Anencephaly is a serious but rare birth defect. Babies with this birth defect are born without some portions of the brain and skull. The reason behind this anomaly lies in the abnormal development of the neural tube during infancy. The neural tube makes the baby’s brain and the whole nervous system. So, any problem with normal neural tube development can impact the baby’s nervous system.
Researchers have linked different genetic, nutritional, and environmental factors with anencephaly. These factors include lack of folic acid, excess vitamin A intake during pregnancy, some medicines, and maternal diabetes, which increase the risk for anencephaly.
Since the brain is crucial for controlling body functions, emotions, and memory, anencephaly affects the baby’s development. Sadly, babies born with anencephaly typically live only a few minutes, hours, or days. Most pregnancies with this condition end in miscarriage or stillbirth.
What is Anencephaly?
The term anencephaly is a Greek term that literally means “without a brain”. Anencephaly is a condition when a baby is born with a missing brain, skull, and scalp. It is a rare birth defect, and only 1-5 per 1000 babies are affected with this condition.1Oumer, M., Kibret, A. A., Girma, A., Tazebew, A., & Silamsaw, M. (2021). Prevalence of anencephaly in Africa: a systematic review and meta-analysis. Scientific reports, 11(1), 23707. https://doi.org/10.1038/s41598-021-02966-w During a baby’s development in the womb, a structure called a neural tube is formed. This tube is responsible for developing the brain, spinal cord, and nerves. In anencephaly, there’s a defect in the closure of the upper part of the neural tube, manifesting in the baby being born without the forebrain (front part of the brain) and the cerebrum (thinking and coordinating part of the brain). Typically, the remaining brain sections lack proper covering by bone or skin. The baby’s brain is exposed to the amniotic fluid, leading to brain and scalp degeneration.
What are the Causes of Anencephaly?
The exact cause behind the neural tube closure failure has not been determined. However, various factors like changes in chromosomes, the mother’s nutritional status, and environmental exposure during pregnancy may seem to play a role.2Centers for Disease Control and Prevention. (n.d.). Anencephaly. Retrieved January 30, 2024, from https://www.cdc.gov/ncbddd/birthdefects/anencephaly.html#:~:text=Some%20babies%20have%20anencephaly%20because,medicines%20she%20uses%20during%20pregnancy.
Here’s the list of risk factors for anencephaly:
Genetics
Most neural tube defects are linked to various factors, but certain families may experience rare cases inherited through genes. In instances with this genetic predisposition, families may have children who develop conditions like spina bifida or anencephaly.
Amniotic Band Disruption Sequence
Amniotic band disruption sequence is a condition that happens when the bag of water around the baby (amniotic sac) breaks. It causes problems with the normal development of a baby in the womb. It affects the structure of the hands, face, brain, and other body organs.
Folic Acid Deficiency
Folate, or vitamin B9, is an important nutrient that helps the body do various tasks, especially making DNA.
Taking 400 micrograms of folic acid every day before and during early pregnancy can help prevent neural tube defects, including anencephaly. Statistics have shown that since the United States started adding folic acid to grains, there’s been a 28% decrease in pregnancies affected by neural tube defects.3Mai CT, Isenburg JL, Canfield MA, Meyer RE, Correa A, Alverson CJ, Lupo PJ, Riehle‐Colarusso T, Cho SJ, Aggarwal D, Kirby RS. National population‐based estimates for major birth defects, 2010–2014. Birth Defects Research. 2019; 111(18): 1420-1435.
So, if you’re at risk for neural tube defects, talk to your doctor about taking a higher dose of folic acid.
Excessive Vitamin A Intake
Although there has not been much evidence that excess vitamin A intake causes anencephaly, 2017 research has found that excess vitamin A intake during pregnancy harms the baby.4Kondo, A., Matsuo, T., Morota, N., Kondo, A. S., Okai, I., & Fukuda, H. (2017). Neural tube defects: Risk factors and preventive measures. Congenital anomalies, 57(5), 150–156. https://doi.org/10.1111/cga.12227 It can cause different types of neural tube defects, for example, spina bifida or anencephaly.
Medicines
Pregnant women have to be vigilant while taking different medications because not every medicine is safe during pregnancy. Some drugs cause drastic effects on the baby.
For example, the anti-seizure drugs Valproate, Carbamazepine, Lamotrigine, and Phenytoin raise the risk of anencephaly. These drugs reduce the absorption of folic acid in the blood, thus leading to anencephaly.5Nojima, M., Kitahara, H., Yamada, Y., Nakazawa, A., Abe, M., Haga, N., & Shibasaki, J. (2016). Neurological teratogenic effects of antiepileptic drugs during pregnancy (Review). Experimental and Therapeutic Medicine, 12(5), 3628. https://doi.org/10.3892/etm.2016.3628
There are some other drugs as well that can cause anencephaly:
- Aspirin (pain reliever)
- Trimethoprim (anti-malarial drug)
- Triamterene (a diuretic)
Maternal Diabetes
If a woman has uncontrolled blood sugar levels during pregnancy, it can pose serious risks to the baby. Maternal diabetes disrupts the normal fetal brain development. Research says that around 8-12% of all diabetic pregnancies have been associated with malformations.6Bhandari J, Thada PK, Khattar D. Diabetic Embryopathy. [Updated 2023 Sep 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK558974/
Maternal Hyperthermia
It is a condition when the mother’s body remains too hot during pregnancy. It is also considered a risk factor for neural tube defects in the baby.
Opioids Abuse
Any type of drug abuse by a pregnant woman is detrimental to the baby. Opioids like heroin and hydrocodone may lead to neural tube defects (NTDs).
What are the Symptoms of Anencephaly?
According to the National Institute of Neurological Disorders and Stroke (NINDS), an anencephalic baby is typically blind, deaf, and doesn’t understand the surroundings.7National Institute of Neurological Disorders and Stroke. (n.d.). Anencephaly. Retrieved from https://www.ninds.nih.gov/health-information/disorders/anencephaly?search-term=Anencephaly

Here are some signs and symptoms of a baby born with anencephaly:
- Exposed areas of brain tissue (no skin or skull covering it)
- Large areas of the brain are missing
- Folding of the ears
- Lack of consciousness (awareness)
- Absence of vision
- Absence of hearing
- Inability to feel pain
- Split in the roof of the mouth (cleft palate)
- Congenital heart defects
- Reflexes may be present, but they don’t indicate awareness
Some babies may have a brain stem, allowing basic movements like breathing and responding to touch.
How to Diagnose Anencephaly?
During pregnancy, women undergo specific prenatal screening tests that help identify any birth defects present. Usually, an anomaly scan is done at 18-22 weeks of pregnancy.
Diagnostic tests for anencephaly include:
Quad Marker Screening Test
This type of blood test examines four markers in the mother: Alpha-fetoprotein (AFP), Human chorionic gonadotropin (hCG), Estriol, and Inhibin-A. Elevated AFP levels may suggest the presence of anencephaly.8Spear, B. T. (2013). Alpha-fetoprotein. Brenner’s Encyclopedia of Genetics, 89–91. https://doi.org/10.1016/b978-0-12-374984-0.00039-5
Ultrasound
Ultrasound is normally done at different intervals during pregnancy. This helps keep track of the baby’s development and assess the mother’s health status.
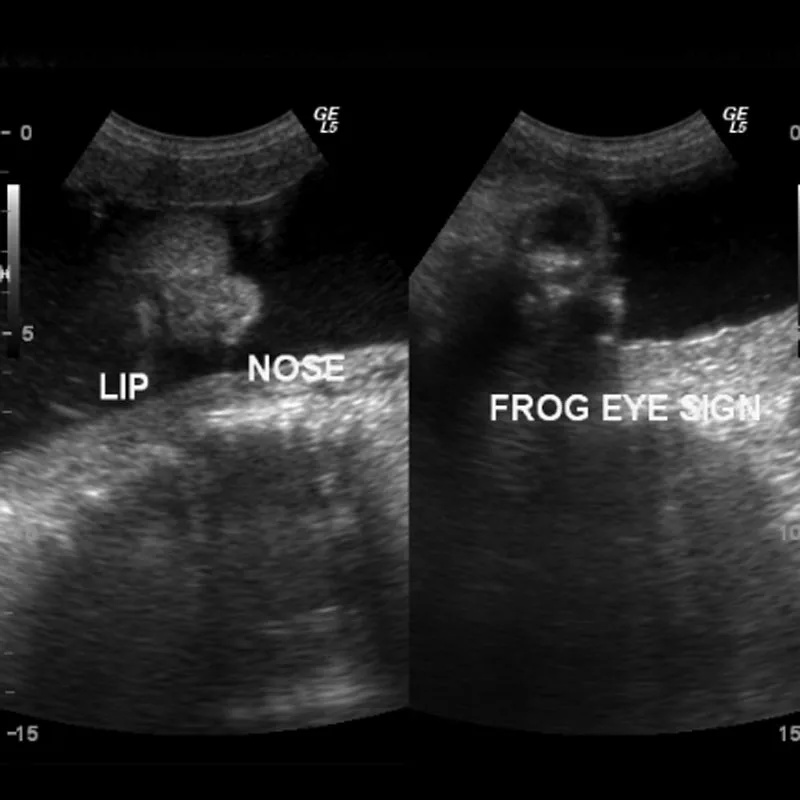
An ultrasound helps visualize the fetal skull, brain, and spine. Ultrasound is a highly accurate (nearly 100% at 14 weeks), non-invasive, and cost-effective method for detecting anencephaly. Key features include:
- Absence of Calvarium: There is no brain tissue above the orbits, with parts of the occipital bone and midbrain possibly present.
- Exencephaly: Some neural tissue may be visible at earlier stages.
- Shorter Crown-Rump Length: The fetus may have a shorter-than-expected CRL.
- Facial Appearance: The fetus may show a “frog eye” or “Mickey Mouse” appearance due to absent cranial bones and bulging orbits.
- Polyhydramnios: Excess amniotic fluid may be present due to impaired swallowing.
These features make ultrasound an effective tool for early anencephaly diagnosis.
Fetal Magnetic Resonance Imaging (MRI)
This detailed imaging test uses powerful magnets to visualize the fetus’s brain and spine more clearly. The MRI results show evident changes in the size of the ventricles.
Amniocentesis
This is usually done when an abnormality is seen in the quad-screening test. A thin needle is inserted into the amniotic sac to withdraw fluid. This fluid is then examined for high AFP and acetylcholinesterase levels, indicating a potential neural tube defect. Usually, an elevated macrophage amniotic fluid count suggests CNS defects or other neural abnormalities.9Sutherland, G. R., Brock, D. J., & Scrimgeour, J. B. (1975). Amniotic fluid macrophages and the antenatal diagnosis of anencephaly and spina bifida. Journal of Medical Genetics, 12(2), 135–137. https://doi.org/10.1136/jmg.12.2.135
Postnatal Examination
If prenatal screening tests are declined, including ultrasounds, the healthcare provider can easily diagnose anencephaly during the newborn’s physical exam after birth.
What is the Treatment of Anencephaly?
Sadly, there is no definitive cure for anencephaly. The treatment is only supportive, and all the efforts are made to keep the baby as comfortable as possible.
The doctor may refer the parents for genetic counseling to discuss risks for future pregnancies. Unfortunately, there has been no known strategy to avoid the risk of anencephaly in future pregnancies completely. However, the CDC recommends pregnant women take 400 mcg of folic acid daily to avoid the risk of anencephaly.10Centers for Disease Control and Prevention. (1991). Use of folic acid for prevention of spina bifida and other neural tube defects–1983–1991. MMWR Morb Mortal Wkly Rep, 40(30), 513–516.
What are the Complications of Anencephaly?
Anencephaly always leads to a sad outcome. When expecting a baby with anencephaly, there are common issues like too much amniotic fluid causing discomfort and an increased chance of abnormal labor.
Since the pituitary gland might be missing in the baby, there may not be a spontaneous start for labor. It can lead to a risk of the pregnancy going past the due date. In such cases, doctors might need to help start labor. Also, there’s a higher chance of unusual baby positions during delivery.
Anencephaly Vs. Microcephaly
Both conditions affect the development of the brain, but these are two different conditions with different prognoses.
Anencephaly involves the absence of a major portion of the brain and skull, resulting in a large head due to the missing skull. On the other hand, microcephaly means an abnormally small head size due to an underdeveloped brain. It causes intellectual disabilities, developmental delays, and seizures.
Anencephaly is typically fatal shortly after birth, while microcephaly survival varies. Some microcephalic babies may have a normal life expectancy.
The causes of microcephaly and anencephaly are more or less the same, i.e., genetic influences, toxic drugs, malnutrition, and infections. Their diagnosis is done through prenatal ultrasound and postnatal head circumference measurement.
While there’s no certain way to prevent anencephaly, taking adequate folic acid decreases the risk of this anomaly. On the other side, adequate nutrition, avoiding toxic drugs, and mosquito control to prevent Zika virus-related cases are some preventive strategies for microcephaly. Treatment for both conditions focuses on supportive care, but no cure exists.
Anencephaly Vs. Spina Bifida
Conclusion
To sum it up, anencephaly is a condition that warrants parents-to-be to learn more about this complication, which happens rarely during the birth period but has serious implications. The coalescence of genes, nutrition, and environmental factors also has a role, and that shows why there is a need for measures that will be anticipative. During the initial stages of pregnancy, timely appointments are helpful in “finding” any developing problems. Unfortunately, no treatment exists, so resolving the condition can be difficult. Parents can use tips from genetic counselors to get some direction.
Refrences
- 1Oumer, M., Kibret, A. A., Girma, A., Tazebew, A., & Silamsaw, M. (2021). Prevalence of anencephaly in Africa: a systematic review and meta-analysis. Scientific reports, 11(1), 23707. https://doi.org/10.1038/s41598-021-02966-w
- 2Centers for Disease Control and Prevention. (n.d.). Anencephaly. Retrieved January 30, 2024, from https://www.cdc.gov/ncbddd/birthdefects/anencephaly.html#:~:text=Some%20babies%20have%20anencephaly%20because,medicines%20she%20uses%20during%20pregnancy.
- 3Mai CT, Isenburg JL, Canfield MA, Meyer RE, Correa A, Alverson CJ, Lupo PJ, Riehle‐Colarusso T, Cho SJ, Aggarwal D, Kirby RS. National population‐based estimates for major birth defects, 2010–2014. Birth Defects Research. 2019; 111(18): 1420-1435.
- 4Kondo, A., Matsuo, T., Morota, N., Kondo, A. S., Okai, I., & Fukuda, H. (2017). Neural tube defects: Risk factors and preventive measures. Congenital anomalies, 57(5), 150–156. https://doi.org/10.1111/cga.12227
- 5Nojima, M., Kitahara, H., Yamada, Y., Nakazawa, A., Abe, M., Haga, N., & Shibasaki, J. (2016). Neurological teratogenic effects of antiepileptic drugs during pregnancy (Review). Experimental and Therapeutic Medicine, 12(5), 3628. https://doi.org/10.3892/etm.2016.3628
- 6Bhandari J, Thada PK, Khattar D. Diabetic Embryopathy. [Updated 2023 Sep 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK558974/
- 7National Institute of Neurological Disorders and Stroke. (n.d.). Anencephaly. Retrieved from https://www.ninds.nih.gov/health-information/disorders/anencephaly?search-term=Anencephaly
- 8Spear, B. T. (2013). Alpha-fetoprotein. Brenner’s Encyclopedia of Genetics, 89–91. https://doi.org/10.1016/b978-0-12-374984-0.00039-5
- 9Sutherland, G. R., Brock, D. J., & Scrimgeour, J. B. (1975). Amniotic fluid macrophages and the antenatal diagnosis of anencephaly and spina bifida. Journal of Medical Genetics, 12(2), 135–137. https://doi.org/10.1136/jmg.12.2.135
- 10Centers for Disease Control and Prevention. (1991). Use of folic acid for prevention of spina bifida and other neural tube defects–1983–1991. MMWR Morb Mortal Wkly Rep, 40(30), 513–516.





