Pierre Robin Syndrome, a rare congenital disorder, manifests with facial and mouth deformities that impede breathing. It can occur independently or alongside syndromes like Stickler or Treacher Collins. Common symptoms include a small lower jaw, backward-placed large tongue, and cleft palate.
The term “Pierre Robin Sequence” has replaced “Pierre Robin Syndrome” to describe the pathology better. Diagnosis typically relies on newborn physical examination, although imaging techniques and breathing/feeding tests can aid confirmation. Despite its various anomalies, proper interventions and therapies generally yield a favorable prognosis for children with PRS.
The estimated occurrence rate ranges from 1 in 8,500 to 1 in 14,000 births1Izumi, K., Konczal, L. L., Mitchell, A. L., & Jones, M. C. (2012). Underlying Pierre Robin sequence genetic diagnosis: retrospective chart review at two children’s hospitals and a systematic literature review. The Journal of Pediatrics, 160(4), 645–650.e2. https://doi.org/10.1016/j.jpeds.2011.09.021.
What is Pierre Robin Syndrome?
Pierre Robin Syndrome, also referred to as Pierre Robin Sequence or Robin Sequence, encompasses a cluster of abnormalities affecting the head and face. Characteristics include a small lower jaw (micrognathia), abnormally positioned tongue (glossoptosis), and breathing difficulties arising from airway obstruction. These combined features can result in early-life breathing and feeding challenges. Consequently, affected infants may struggle with growth and weight gain. Untreated airway obstruction can lead to complications such as hypoxia, right heart failure, failure to thrive, feeding difficulties, and potential cerebral impairment. Furthermore, many individuals with Pierre Robin Sequence also have a cleft palate, further impacting their feeding abilities.
The term “sequence” is used to describe this condition due to the sequential events that occur during fetal development. Although the exact cause remains uncertain, the series of anomalies observed in utero typically initiates with an underdeveloped jaw, leading to tongue displacement and the subsequent formation of a U-shaped cleft palate. While some research indicates a potential genetic component, other theories propose factors such as uterine crowding or specific neurological conditions.2Johns Hopkins Medicine. (n.d.). Pierre Robin Sequence. Retrieved from https://www.hopkinsmedicine.org/health/conditions-and-diseases/pierre-robin-sequence#:~:text=What%20You%20Need%20to%20Know,tongue%20and%20upper%20airway%20obstruction.

Causes Of Pierre Robin Syndrome
The exact cause of Pierre Robin Sequence (PRS) is not fully understood. However, it is believed to result from a combination of genetic and environmental factors. Pierre Robin Syndrome is of two types: isolated and syndromic.
Isolated/Non-Syndromic Pierre Robin Syndrome
In isolated or non-syndromic PRS, there are mutations in different chromosomes, like 2, 4, 11, or 17. Emerging evidence indicates that mutations in genes such as SOX9 or KCNJ2, located on chromosome 17, could potentially influence the formation of facial structures and cartilage development, thus contributing to the occurrence of Pierre Robin Sequence (PRS).3Gangopadhyay, N., Mendonca, D. A., & Woo, A. S. (2012). Pierre Robin sequence. Seminars in plastic surgery, 26(2), 76–82. https://doi.org/10.1055/s-0032-1320065 Twins and family members of these babies are more likely to have related conditions such as cleft lip and cleft palate.
Syndromic Pierre Robin Syndrome
On the other hand, syndromic PRS, which constitutes about 60% of cases, is linked to other conditions.4Izumi, K., Konczal, L. L., Mitchell, A. L., & Jones, M. C. (2012). Underlying genetic diagnosis of Pierre Robin sequence: retrospective chart review at two children’s hospitals and a systematic literature review. The Journal of Pediatrics, 160(4), 645–650.e2. https://doi.org/10.1016/j.jpeds.2011.09.021 These syndromes include:
Stickler Syndrome
In Stickler syndrome, there’s a mutation in a gene, which is needed for collagen formation.
The mutation causes features like a flat midface, eye problems, joint flexibility, hearing problems, and typical PRS signs. About 47% of PRS children have stickler syndrome.5Karempelis, P., Hagen, M., Morrell, N., & Roby, B. B. (2020). Associated syndromes in patients with Pierre Robin Sequence. International Journal of pediatric otorhinolaryngology, 131, 109842. https://doi.org/10.1016/j.ijporl.2019.109842
Velocardiofacial Syndrome
In Velocardiofacial syndrome, there’s a deletion of a specific gene. It affects the heart, thymus, parathyroid, and facial development, leading to unique facial characteristics, slender fingers, hypothyroidism, immune issues, hearing loss, and heart defects.
Treacher Collins Syndrome
Treacher-Collins syndrome, also associated with PRS, leads to underdeveloped facial bones, problems with the jaw joint, cleft palate, and ear anomalies.6Giudice, A., Barone, S., Belhous, K., Morice, A., Soupre, V., Bennardo, F., Boddaert, N., Vazquez, M. P., Abadie, V., & Picard, A. (2018). Pierre Robin sequence: A comprehensive narrative review of the literature over time. Journal of stomatology, oral and maxillofacial surgery, 119(5), 419–428. https://doi.org/10.1016/j.jormas.2018.05.002
Pierre Robin Syndrome Symptoms
The major symptoms of Pierre Robin syndrome are:
Micrognathia
The mandible is underdeveloped, with a shortened body length and increased angle.
Glossoptosis
This refers to the displacement of the base of the tongue toward the pharynx. The severity of glossoptosis can vary widely, leading to differing degrees of respiratory distress.
Airway Obstruction
Ranges from mild to severe respiratory compromise, affecting breathing, feeding, and long-term health.
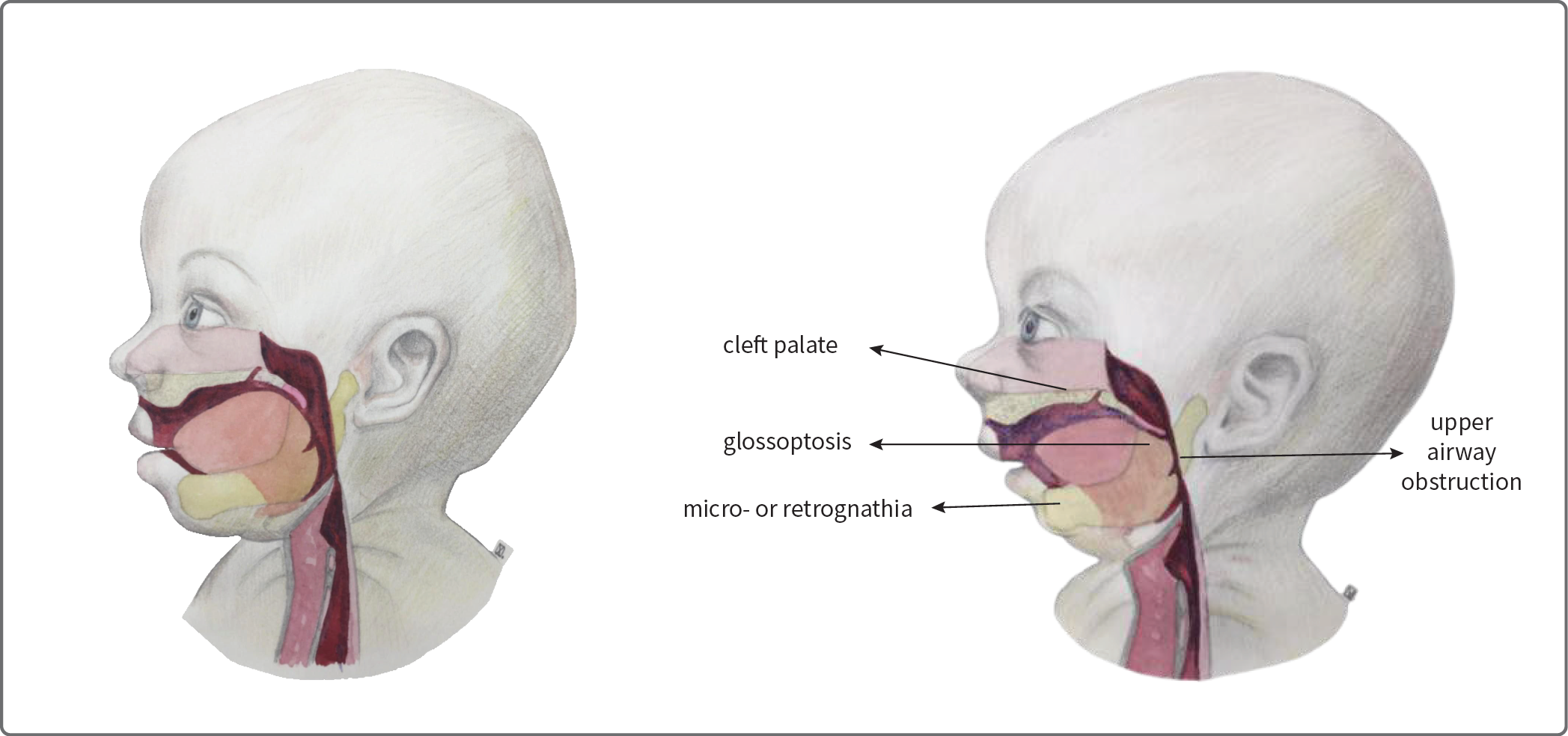
Image courtesy: Lozar Krivec, J., Železnik, M., Eberlinc, A., Gluvajić, D., & Krivec, U. (2022, April 30). Pierre Robin Sequence: Treatment with Nasopharyngeal Tube. Slovenian Medical Journal. DOI: 10.6016/ZdravVestn.3194
Other common symptoms include:
- Large tongue or tight tongue attachment
- Cleft lip and palate
- Ear infections
- Abnormalities in the outer ear
- Hearing loss (Usually conductive, affecting many patients)
- Blocked ear canal (External auditory canal atresia)
- Nose shape deformity
- Dental malformations like crowding
- Eye problems
- Heart problems like murmurs, valve problems
- Bone and muscle problems
- Central nervous system (CNS) defects – like language delays or epilepsy
- Genitourinary defects (undescended testes, hydronephrosis, and hydrocele)
Diagnosing Pierre Robin Syndrome (PRS)
Diagnostic Evaluation During Pregnancy
During pregnancy, ultrasound examination plays a vital role in identifying potential signs of Pierre Robin Sequence (PRS), such as micrognathia (underdeveloped jaw) and polyhydramnios (excessive amniotic fluid). These findings raise concern for PRS and necessitate further diagnostic steps. Prenatal diagnosis is essential as it enables healthcare providers to counsel parents regarding potential complications and treatment options. Prenatal diagnosis is crucial for counseling parents about potential complications and treatment options. Amniocentesis with microarray may be recommended for further evaluation, particularly when genetic syndromes are suspected. Referral to a genetic counselor is advisable.
Diagnosis after Birth
Diagnosing Pierre Robin Syndrome typically occurs shortly after birth through a combination of clinical evaluation and diagnostic tests. Immediate assessment in the delivery room is crucial to determine if urgent airway interventions are necessary.
- Clinical Examination: During a physical check-up, healthcare providers assess the baby’s facial features, jaw size, and signs of respiratory distress. Continuous monitoring of oxygen saturation aids in detecting respiratory issues. Medical professionals may conduct further diagnostic procedures, such as polysomnography, nasoendoscopy, or bronchoscopy, to assess the severity of airway obstruction. Evaluating feeding abilities and monitoring growth charts help determine the need for nutritional support, including nasogastric tube feeding if required.
- Imaging Studies: X-rays, CT scans, or MRIs visualize the jaw and palate structures. A bronchoscope may be employed to inspect the airway for any obstructions.
- Genetic Testing: Medical professionals may sometimes recommend genetic testing to identify related genetic issues or syndromes associated with Pierre Robin Syndrome.
Pierre Robin Syndrome Treatment
Treatment for Pierre Robin Sequence aims to ensure the baby can eat and breathe safely and comfortably. Since there are different symptoms involved in Pierre Robin Syndrome, the treatment plan includes medical approaches from different fields. Your baby’s treatment team will have a:
- Pediatrician/neonatologist
- Craniofacial surgeon
- Geneticist
- Ophthalmologist
- Otorhinolaryngologist (ENT surgeon)
- Pulmonologist
- Speech pathologist
Here are the different aspects of a treatment plan for PRS:
Monitoring & Supportive Care
Scheduled doctor appointments are needed to assess the child’s growth, development, and overall health.
Management of Airway and Breathing
Children with the Pierre Robin Sequence may experience difficulty obtaining sufficient oxygen due to glossoptosis, where the tongue abnormally positions further back in the mouth.
Non-Surgical management:
Non-surgical interventions to aid breathing include:
Positional Therapy
It is required to help the baby sleep in a comfortable position. Placing the baby in a slightly inclined or lateral (side) position while sleeping helps prevent the tongue from falling back into the throat, reducing the risk of airway obstruction.
Studies say that 70% of PRS babies recover just by positional therapy and other conventional interventions without any surgery.7Côté, A., Fanous, A., Almajed, A., & Lacroix, Y. (2015). Pierre Robin sequence: a review of diagnostic and treatment challenges. International Journal of pediatric otorhinolaryngology, 79(4), 451–464. https://doi.org/10.1016/j.ijporl.2015.01.035
Nasopharyngeal Airway/ Intubation
Intubation is a procedure to ensure that a person can breathe well, especially when the airway is at risk of getting blocked.
Nasopharyngeal intubation means putting a breathing tube through the nose into the upper part of the throat (nasopharynx) to maintain an open airway and facilitate breathing. This tube requires periodic replacement and may need adjustments as the baby grows.8Cladis, F., Kumar, A., Grunwaldt, L., Otteson, T., Ford, M., & Losee, J. E. (2014). Pierre Robin Sequence: a perioperative review. Anesthesia and analgesia, 119(2), 400–412. https://doi.org/10.1213/ANE.0000000000000301 Doctors need to watch and take care of the airway in babies with PRS to avoid problems linked to breathing difficulties.
Surgical Interventions
Surgical interventions for managing the airway include:
Tongue-Lip Adhesion:
This procedure involves repositioning the tongue by attaching its base to the lower lip. The procedure helps maintain a stable airway until surgeons repair the baby’s cleft palate, typically around 9 to 11 months of age, after which they reverse the procedure.
Mandibular Distraction Osteogenesis
This surgical intervention lengthens the lower jaw bone. It involves gradually stretching divided segments of the jaw to generate new bone.
It is done to improve the airway and alleviate breathing difficulties by creating more space in the mouth.

Management of Feeding Difficulties
In treating feeding difficulties associated with the Pierre Robin Sequence, a multidisciplinary team monitors the child’s growth and weight gain closely. They may recommend the following interventions:
- Specialty Feeders: The Haberman feeder is commonly used for infants with Pierre Robin Sequence or cleft palate. It features a unique design with a one-way valve separating the nipple from the bottle, helping even weak suckers to feed effectively. Benefits include reducing issues like vomiting and colic, with adjustable flow settings and the ability to apply compression to aid feeding.
- Nasogastric Feeding Tube (NG tube): Medical professionals pass this flexible tube through the baby’s nose into the stomach, providing a temporary solution to ensure weight gain over weeks to months.
- Gastrostomy Feeding Tube (G-tube): Surgically inserted directly into the stomach, the G-tube provides long-term nutrition support over six months to years, offering a more permanent solution for feeding difficulties.
Cleft Palate Repair
About 90% of the babies with PRS have cleft palate defects.9Santoro, M., Coi, A., Barišić, I., Pierini, A., Addor, M. C., Baldacci, S., Ballardini, E., Boban, L., Braz, P., Cavero-Carbonell, C., de Walle, H. E. K., Draper, E. S., Gatt, M., Haeusler, M., Klungsøyr, K., Kurinczuk, J. J., Materna-Kiryluk, A., Lanzoni, M., Lelong, N., Luyt, K., … Garne, E. (2021). Epidemiology of Pierre-Robin sequence in Europe: A population-based EUROCAT study. Pediatric and perinatal epidemiology, 35(5), 530–539. https://doi.org/10.1111/ppe.12776 If a cleft palate is present, surgical correction is performed to close the gap in the roof of the mouth. This helps with feeding, prevents nasal regurgitation, and supports speech development.
Orthodontic Interventions
Orthodontic interventions may include using special devices to address dental and jaw alignment issues as the child grows. These interventions contribute to normal facial development.
Speech Therapy
A cleft palate can lead to speech difficulties. So, speech therapy is designed to address these difficulties. Therapists work on improving articulation, language skills, and overall communication development.
Is Surgery Always Required For Pierre Robin Syndrome?
The simple answer: No. PRS is divided into two severity categories: mild to moderate and severe.
Moderate Pierre Robin Syndrome
Children with mild to moderate PRS won’t need surgery since their small jaw tends to get bigger as they grow. Simple measures like changing sleeping positions, nasal breathing, and feeding tubes can often help with eating and breathing. Some people use devices like CPAP, but it can be challenging for patients.
Severe Pierre Robin Syndrome
Severe cases usually need surgery. Syndromic PRS almost always requires surgery, while only about 10% of isolated PRS cases do. Surgeons perform tongue-lip adhesion, mandibular distraction osteogenesis, and conduct tracheostomy, often reserved for severe cases, as surgical options. It’s a standard for airway protection but comes with potential complications like infections and longer ICU stays. Corrective surgery for a cleft palate may also be needed, but not immediately.
Because babies with PRS are more likely to get ear infections, doctors might suggest ear tube surgery to address this issue. It’s essential to discuss the best approach for your child’s specific situation with their healthcare team.
Pierre Robin Syndrome Life Expectancy – What’s the prognosis?
Most kids with the Pierre Robin sequence can expect a positive outcome if they receive early treatment and regular check-ups from an experienced medical team. This helps prevent any issues that might arise due to the condition.10Logjes, R. J. H., Haasnoot, M., Lemmers, P. M. A., Nicolaije, M. F. A., van den Boogaard, M. H., Mink van der Molen, A. B., & Breugem, C. C. (2018). Mortality in Robin sequence: identification of risk factors. European Journal of Pediatrics, 177(5), 781–789. https://doi.org/10.1007/s00431-018-3111-4
Studies have found that the death rate in PRS is highest in the first year of life – calling it the critical period. However, with early interventions and proper care, 95% of the children get better up to the age of 10.11Santoro, M., Garner, E., Coi, A., Tan, J., Loane, M., Ballardini, E., Cavero-Carbonell, C., de Walle, H. E., Gatt, M., Gissler, M., Jordan, S., Klungsøyr, K., Lelong, N., Urhoj, S. K., Wellesley, D. G., & Morris, J. K. (2023). Survival, hospitalization, and surgery in children born with Pierre Robin sequence: a European population-based cohort study. Archives of disease in childhood, 108(7), 550–555. https://doi.org/10.1136/archdischild-2022-324716
To sum it up, Pierre Robin Syndrome, now known as Pierre Robin Sequence, is a rare congenital disorder of facial and mouth deformities that arise, affecting breathing and feeding. While interventions and therapies indicate a favorable prognosis, severe cases may require surgical intervention. Early treatment, regular monitoring, and a multi-disciplinary approach can help most children with PRS have positive outcomes, reflecting the role of timely interventions.
Refrences
- 1Izumi, K., Konczal, L. L., Mitchell, A. L., & Jones, M. C. (2012). Underlying Pierre Robin sequence genetic diagnosis: retrospective chart review at two children’s hospitals and a systematic literature review. The Journal of Pediatrics, 160(4), 645–650.e2. https://doi.org/10.1016/j.jpeds.2011.09.021
- 2Johns Hopkins Medicine. (n.d.). Pierre Robin Sequence. Retrieved from https://www.hopkinsmedicine.org/health/conditions-and-diseases/pierre-robin-sequence#:~:text=What%20You%20Need%20to%20Know,tongue%20and%20upper%20airway%20obstruction.
- 3Gangopadhyay, N., Mendonca, D. A., & Woo, A. S. (2012). Pierre Robin sequence. Seminars in plastic surgery, 26(2), 76–82. https://doi.org/10.1055/s-0032-1320065
- 4Izumi, K., Konczal, L. L., Mitchell, A. L., & Jones, M. C. (2012). Underlying genetic diagnosis of Pierre Robin sequence: retrospective chart review at two children’s hospitals and a systematic literature review. The Journal of Pediatrics, 160(4), 645–650.e2. https://doi.org/10.1016/j.jpeds.2011.09.021
- 5Karempelis, P., Hagen, M., Morrell, N., & Roby, B. B. (2020). Associated syndromes in patients with Pierre Robin Sequence. International Journal of pediatric otorhinolaryngology, 131, 109842. https://doi.org/10.1016/j.ijporl.2019.109842
- 6Giudice, A., Barone, S., Belhous, K., Morice, A., Soupre, V., Bennardo, F., Boddaert, N., Vazquez, M. P., Abadie, V., & Picard, A. (2018). Pierre Robin sequence: A comprehensive narrative review of the literature over time. Journal of stomatology, oral and maxillofacial surgery, 119(5), 419–428. https://doi.org/10.1016/j.jormas.2018.05.002
- 7Côté, A., Fanous, A., Almajed, A., & Lacroix, Y. (2015). Pierre Robin sequence: a review of diagnostic and treatment challenges. International Journal of pediatric otorhinolaryngology, 79(4), 451–464. https://doi.org/10.1016/j.ijporl.2015.01.035
- 8Cladis, F., Kumar, A., Grunwaldt, L., Otteson, T., Ford, M., & Losee, J. E. (2014). Pierre Robin Sequence: a perioperative review. Anesthesia and analgesia, 119(2), 400–412. https://doi.org/10.1213/ANE.0000000000000301
- 9Santoro, M., Coi, A., Barišić, I., Pierini, A., Addor, M. C., Baldacci, S., Ballardini, E., Boban, L., Braz, P., Cavero-Carbonell, C., de Walle, H. E. K., Draper, E. S., Gatt, M., Haeusler, M., Klungsøyr, K., Kurinczuk, J. J., Materna-Kiryluk, A., Lanzoni, M., Lelong, N., Luyt, K., … Garne, E. (2021). Epidemiology of Pierre-Robin sequence in Europe: A population-based EUROCAT study. Pediatric and perinatal epidemiology, 35(5), 530–539. https://doi.org/10.1111/ppe.12776
- 10Logjes, R. J. H., Haasnoot, M., Lemmers, P. M. A., Nicolaije, M. F. A., van den Boogaard, M. H., Mink van der Molen, A. B., & Breugem, C. C. (2018). Mortality in Robin sequence: identification of risk factors. European Journal of Pediatrics, 177(5), 781–789. https://doi.org/10.1007/s00431-018-3111-4
- 11Santoro, M., Garner, E., Coi, A., Tan, J., Loane, M., Ballardini, E., Cavero-Carbonell, C., de Walle, H. E., Gatt, M., Gissler, M., Jordan, S., Klungsøyr, K., Lelong, N., Urhoj, S. K., Wellesley, D. G., & Morris, J. K. (2023). Survival, hospitalization, and surgery in children born with Pierre Robin sequence: a European population-based cohort study. Archives of disease in childhood, 108(7), 550–555. https://doi.org/10.1136/archdischild-2022-324716