What is Ichthyosis Vulgaris?
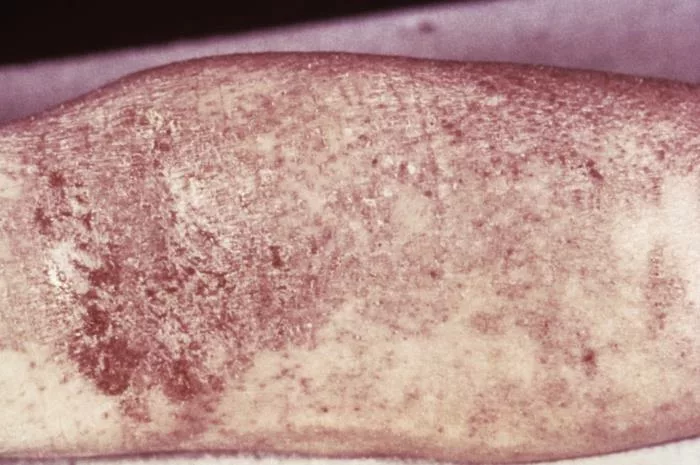
Ichthyosis is a skin disease that has many variants. The term “ichthyosis” is derived from the Greek word “ichthys,” meaning fish, highlighting the fish-like scales that appear on the skin of affected individuals. Ichthyosis vulgaris is the most common and the mildest form, making up more than 95% of cases of ichthyosis. 1 Jaffar, Huda, et al. “Ichthyosis vulgaris: an updated review.” Skin Health and Disease 3.1 (2023): e187. It is an inherited skin disorder characterized by dry, scaly skin. It affects people of all ethnicities causing discomfort and psychological distress due to the physical manifestations. Ichthyosis vulgaris typically presents in early childhood and persists throughout life.
Symptoms of Ichthyosis Vulgaris
The hallmark symptom of ichthyosis vulgaris is the presence of dry, rough, and scaly skin, often resembling fish scales. The symptoms usually manifest in infancy and are fully displayed by age 5. In some individuals, the symptoms may be mild enough to escape diagnosis, whereas some are severe. Scales in ichthyosis vulgaris usually appear on the legs, arms, abdomen, and other body parts, but the severity and extent can vary widely among affected persons. Other common symptoms include:
Xerosis
The medical term for dry skin is xerosis. Xerosis refers to abnormally dry skin or membranes. There can be partial or complete lesions on the body.
Hyperkeratosis
Hyperkeratosis refers to the increased thickness of the stratum corneum, the outer layer of the skin.2Fozia, Fozia, et al. “Novel homozygous mutations in the genes TGM1, SULT2B1, SPINK5, and FLG in four families underlying congenital ichthyosis.” Genes 12.3 (2021): 373.
Keratosis Pilaris
Keratosis pilaris is a benign skin condition characterized by dry, rough patches and small bumps, typically appearing on the upper arms, thighs, cheeks, or buttocks. However, these bumps are usually painless and non-itchy. Keratosis pilaris is commonly viewed as a prevalent form of skin anomaly.
Palmoplantar Hyper Linearity
Hyperlinearity is a thickening of the skin on the palms and soles with an increase in the number of lines in the skin.3Thyssen, J. P., E. Godoy‐Gijon, and P. M. Elias. “Ichthyosis vulgaris: the filaggrin mutation disease.” British journal of dermatology 168.6 (2013): 1155-1166.

Generalized Scaly Dermatosis
A chronic dermatosis characterized by round or oval, scaly patches primarily on the limbs and trunk.
Complications of Ichthyosis Vulgaris
Although ichthyosis vulgaris is primarily known for causing dry, scaly skin, it can also lead to several complications that require careful monitoring.
Erythroderma in Ichthyosis Vulgaris
Dermatologists observe erythema, characterized by redness and inflammation of the skin, especially in areas of increased friction or irritation. Additionally, they monitor for signs of worsening erythema over time. This is not a common feature of ichthyosis.
Pruritis
Patients with ichthyosis vulgaris usually experience pruritis, which is caused by skin dryness and scaling. This leads to discomfort and a poor quality of life. Furthermore, dermatologists address pruritis management to improve patients’ well-being.
Lichenification
Repeated scratching due to itching can cause lichenification when your skin becomes thick and leathery.
Anhidrosis
Reduction in sweat production may occur in individuals. Additionally, heat-related complications may occur.
Dehydration
Transepidermal water loss occurs due to impairment of the skin barrier. This contributes to dehydration and electrolyte imbalance, so doctors advise patients to stay hydrated.
Mineral & Protein Loss
Severe cases of ichthyosis vulgaris can cause significant mineral and protein loss through the skin. Consequently, it leads to nutritional deficiency and impaired wound healing.
Vitamin D Deficiency
Children with ichthyosis may sometimes develop rickets due to Vitamin D deficiency. Vitamin D deficiency usually occurs because of limited sun exposure, which causes discomfort in patients.
Ocular manifestations
Some individuals with ichthyosis experience ocular complications, such as dry eyes, corneal abrasion, or eyelid inflammation. Subsequently, dermatologists collaborate with ophthalmologists to address these ocular symptoms.
Hearing Problem
In rare cases, scale accumulation in the external ear can cause hearing impairment and even lead to recurrent ear infections.
Causes of Ichthyosis Vulgaris
There can be multiple reasons why an individual can get ichthyosis vulgaris. One of the following must happen.
Inherited Ichthyosis Vulgaris
In this type of ichthyosis, the individual gets genes from one or both parents. Ichthyosis vulgaris is primarily caused by mutations in the filaggrin gene (FLG) located on chromosomes.4Smith, Frances JD, et al. “Loss-of-function mutations in the gene encoding filaggrin cause ichthyosis vulgaris.” Nature Genetics 38.3 (2006): 337-342. These mutations impair the production or function of filaggrin, a protein crucial for maintaining the skin’s barrier function. The body needs filaggrin to create a healthy outermost layer of skin. Without adequate filaggrin, the skin loses moisture and becomes prone to dryness and scaling. The inheritance pattern of ichthyosis vulgaris is autosomal dominant, meaning a child only needs to inherit one copy of the mutated gene from either parent to develop the condition. However, individuals with two copies of the mutated gene (homozygous) may experience more severe symptoms.
Another cause of ichthyosis vulgaris is gene mutation in the womb. The child usually appears with the disease between 3 months and 5 years old. This type of ichthyosis often runs in the family.
Less filaggrin is the main cause of ichthyosis vulgaris. Without filaggrin, the body can not shed old, dead skin cells as it should. As a result, the skin cells build up on the skin surface, leading to scales all over the body.
Acquired Ichthyosis
It is a nonhereditary cutaneous disorder characterized by dry, rough skin on significant body parts. Microscopic studies have revealed that acquired ichthyosis has reduced or no granular layer. Moreover, it is usually associated with malignancies, autoimmune diseases, endocrine issues, metabolic and inflammatory diseases, and some medicines.5Patel, Nisha, et al. “Acquired ichthyosis.” Journal of the American Academy of Dermatology 55.4 (2006): 647-656. Some medicines that may trigger the onset of ichthyosis are:
- Cimetidine (an antacid and antihistamine used to treat ulcers and acid reflux)
- Clofazimine (a drug used to treat leprosy)
- Nicotinic acid (Vitamin B)
Pathology of Ichthyosis Vulgaris
Histologically, both ichthyosis vulgaris and acquired ichthyosis are present with laminated orthokeratosis, which is a thickening of the keratin layer with preserved keratinocyte maturation. However, the granular layer usually shows reduced thickness or is completely absent, the spinous layer maintains normal thickness, and there is an absence of any inflammatory infiltrate in the dermis.
Diagnosis of Ichthyosis Vulgaris
A comprehensive evaluation is needed to properly and correctly diagnose ichthyosis vulgaris. This includes patient history, physical examination, clinical findings, and sometimes genetic testing. Here is a detailed overview.
Clinical Examination
The clinical examination includes the following:
Skin Assessment
Dermatologists observe the skin for specific features of ichthyosis, such as fish-like scales and dry skin. They also evaluate the distribution of the lesion. The condition commonly affects the extensor surfaces of the arms, legs, and trunk, manifesting as bilateral lesions with symmetrical involvement. Observers also note hyperlinear palms and feet, follicular plugging, and other skin markings and changes.
Patient History
The age of onset, duration, and progression of symptoms play crucial roles in diagnosis. As ichthyosis vulgaris is an autosomal dominant disease, a detailed family history helps in identifying the pattern.
Laboratory Tests
The doctor may conduct the following test to confirm the diagnosis:
Skin Biopsy
Although it may not always be necessary, doctors may perform it to rule out other conditions. The biopsy typically shows hyperkeratosis and retention of keratinocytes.
Genetic Testing
Genetic testing can identify mutations in the filaggrin gene (FLG), which confirms the diagnosis of ichthyosis vulgaris and aids in genetic counseling. It is required in individuals and families suffering from ichthyosis. However, discussing the inheritance pattern can reduce the risk of transferring mutated genes to the offspring.
Treatment of Ichthyosis Vulgaris
While there is currently no cure for ichthyosis vulgaris, various treatment strategies can help manage symptoms and improve quality of life:
Emollients
The main treatment approach for hereditary and acquired ichthyosis vulgaris includes skin hydration. Emollients are moisturizing treatments applied directly to the skin to soothe and hydrate it. They cover the skin with a protective film to trap moisture. Urea-based emulsion, composed of 10% urea, natural moisturizing factors, and ceramides used twice daily, represents an effective therapeutic option.6 Benintende C, Boscaglia S, Dinotta F, Lacarrubba F, Micali G. Treatment of ichthyosis vulgaris with a urea-based emulsion: videodermatoscopy and confocal microscopy evaluation. G Ital Dermatol Venereol. 2017 Dec;152(6):555-559.
Urea has keratolytic properties, so it helps restore stratum corneum function and hydration. Moreover, it prevents excessive keratin accumulation; thus, it is used as the first line of treatment for ichthyosis.
Topical Retinoids
Prescription of retinoid creams may help reduce skin texture and reduce scaling. Topical retinoids reduce the cohesiveness of epithelial cells, stimulate mitosis and turnover, and suppress keratin synthesis.7 Haas AA, Arndt KA. Selected therapeutic applications of topical tretinoin. J Am Acad Dermatol. 1986 Oct;15(4 Pt 2):870-7.
Topical Steroid
In case of intense inflammation and itching, topical steroids can be helpful.
Keratolytic
Products containing salicylic acid can help exfoliate dead skin cells and reduce inflammation.
Differential Diagnosis
The differential diagnoses of ichthyosis vulgaris include:
- Atopic dermatitis
- Psoriasis
- Allergic and irritant contact dermatitis
- Asteatotic eczema
- Lamellar ichthyosis
- X-linked ichthyosis
- Harlequin ichthyosis
- Drug eruptions
- Sjogren Larsson syndrome
Difference between Ichthyosis Vulgaris, Atopic Dermatitis & Psoriasis
Skin diseases are very tricky to diagnose and treat. Proper insight into the patient’s history, clinical examination, and histopathology can lead to the correct diagnosis. Ichthyosis vulgaris, atopic dermatitis, and psoriasis have the following key differentiating points.
| Ichthyosis Vulgaris | Atopic Dermatitis | Psoriasis | |
| Age of Onset | Early childhood | Infancy to adulthood 8Spergel, Jonathan M., and Amy S. Paller. “Atopic dermatitis and the atopic march.” Journal of Allergy and Clinical Immunology 112.6 (2003): S118-S127. | Typically, adulthood |
| Histopathology | Reduced granular layer or absent, normal spinous layer | Epidermal hyperplasia, spongiosis, lymphocytic infiltrate | Epidermal hyperplasia, parakeratosis, Munro micro abscess9 Uribe-Herranz, Mireia, et al. “IL-1R1 signaling facilitates Munro’s microabscess formation in psoriasiform imiquimod-induced skin inflammation.” Journal of Investigative Dermatology 133.6 (2013): 1541-1549. |
| Causes | Filaggrin gene mutation | Genetic predisposition, environmental triggers | Immune dysfunction, Genetic predisposition |
| Symptoms | Dry, scaly skin; fish-like scales; hyper linear palms | Dry, itchy, inflamed skin; eczematous lesions; lichenification | Red, scaly plaques; silvery scales; nail changes |
| Treatment Options | Emollients, topical retinoids, keratolytic | Moisturizers, topical corticosteroids, calcineurin inhibitors | Topical corticosteroids, phototherapy, systemic medications |
| Key Differentiating Points | Onset in early childhood, fish-like scales, hyper linear palms | Onset can be at any age, eczematous lesions, lichenification | Typically, adult-onset, red plaques with silvery scales, nail changes |


Living with Ichthyosis Vulgaris
Living with ichthyosis can pose challenges depending on the type and severity of the disorder. Nevertheless, implementing the following self-care strategies can aid in managing the condition, enhancing overall health, and fostering a better quality of life:
Moisturizing Baths
Taking baths can increase skin moisture and facilitate the removal of scales before applying topical treatments.
Maintain a Cool Environment
Keeping the environment cool can benefit individuals with ichthyosis who struggle with heat intolerance and reduced sweating or significant itching.
Use Humidifiers
Since heating and air conditioning systems can lead to dry air, using humidifiers helps retain moisture, preventing excessive skin dryness.
Wear Loose-Fitting Clothing
Moreover, choosing loose-fitting garments made from materials like cotton is less likely to irritate the skin.
Select Gentle Laundry Detergents
Utilize laundry detergents specifically formulated for sensitive skin without excessive dyes or fragrances.
Seek Community Support
Engage with supportive communities or online support groups dedicated to ichthyosis. Additionally, some individuals may find it beneficial to consult with mental health professionals to address coping mechanisms for dealing with the challenges associated with the disorder.
Conclusion
Accurate diagnosis is crucial for implementing appropriate management strategies in ichthyosis vulgaris. It is important for healthcare professionals to provide genetic counseling for affected individuals and their families.
Refrences
- 1Jaffar, Huda, et al. “Ichthyosis vulgaris: an updated review.” Skin Health and Disease 3.1 (2023): e187.
- 2Fozia, Fozia, et al. “Novel homozygous mutations in the genes TGM1, SULT2B1, SPINK5, and FLG in four families underlying congenital ichthyosis.” Genes 12.3 (2021): 373.
- 3Thyssen, J. P., E. Godoy‐Gijon, and P. M. Elias. “Ichthyosis vulgaris: the filaggrin mutation disease.” British journal of dermatology 168.6 (2013): 1155-1166.
- 4Smith, Frances JD, et al. “Loss-of-function mutations in the gene encoding filaggrin cause ichthyosis vulgaris.” Nature Genetics 38.3 (2006): 337-342.
- 5Patel, Nisha, et al. “Acquired ichthyosis.” Journal of the American Academy of Dermatology 55.4 (2006): 647-656.
- 6Benintende C, Boscaglia S, Dinotta F, Lacarrubba F, Micali G. Treatment of ichthyosis vulgaris with a urea-based emulsion: videodermatoscopy and confocal microscopy evaluation. G Ital Dermatol Venereol. 2017 Dec;152(6):555-559.
- 7Haas AA, Arndt KA. Selected therapeutic applications of topical tretinoin. J Am Acad Dermatol. 1986 Oct;15(4 Pt 2):870-7.
- 8Spergel, Jonathan M., and Amy S. Paller. “Atopic dermatitis and the atopic march.” Journal of Allergy and Clinical Immunology 112.6 (2003): S118-S127.
- 9Uribe-Herranz, Mireia, et al. “IL-1R1 signaling facilitates Munro’s microabscess formation in psoriasiform imiquimod-induced skin inflammation.” Journal of Investigative Dermatology 133.6 (2013): 1541-1549.





