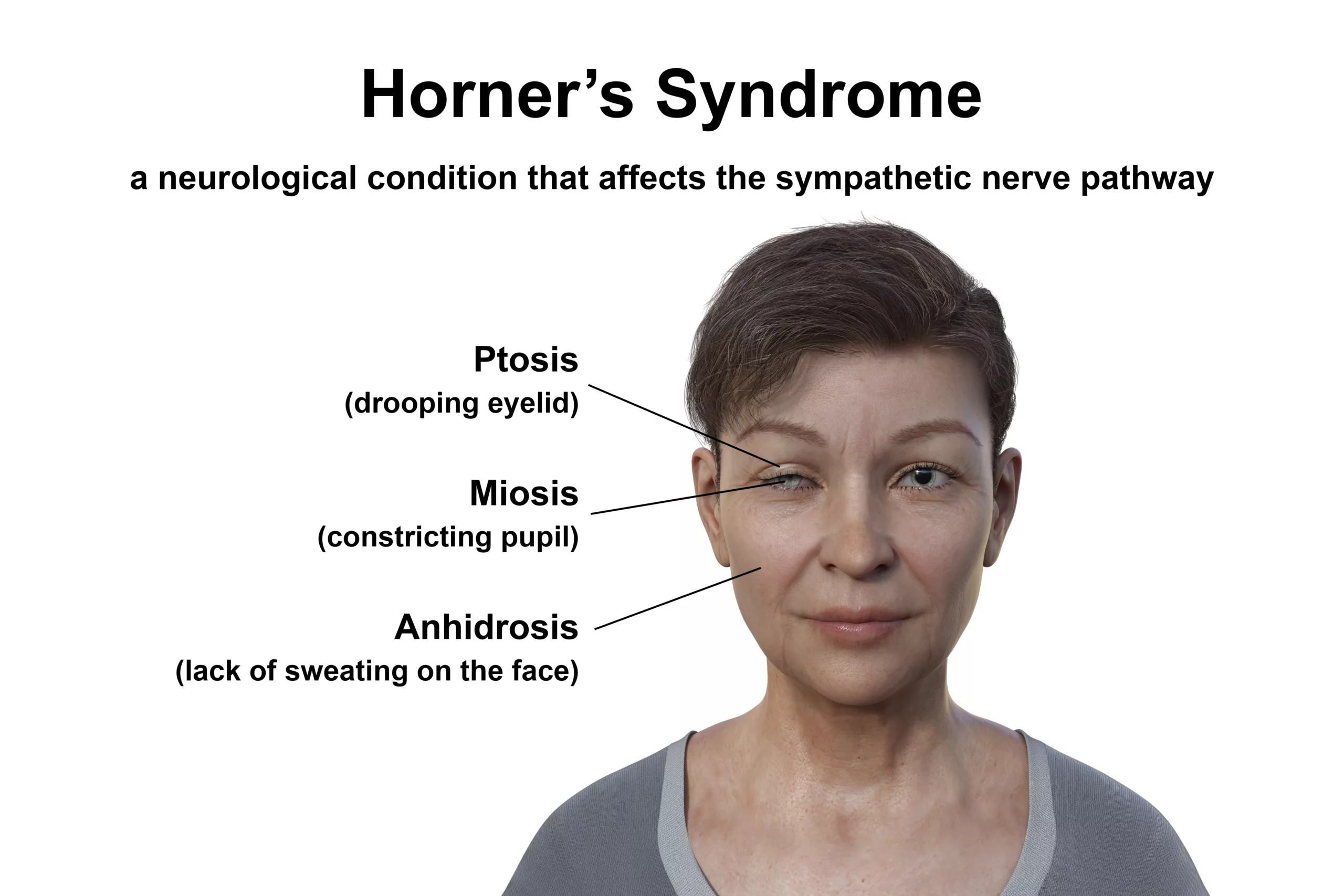
Horner’s Syndrome is a visual problem caused by damage to the sympathetic nerve supply. It affects the eye and the same side of the face. Paralysis of the sympathetic nerve supply causes drooping eyelids, constriction of pupils, and loss of sweating on the same side of the face. It is a rare condition and mostly occurs due to some injury.
What Is Horner’s Syndrome?
This syndrome is a triad of ptosis (dropping or falling of your eyelids), miosis (constriction of pupils), and anhidrosis (a decrease or lack of sweating) of the same side of your face.
It is also known as Bernard Horner’s Syndrome, Horner’s Syndrome, Oculosympathetic palsy, or Von Passow syndrome. It was first described by Swiss ophthalmologist Johann Friedrich Horner. He explained the effect of paralysis of the sympathetic nerve on the ipsilateral side (the same side) of the face and eye.1Thompson H. S. (1986). Johann Friedrich Horner (1831-1886). American Journal of Ophthalmology, 102(6), 792–795. https://doi.org/10.1016/0002-9394(86)90411-3
Symptoms Of Horner’s Syndrome
There are the following symptoms of Horner’s syndrome, apart from its triad, include the following:
- Different size of your pupils
- Failure to change the color of the iris in children and different colored iris (Heterochromia) as a result.
- The sunken appearance of your eyes
- The affected eye may appear red
- Delay in dilation of the pupil of your affected eye in dim light
- Flushing of the face on performing any physical activity
Causes Of Horner’s Syndrome
This syndrome is an acquired condition that may have several causes, such as diseases, nerve injury, birth trauma, and iatrogenic or secondary causes.2Biousse, V., Touboul, P. J., D’Anglejan-Chatillon, J., Lévy, C., Schaison, M., & Bousser, M. G. (1998). Ophthalmologic manifestations of internal carotid artery dissection. American Journal of Ophthalmology, 126(4), 565–577. https://doi.org/10.1016/s0002-9394(98)00136-6
However, horner’s syndrome can be congenital as well.
Iatrogenic causes can damage the sympathetic fibers in their extra cranial, intracranial, or intraorbital part. So, we divide the causes into three categories:
Involvement of First Order Neurons
If there is some intracranial cause, it means Horner’s syndrome involves first-order neurons of your ocular pathway. These causes include:
- Multiple sclerosis
- Cerebrovascular accident (CVA)
- Syringomyelia
- Encephalitis
- Meningitis
- Arnold Chiari Malformation
- Lateral medullary Syndrome
- Spinal cord tumor
- Spinal cord trauma above the second and third thoracic vertebrae (T2-T3)
- Neuroblastoma3Smith, S. J., Diehl, N., Leavitt, J. A., & Mohney, B. G. (2010). Incidence of pediatric Horner syndrome and the risk of neuroblastoma: a population-based study. Archives of ophthalmology (Chicago, Ill.: 1960), 128(3), 324–329. https://doi.org/10.1001/archophthalmol.2010.6
Involvement of Second Order Neurons
Second-order neurons are in the thoracic region. The following conditions can lead to their damage:
- Trauma to brachial plexus
- Thoracic rib
- Subclavian artery aneurysm
- Mediastinal lymphadenopathy
- Dental abscess
- Pancoast tumor (A malignancy involving your lungs)
- Surgeries like tonsillectomy, thyroidectomy, radical neck dissection, coronary artery bypass grafting, and other neck surgeries.4Sandoval, M. A., & Cabungcal, A. C. (2015). Horner syndrome after radical neck surgery for anaplastic thyroid carcinoma. BMJ case reports 2015, bcr2015209324. https://doi.org/10.1136/bcr-2015-2093245Kucur, C., Ozbay, I., Oghan, F., Yildirim, N., Zeybek Sivas, Z., & Canbaz Kabay, S. (2015). A Rare Complication of Radiofrequency Tonsil Ablation: Horner Syndrome. Case reports in otolaryngology, 2015, 570520. https://doi.org/10.1155/2015/570520
Involvement of Third Order Neurons
Third-order neurons lie near the cavernous sinus and your internal carotid artery. The following conditions affect them, causing Horner’s Syndrome:6Allen, A. Y., & Meyer, D. R. (2009). Neck procedures resulting in Horner syndrome. Ophthalmic plastic and reconstructive surgery, 25(1), 16–18. https://doi.org/10.1097/IOP.0b013e318191febf
- Herpes zoster infection
- Temporal arteritis
- Internal carotid artery aneurysm or dissection of carotid artery7Pirouzian, A., Holz, H. A., Ip, K. C., & Sudesh, R. (2010). Acquired infantile Horner syndrome and spontaneous internal carotid artery dissection: a case report and review of the literature. Journal of AAPOS: the official publication of the American Association for Pediatric Ophthalmology and Strabismus, 14(2), 172–174. https://doi.org/10.1016/j.jaapos.2009.12.169
- Carotid cavernous fistula
- Raeder para trigeminal syndrome
How Common Horner’s Syndrome Is?
This is a rare condition. It occurs in one out of six thousand people without age, gender, or race specification.
How Does Horner’s Syndrome Occur?
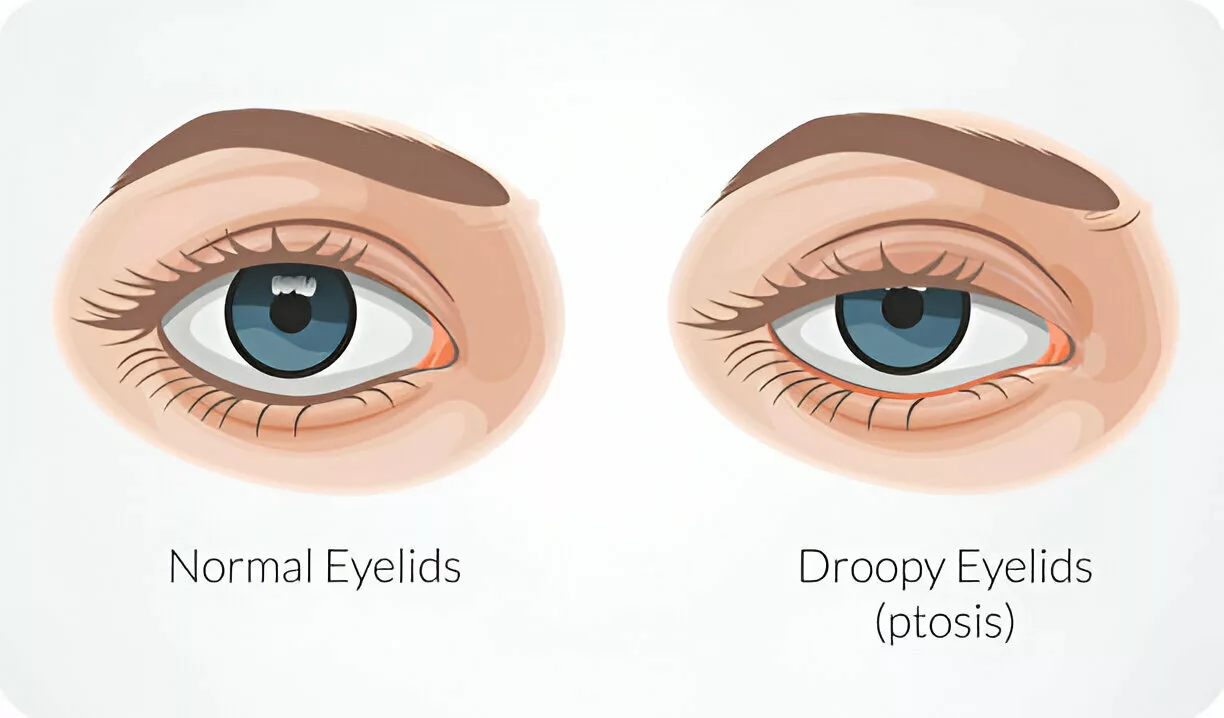
This syndrome occurs due to sympathetic disruption that affects the eye muscles. Failure of the superior tarsal muscles results in the dropping of eyelids because they are responsible for eyelid elevation.
Moreover, sympathetic innervation is responsible for the dilation of the eyes, and its damage causes miosis. And lastly, anhidrosis results from damage to the vasomotor fibers that cause sweating on your face.8Walker, L., & French, S. (2014). Horner’s Syndrome: A Case Report and Review of the Pathophysiology and Clinical Features. The West Indian Medical Journal, 63(3), 278–280. https://doi.org/10.7727/wimj.2014.004
How Is Horner’s Syndrome Diagnosed?
History:
The history involves the following important questions:
- History of trauma, surgery (particularly neck surgery), type of anesthesia during surgery, and any mydriatic drugs.
- History of double vision, headache, facial numbness, flushing, or pain.
- History of anhidrosis, skin lesions, paraganglionic involvement, and pain.
Examination:
Detailed examination is important for the diagnosis of this syndrome; it includes the following steps apart from general examination:
Eye Examination
- Pupillary light reflex
- Accommodation reflex
- Measurements of size and dilation of pupil
- Assessment of extraocular movements
- Visual field, visual acuity, and color vision assessment
- Slit lamp examination
Moreover, your doctor assesses partial ptosis, heterochromia, enophthalmos, lid retraction, and exophthalmos.
Pharmaceutical Tests:
The following pharmaceutical tests for Horner’s syndrome:
Topical Cocaine Test
In a topical cocaine test, your doctor instills a few drops of cocaine in your eyes and observes them after thirty minutes. Poor dilatation of the pupil of the affected eye indicates damage to the sympathetic nerve supply. However, it does not indicate the level of lesion.
Topical Hydroxyamphetamine Test
A topical Hydrophile test is useful for detecting the level of the lesion. It stimulates the release of norepinephrine from the postsynaptic ganglions. Your doctor instills a few drops of amphetamine in both your eyes; if the lesion is at the level of third-order neurons, the affected eye fails to dilate normally like the normal eye. But if the lesion is at the level of first—or second-order neurons, the response is normal.
Apraclonidine Test
The apraclonidine test is the test of choice for Horner’s syndrome. This test uses Apraclonidine, an alpha 1 and alpha 2 receptor agonist. In this test, your doctor instills a few drops of apraclonidine in your eyes and observes it after thirty minutes. The affected eye shows dilatation of the pupil, while the normal eye remains insensitive. Repeated instillation of apraclonidine in your eyes results in the reversal of anisocoria; your normal eye constricts, and the affected eye dilates.
Other pharmaceutical tests involve adrenaline and phenylephrine tests.
Laboratory Investigations:
Laboratory investigations for this syndrome include:
- Complete blood test (CBC)
- Erythrocyte sedimentation rate (ESR)
- Urine culture
- Blood culture
- Vitamin B12 and folate levels
- Thyroid function tests
- Urine assessment for catecholamines
- HIV and infection screening
- Purified protein derivative (PPD) for the detection of tuberculosis
Imaging Modalities:
- X-ray chest and CT chest are used to detect any malignancy of the lungs, like a Pancoast tumor
- Head CT scan and magnetic resonance imaging (MRI) for stroke patients
- Doppler Ultrasound of the affected vessels in case of vascular causes
- Biopsy of temporal artery in case of temporal arteritis
What Is The Management Of Horner’s Syndrome?
Management steps for the treatment include:
Treatment Of The Cause:
Management of Horner’s syndrome involves treating its cause at the first step. Your doctor will treat the underlying pathology at this step, which is beneficial in resolving these symptoms. If the cause is a middle ear infection, the doctor treats it first.
Surgical Treatment:
Surgical options are also related to the treatment of the cause; they include:
- Surgical treatment of the aneurysm of the carotid artery includes aneurysm clipping, aneurysm coiling, endovascular repair, and shunting.
- Vascular care for the carotid dissection.
- Surgical removal of the lung tumor, neuroblastoma, or any other malignancy.
- Surgery to relieve compression on your nerve pathways.
Pharmaceutical Management:
Pharmaceutical treatment involves the use of corticosteroids, beta-blockers, and anticholinesterase drugs. These drugs are very helpful in managing the symptoms of Horner’s syndrome.
Eyelid Crutches:
Your doctor can advise using eyelid crutches to support your drooping eyelid.
Botulinum Toxin Injections:
Botulinum toxin injections are useful for treating Horner’s syndrome in some cases.
Prism lenses:
If you have a complaint of double vision (diplopia), your doctor may recommend prism lenses to correct it.
Physiotherapy:
Your doctor may advise you on physiotherapy to improve your quality of life.
What Is The Prognosis Of Horner’s Syndrome?
This syndrome itself has a good prognosis, and that depends on treating the underlying cause. Symptoms like ptosis and miosis start improving as soon as the underlying cause is treated. However, if the underlying cause is serious and chronic, like some malignancy, it can be chronic, and the prognosis is not good.

What Are The Complications Of Horner’s Syndrome?
Horner’s syndrome itself does not have any complications, but the underlying causes, like malignancy and tumors, can lead to many complications. For example, if Horner’s syndrome occurs due to multiple sclerosis in a patient, it can cause various complications like muscle spasms, bladder dysfunction, seizures, or sexual dysfunction. Visual dysfunction can worsen as well.
Some underlying causes, like carotid aneurysms and cerebrovascular accidents like stroke, can be life-threatening as well.
Horner’s Syndrome Vs. Adie’s Pupil
| Horner’s Syndrome | Adie’s Pupil | |
| Definition | Horner’s syndrome is a triad of miosis, ptosis, and anhidrosis. | In Adie’s pupil, one or both pupils are abnormally dilated and do not constrict in response to light. |
| Causes | Causes of Horner’s syndrome include nerve injury, birth trauma, stroke, and carotid dissection. | The causes of Adie’s pupil include inflammation, Guillain-Barre Syndrome, Human papillomavirus, and syphilis. |
| Pathophysiology | There is damage to the sympathetic innervation of the eye in Horner’s syndrome. | There is damage to post-ganglionic fibers of the ciliary ganglion due to inflammation. |
Does Horner’s Syndrome Cause Blindness?
This is a benign condition that doesn’t often cause serious eye problems. However, it can cause visual problems in some cases, and temporary or permanent blindness occurs in severe cases when the nerve is damaged.
Is Horner’s Syndrome Related To Epidural Anaesthesia In Pregnant Ladies?
If the doctor gives epidural anesthesia to the pregnant lady during a C-Section or for pain relief, the spinal block can include your facial area and eye. Mostly, it does not cause severe manifestations, but it can also cause Transient Horner’s syndrome. However, these symptoms are temporary and resolve spontaneously without any particular treatment except in a few cases.9Biousse, V., Guevara, R. A., & Newman, N. J. (1998). Transient Horner’s syndrome after lumbar epidural anesthesia. Neurology, 51(5), 1473–1475. https://doi.org/10.1212/WNL.51.5.1473
Does Brachial Plexus Injury Cause Horner’s Syndrome?
The sympathetic nerve fibers of the face and arms are connected to the brachial plexus, which can be injured and lead to Horner’s syndrome. Brachial plexus injury can occur due to trauma, tumors, radiotherapy, inflammation, stretching of nerve fibers, or birth trauma.
What Is The Relation Of Birth Trauma To Horner’s Syndrome?
Birth trauma in newborns can damage the brachial plexus and the sympathetic nerves, resulting in Horner’s syndrome. Birth trauma can occur due to forceps delivery with poor technique, shoulder dystocia, pulling the hands of the baby too forcefully, and trying to deliver a breech presentation. So, there is a need to be careful during delivery. The doctors foresee expected complications of delivery and plan an adequate method for the delivery of the baby in such conditions.
What Is the Relationship Between Raeder ParaTrigeminal Syndrome And Horner’s Syndrome?
Raeder para trigeminal syndrome occurs in males, and it involves Horner’s syndrome along with unilateral headache. In fact, it is a problem in the trigeminal nerve, causing pain and anesthesia or hypoesthesia along the distribution of your trigeminal nerve.
Which nerve, trunk, and ganglia are affected By Horner’s syndrome?
In Horner’s syndrome, the sympathetic trunk and cervicothoracic ganglia are affected. The lesion originates from the eighth cervical (C8) to the first thoracic (T1) vertebrae. The trigeminal nerve is affected by Horner’s Syndrome. The stellate ganglion is affected if the lesion is in your upper neck. The lesion can involve any first, second, or third-order neurons.
Is Horner’s Syndrome A Genetic Condition?
No, Horner’s syndrome is not a genetic condition but an acquired one. Sometimes, congenital Horner syndrome can occur in children due to birth trauma or injury to the carotid artery during birth.
Can Carotid Artery Dissection Cause Horner’s Syndrome?
Carotid artery dissection leads to Horner’s syndrome. The reason behind this is that the tear in the carotid artery causes separation of its layers and damage to the sympathetic fibers, or its dissection may disrupt the sympathetic trunk or injure the nearby sympathetic fibers along the carotid artery. All of these can cause Horner’s syndrome.
What Other Consultations Are Required For The Patients Having Horner’s Syndrome?
If an ophthalmologist suspects Horner’s syndrome in a patient, he needs other consultations, such as pulmonology, neurology, neuro-ophthalmology, radiology, and oncology. These checkups aim to identify the cause of this syndrome and rule out other pathologies.
Conclusion
Horner’s syndrome is a triad of ptosis, miosis, and anhidrosis. It is a rare condition that is secondary to some other causes. However, it can be congenital as well. It has no specific treatment and resolves itself with the treatment of cause.
Refrences
- 1Thompson H. S. (1986). Johann Friedrich Horner (1831-1886). American Journal of Ophthalmology, 102(6), 792–795. https://doi.org/10.1016/0002-9394(86)90411-3
- 2Biousse, V., Touboul, P. J., D’Anglejan-Chatillon, J., Lévy, C., Schaison, M., & Bousser, M. G. (1998). Ophthalmologic manifestations of internal carotid artery dissection. American Journal of Ophthalmology, 126(4), 565–577. https://doi.org/10.1016/s0002-9394(98)00136-6
- 3Smith, S. J., Diehl, N., Leavitt, J. A., & Mohney, B. G. (2010). Incidence of pediatric Horner syndrome and the risk of neuroblastoma: a population-based study. Archives of ophthalmology (Chicago, Ill.: 1960), 128(3), 324–329. https://doi.org/10.1001/archophthalmol.2010.6
- 4Sandoval, M. A., & Cabungcal, A. C. (2015). Horner syndrome after radical neck surgery for anaplastic thyroid carcinoma. BMJ case reports 2015, bcr2015209324. https://doi.org/10.1136/bcr-2015-209324
- 5Kucur, C., Ozbay, I., Oghan, F., Yildirim, N., Zeybek Sivas, Z., & Canbaz Kabay, S. (2015). A Rare Complication of Radiofrequency Tonsil Ablation: Horner Syndrome. Case reports in otolaryngology, 2015, 570520. https://doi.org/10.1155/2015/570520
- 6Allen, A. Y., & Meyer, D. R. (2009). Neck procedures resulting in Horner syndrome. Ophthalmic plastic and reconstructive surgery, 25(1), 16–18. https://doi.org/10.1097/IOP.0b013e318191febf
- 7Pirouzian, A., Holz, H. A., Ip, K. C., & Sudesh, R. (2010). Acquired infantile Horner syndrome and spontaneous internal carotid artery dissection: a case report and review of the literature. Journal of AAPOS: the official publication of the American Association for Pediatric Ophthalmology and Strabismus, 14(2), 172–174. https://doi.org/10.1016/j.jaapos.2009.12.169
- 8Walker, L., & French, S. (2014). Horner’s Syndrome: A Case Report and Review of the Pathophysiology and Clinical Features. The West Indian Medical Journal, 63(3), 278–280. https://doi.org/10.7727/wimj.2014.004
- 9Biousse, V., Guevara, R. A., & Newman, N. J. (1998). Transient Horner’s syndrome after lumbar epidural anesthesia. Neurology, 51(5), 1473–1475. https://doi.org/10.1212/WNL.51.5.1473