What is Ischemic Cardiomyopathy?
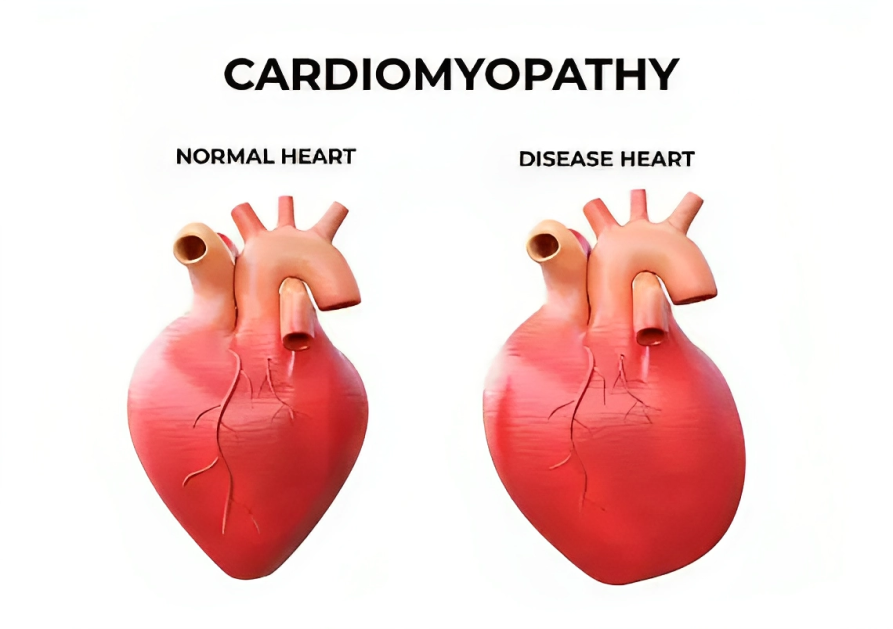
Ischemia is the compromised blood supply to the affected organ, tissue, and heart muscles. Ischemic cardiomyopathy is a clinical condition in which the ability of your heart to pump blood efficiently reduces significantly due to fibrosis of the myocardium caused by ischemia. It is one of the prime causes of heart failure in most of the countries.1Cabac-Pogorevici, I., Muk, B., Rustamova, Y., Καλογερόπουλος, Α., Tzeis, S., & Vardas, P. (2020). Ischaemic cardiomyopathy. Pathophysiological insights, diagnostic management and the roles of revascularisation and device treatment. Gaps and dilemmas in the era of advanced technology. European Journal of Heart Failure, 22(5), 789–799. https://doi.org/10.1002/ejhf.1747
Ischemic cardiomyopathy is mainly associated with coronary artery disease (CAD) and heart attack. Coronary arteries in the heart supply oxygenated blood and nutrition to your heart muscle. When coronary artery disease occurs, it causes the narrowing of the arteries, resulting in inadequate blood flow oxygen toward the muscles, causing myocardial damage.
The main function of the myocardium is to contract your heart to pump blood into the body. Initially, when oxygenated blood flow is decreased, myocardial damage is reversible. However, when ischemia persists for an extended period, it causes irreversible damage to cardiomyocytes. This irreversible damage results in heart remodeling. Remodeling is characterized by scarring and fibrosis of the myocardium, which causes conduction abnormality and decreases cardiac output and arrhythmias.2Bhandari, B. (2023, July 31). Ischemic cardiomyopathy. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK537301/#:~:text=Ischemic%20cardiomyopathy%20(ICM)%20is%20a, CAD)%20has%20to%20be%20addressed.
How common is Ischemic Cardiomyopathy?
It is the most common cardiac issue in the United States (US). It is associated with significant morbidity and mortality. According to Heart disease and statistics reports from the American Heart Association (AHA), it was stated that about 15.5 million adults had coronary artery disease.3The American Heart Association. (n.d.). Silent Ischemia and Ischemic Heart Disease. Retrieved from https://www.heart.org/en/health-topics/heart-attack/about-heart-attacks/silent-ischemia-and-ischemic-heart-disease Moreover, the overall mortality ratio from coronary artery diseases was approximately 102 deaths per 10,000 individuals. Ischemic cardiomyopathy can occur at any age. It is more prevalent in males (38%) than females (18%).4Khan, M. A., Hashim, M., Mustafa, H., Baniyas, M. Y., Suwaidi, S. K. B. M. A., AlKatheeri, R., Alblooshi, F. M. K., Almatrooshi, M. E. a. H., Alzaabi, M., Darmaki, R. S. A., & Lootah, S. N. a. H. (2020). Global Epidemiology of Ischemic Heart Disease: Results from the Global Burden of Disease Study. Cureus. https://doi.org/10.7759/cureus.9349
Pathophysiology
As previously mentioned, Coronary artery disease is one of the leading causes of ischemic cardiomyopathy. Your heart is the main organ that pumps and supplies oxygen-rich blood and nutrients to your body. Several deleterious alterations take place in ischemic cardiomyopathy. These changes mainly imbalance perfusion and contraction ratio.
Coronary artery disease results from damage to vascular endothelial cells. It usually occurs after myocardial ischemia, leading to fat accumulation (mainly low-density lipoproteins) and macrophages, causing foam cell formation. Moreover, these fat-laden macrophages (foam cells) cause fibrosis of the affected site, resulting in plaque formation. The plaques have the potential for thrombosis.
Your heart muscles are supplied by coronary vessels. When atherosclerotic plaque is formed, it causes the narrowing of the coronary vessels, resulting in inadequate supply to the cardiac muscle. When the blood supply to the heart muscle is insufficient, it causes ischemia. Initially, ischemia is reversible. However, if ischemia persists for a long period, it leads to irreversible muscle damage and fibrosis.
In ischemic cardiomyopathy, left ventricles lose their ability to function optimally. 5Cabac-Pogorevici, I., Muk, B., Rustamova, Y., Καλογερόπουλος, Α., Tzeis, S., & Vardas, P. (2020). Ischaemic cardiomyopathy. Pathophysiological insights, diagnostic management and the roles of revascularisation and device treatment. Gaps and dilemmas in the era of advanced technology. European Journal of Heart Failure, 22(5), 789–799. https://doi.org/10.1002/ejhf.1747
Ischemic vs Non-Ischemic Cardiomyopathy:
As we have discussed above, ischemic cardiomyopathy is the most common clinical condition that occurs due to compromised blood supply in the coronary arteries. It is mainly linked to coronary artery disease (CAD).
In contrast, non-ischemic cardiomyopathy is not linked to coronary artery disease and does not stem from ischemia or compromised blood supply in the coronary arteries. Instead, the major causes of non-ischemic cardiomyopathy include viral or bacterial infections (viral or bacterial myocarditis), drug reactions, and autoimmune diseases like lupus erythematosus, which can lead to lupus myocarditis.
What is Ischemic Dilated Cardiomyopathy?
Ischemic cardiomyopathy is the most common type of Dilated cardiomyopathy, which is a slow progressive disease. It is characterized by left ventricular enlargement with decreased ventricular contraction. Worldwide, it is the prime cause of heart failure. It may or may not be associated with coronary artery disease.
Causes & Risk Factors of Ischemic Cardiomyopathy
Coronary artery diseases lead to Inadequate blood supply and nutrients. When blood does not meet the metabolic demand, it results in cell death, fibrosis, and ventricular enlargement. Some other causes of cardiomyopathy are:
- Collagen vascular disease
- Coronary artery dissection
- Cardiac tumors (myxoma)
- Heart attack
- Prinzmetal angina
Risk Factors:
There can be multiple risk factors for ischemic cardiomyopathy. They can be modifiable and non-modifiable.
Modifiable Risk Factors
Modifiable risk factors are those that can be controlled and can be changed accordingly. These factors include the following:
- Diabetes mellitus
- Hypertension
- Alcohol abuse
- Drugs intoxications
- Obesity
- Hyperlipidemia
- Tobacco abuse
Non-Modifiable Risk Factors
Non-modifiable risk factors are those that can not be changed.6Cabac-Pogorevici, I., Muk, B., Rustamova, Y., Καλογερόπουλος, Α., Tzeis, S., & Vardas, P. (2020). Ischaemic cardiomyopathy. Pathophysiological insights, diagnostic management and the roles of revascularisation and device treatment. Gaps and dilemmas in the era of advanced technology. European Journal of Heart Failure, 22(5), 789–799. https://doi.org/10.1002/ejhf.1747 These are:
- Positive family history
- Aging
- Gender
Symptoms of Ischemic Cardiomyopathy
There are multiple symptoms of ischemic cardiomyopathy, which vary from person to person. Signs and symptoms of this disease depend on the severity of the disease. Some people stay asymptomatic, while others show mild to moderate symptoms. However, a few people may present with symptoms of heart failure. The most common symptoms of ischemic cardiomyopathy include the following:
- Angina (chest pain)
- Palpitations
- Dyspnea (difficult breathing) on exertion
- Orthopnea (shortness of breath during lying position and subside on standing)
- Exercise intolerance
- Easy fatigability
- Arrhythmias (irregular rhythm of the heart)
- Dizziness
- Syncope (fainting)
- Edema (swelling of legs and feet)
- Heart failure
- Weight gain
How to Diagnose Ischemic Cardiomyopathy?
A comprehensive examination, including history, physical examination, laboratory investigations, and imaging modalities, is required to diagnose ischemic cardiomyopathy.
History:
History is the most efficient way to reach a diagnosis. Your doctor asks some questions about your disease. These are:
- Biodata ( Name, age, weight )
- Presenting complaints?
- Do you have chest pain? If yes, what is the chest pain’s area, onset, and duration?
- Have you had this before?
- Do you have palpitations?
- How much can you walk?
- Do you have breathing difficulty?
- Do you have swelling in your legs?
- Do you have any other medical illness?
- Are you taking some medication for this or not? If yes, then which medication?
- Is there any person in your family who has this disease?
- Do you have hypertension?
- Social history
- Do you use tobacco?
- Do you smoke? If yes, then ask how many packs per day.
- Do you drink alcohol?
Physical Examination:
After a detailed history, your doctor will do a complete physical examination to make a diagnosis. He will perform a physical examination in the following steps:
Inspection
On inspection, your doctor will check your chest for chest abnormalities, respiratory rate, scar marks, signs of anemia or hepatitis, heart rate, and signs of hypoxia, like cyanosis, jugular vein distension, and clubbing of the nails to rule out different causes of ischemic cardiomyopathy.
Palpation
After inspection, your doctor will do palpation to check the temperature, tenderness, apex beat, pulses (for radio femoral delay and other abnormalities), lymph nodes for lymphadenopathy, pitting or non-pitting edema, ascites, and hepatojugular reflux (distention of internal jugular veins on applying pressure over the liver).
Auscultation
It is the main step in a physical examination in which your doctor will auscultate your chest to check the heart sound. In auscultation, your doctor will check for:
- Apex beat
- Murmur
- Aortic bruit
- Auscultate the back of the chest to check for basal crepitations
- Check blood pressure
- Check for S3 gallop
Laboratory Investigations:
The laboratory workup for patients suspected of ischemic cardiomyopathy is as follows:
- Complete blood count (CBC) to check for anemia
- White blood cell count to check infection rate
- Erythrocyte sedimentation (ESR) to check for infection
- Thyroid function tests to check the status of the thyroid
- B-type natriuretic peptide assay
Brain Natriuretic Peptide Test (BNP)
It is an excellent biomarker of the heart. BNP is synthesized inside the verticle and is released when there is damage to the myocardium.
Electrocardiography (ECG)
It provides the electrical activity of the heart. ECG report describes the rate, rhythm, past and current ischemic events, conduction, and chamber enlargement.
Imaging Modalities:
Imaging modalities can confirm your diagnosis and visualize your heart structure. The main motive for using these modalities in clinical practice is to check functional and perfusional abnormalities. These tests also vary in sensitivity, specificity, and handler techniques. The most common imaging investigations are:
Chest X-ray
Chest X-ray is the most basic radiological investigation readily available in every clinical setup. It indicates cardiomegaly (enlargement of the heart) and lung opacities.
Echocardiography
Echocardiography is the most common radiological investigation, specifically for the heart. It shows the internal structure of the heart and cardiac output as well. However, in ischemic cardiomyopathy, echocardiography shows an enlarged left ventricle with a reduced ejection fraction of less than 40%. There are various ways to perform echocardiography.
Moreover, doctors perform stress echocardiography after injecting dobutamine to check pathological responses against stress.

There are two steps to check your heart in echocardiography. In the First step, a low dose of dobutamine is given. In the second step, a high dose of dobutamine is injected, and echocardiography is performed afterward.
Echocardiography reports show an increased heart contractility followed by a low dose of dobutamine administration and deterioration of myocardial contractility after high-dose administration.
Computer Tomography Scan
This single-photon emission computed tomography scan checks the myocardial uptake of radioactive material. These radioactive elements are thallium 201 and technetium 99. It gives an estimation of stress-induced ischemia, scaring, and cardiac functioning.7Subramanyam, P. (2020). Myocardial viability evaluation using a novel 99mTc SestaMIBI and low dose Dobutamine infusion technique in high risk Ischemic cardiomyopathy patients – A pilot study. The Anatolian Journal of Cardiology. https://doi.org/10.14744/anatoljcardiol.2020.99148
Positron Emission Tomography Scan (PET Scan)
This scan helps to determine the metabolic function of the heart. A PET scan uses two protocols to confirm the viability of the myocardium. First, myocardial perfusion is assessed, and second, myocardial glucose is assessed.
Magnetic Resonance Imaging
The cardiovascular magnetic imaging technique is becoming popular because it provides a detailed heart structure, including size, shape, thickness, and cardiac output. It can also help assess myocardial viability after dobutamine administration. Comparatively, this imaging modality is superior to others.
Coronary Angiography
This imaging modality allows direct visualization of coronary vessels, blood flow toward the heart, and obstruction. It is a diagnostic as well as a therapeutic procedure.8Facc, V. Q. N. M. (n.d.). Dilated Cardiomyopathy Treatment & Management: approach considerations, blood pressure control, ACE inhibitors and ARBs. https://emedicine.medscape.com/article/152696-treatment#d25
When to consult with your Doctor?
Immediately Consult with your doctor and book an appointment when you feel persistent chest pain not settling even after rest, especially when you have breathing difficulty.
How to treat Ischemic Cardiomyopathy?
Different medical and surgical treatment options are available for ischemic cardiomyopathy. However, the most definitive treatment option is revascularization therapy. Moreover, some lifestyle modifications also help to overcome ischemic cardiomyopathy. The medical interventions for ischemic cardiomyopathy are:
Beta-blockers:
Beta-blockers are renowned drugs that lower the heart rate by acting on the B1 receptor in the heart and kidney. The main action of this receptor is to increase the heart rate by increasing muscular contraction. In stress, epinephrine is released into the blood and targets the B1 receptor, increasing heart contraction.
Beta-blockers like labetalol, atenolol, and propranolol antagonize the effect of epinephrine on the B1 receptor, leading to a decrease in heart rate and oxygen consumption. This effect prevents ischemia in ischemic cardiomyopathy. 9Pearle DL. Pharmacologic management of ischemic heart disease with beta-blockers and calcium channel blockers. Am Heart J. 1990 Sep;120(3):739-42; discussion 743-5. doi: 10.1016/0002-8703(90)90046-z. PMID: 1975155.
Some beta-blockers specifically act on B1 receptors, called selective B1 blockers. Selective beta-blockers are used in heart failure. However, selective B1 blockers are contraindicated in patients with decompensated heart failure.
Angiotensin-converting enzyme (ACE) inhibitors:
This class of drug is primarily used to treat hypertensive crises and heart failure. ACE inhibitors inhibit the activity of the angiotensin convertase enzyme, which is involved in the production of angiotensin ( a potent vasoconstrictive agent). This enzyme has a dual mechanism of action. It decreases heart rate by decreasing angiotensin concentration in the blood. Also, it decreases the glomerular filtration rate (GFR) of the kidney by inhibiting the contraction of efferent arterioles (driving blood toward the kidney). This way, they help with ischemic cardiomyopathy.
ACE inhibitors also inhibit the inactivation of bradykinin (a potent vasodilator), which causes cough and edema in ischemic cardiomyopathy. Therefore, proper monitoring is required while using ACE inhibitors as a therapy due to their awful side effects.
Side effects of ACE inhibitors:
The side effects encountered by using ACE inhibitors are :
- Edema
- Coughing
- Hyperkalemia (increase in potassium level)
- Fatigue
- Headache
- Kidney problems
Lipid-lowering drug (statins):
Hypercholesterolemia is the most common cause of atherosclerosis that results in ischemia. Statins are the drugs that lower the level of cholesterol in your blood. Statin inhibits the activity of Hex-Methylglutaryl-COA (HMG-COA), which contributes to the production of mevalonate ( precursor of cholesterol). This drug significantly decreases the mortality rate in patients diagnosed with coronary artery disease.
Aspirin:
A daily low dose of aspirin, depending on the weight of the patient, is advised for people having cardiovascular disease or heart attack. The use of this drug has reduced morbidity and mortality in people with coronary artery disease (CAD).
Angiotensin II receptor blockers (ARBs):
This class of drugs has the same effect as ACE inhibitors. However, it does not cause a cough. It is the drug of choice in patients reporting cough after taking ACE inhibitors.
Angiotensin receptor neprilysin inhibitors (ARNI):
This drug class comprises two types (ARB inhibitors + neprilysin inhibitors). Sacubitril/valsartan is the only drug that belongs to this family. It is used to treat cardiovascular diseases and heart failure.
Vasodilators:
Hydralazine and nitrates are one of the most commonly used life-saving drugs used to treat hypertensive crises when other medications fail to overcome hypertension.
Digoxin:
Digoxin is used to treat patients with congestive heart failure. It does not decrease mortality but helps reduce hospital stays. Digoxin prevents activation of the sodium/potassium ATPase pump found on cardiomyocytes, resulting in more calcium inside the heart. Moreover, a high level of calcium increases the contraction of the heart.
Diuretics:
Spironolactone is a potassium-sparing diuretic agent that benefits people with heart failure (NYHA classifications 3 and 4).
Ranolazine:
Ranolazine is an anti-ischemic and anti-arrhythmic drug. This drug acts by inhibiting late sodium current and calcium channels. In ischemic cardiomyopathy, this drug reduces tachycardia and other associated symptoms.
Antiarrhythmic drugs:
Amiodarone is an antiarrhythmic drug to treat ventricular and supraventricular tachycardia. Arrhythmia is the most lethal heart condition, which causes sudden death of the patient if it remains undiagnosed.
Surgical interventions:
Surgical interventions are suitable when medical treatment fails to treat the ongoing cardiovascular disease. These include the following:
Revascularization therapy:
Revascularization is a procedure to restore the perfusion of the ischemic heart. The coronary artery bypass graft is a surgical procedure that offers revascularization and reduces the overall mortality ratio by seven percent. However, the primary goal of this therapy is to restore perfusion of viable ischemic areas of the body.
Left ventricular assist devices:
Implantable left ventricular assist devices are the treatment of choice in people who are unfit for the surgery. FDA-approved left ventricular assist devices are Heart Mate1 and Heart Mate 2.
Biventricular pacing:
In this surgery, surgeons implant a defibrillator under the skin, which triggers the contraction of the left ventricle. It consists of three leads with the following positions:
- Lead one on the right atrium
- Lead two on the right ventricle
- Lead three on coronary sinus
According to research studies, people with heart failure with renal impairment are less likely to respond to this therapy.
Indications of biventricular pacing:
According to the American College of Cardiology Foundation and the American Heart Association (ACCF/AHA), the indications for biventricular pacing are:
- The left ventricular ejection fraction is 30% or less
- New York Health Association (NYHA) class 1 symptoms persist for more than 40 days, followed by myocardial infarction
- Reduced heart conduction (left ventricle bundle block)
- NYHA class 2 symptoms for more than 40 days followed by myocardial infarction with ejection fraction of 35%
Heart transplant:
The ultimate option is a heart transplant if the above-mentioned treatment options do not achieve the desirable effect.10Facc, V. Q. N. M. (n.d.). Dilated Cardiomyopathy Treatment & Management: approach considerations, blood pressure control, ACE inhibitors and ARBs. https://emedicine.medscape.com/article/152696-treatment#d25
The indications of a heart transplant are as follows:
- Chronic ischemia
- Recurrent Ventricular arrhythmia
- Decrease oxygen consumption (less than 1ml/pkg/minute
- Cardiogenic shock refractory to all possible therapies
Lifestyle modifications:
Some lifestyle changes help improve your symptoms. These are the following:
- Consult with the nutritionist and make a healthy diet plan
- Limit your salt intake as it triggers your blood pressure
- Exercise daily
- Stop smoking
- Stop having tobacco products
- Sleep properly
- Avoid stress
- Keep yourself hydrated
- Use compression stockings if you have edema
What is the prognosis of ischemic cardiomyopathy?
The prognosis of ischemic cardiomyopathy depends on the severity of the disease. The viability of cardiomyocytes is the important factor determining ischemic cardiomyopathy’s prognosis. Reversible myocardial damage after revascularization therapy has a good prognosis. In contrast, those with larger areas of irreversible myocardial damage show poor prognosis.
What are the complications of ischemic cardiomyopathy?
Cardiovascular diseases are lethal. It is necessary to diagnose them early to avoid serious complications. Ischemic cardiomyopathy can have the following complications if left untreated:
- Congestive heart failure
- Arrhythmias
- Edema
- Sudden cardiac arrest
Conclusion:
In summary, cardiomyopathy, characterized by diminished heart pumping capacity due to myocardial fibrosis, presents with symptoms that vary in severity. Initially asymptomatic, it requires a combination of medical and surgical interventions for treatment. Surgical measures are considered if medical approaches prove ineffective. In cases of treatment resistance, a heart transplant becomes a viable option.
Refrences
- 1Cabac-Pogorevici, I., Muk, B., Rustamova, Y., Καλογερόπουλος, Α., Tzeis, S., & Vardas, P. (2020). Ischaemic cardiomyopathy. Pathophysiological insights, diagnostic management and the roles of revascularisation and device treatment. Gaps and dilemmas in the era of advanced technology. European Journal of Heart Failure, 22(5), 789–799. https://doi.org/10.1002/ejhf.1747
- 2Bhandari, B. (2023, July 31). Ischemic cardiomyopathy. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK537301/#:~:text=Ischemic%20cardiomyopathy%20(ICM)%20is%20a, CAD)%20has%20to%20be%20addressed.
- 3The American Heart Association. (n.d.). Silent Ischemia and Ischemic Heart Disease. Retrieved from https://www.heart.org/en/health-topics/heart-attack/about-heart-attacks/silent-ischemia-and-ischemic-heart-disease
- 4Khan, M. A., Hashim, M., Mustafa, H., Baniyas, M. Y., Suwaidi, S. K. B. M. A., AlKatheeri, R., Alblooshi, F. M. K., Almatrooshi, M. E. a. H., Alzaabi, M., Darmaki, R. S. A., & Lootah, S. N. a. H. (2020). Global Epidemiology of Ischemic Heart Disease: Results from the Global Burden of Disease Study. Cureus. https://doi.org/10.7759/cureus.9349
- 5Cabac-Pogorevici, I., Muk, B., Rustamova, Y., Καλογερόπουλος, Α., Tzeis, S., & Vardas, P. (2020). Ischaemic cardiomyopathy. Pathophysiological insights, diagnostic management and the roles of revascularisation and device treatment. Gaps and dilemmas in the era of advanced technology. European Journal of Heart Failure, 22(5), 789–799. https://doi.org/10.1002/ejhf.1747
- 6Cabac-Pogorevici, I., Muk, B., Rustamova, Y., Καλογερόπουλος, Α., Tzeis, S., & Vardas, P. (2020). Ischaemic cardiomyopathy. Pathophysiological insights, diagnostic management and the roles of revascularisation and device treatment. Gaps and dilemmas in the era of advanced technology. European Journal of Heart Failure, 22(5), 789–799. https://doi.org/10.1002/ejhf.1747
- 7Subramanyam, P. (2020). Myocardial viability evaluation using a novel 99mTc SestaMIBI and low dose Dobutamine infusion technique in high risk Ischemic cardiomyopathy patients – A pilot study. The Anatolian Journal of Cardiology. https://doi.org/10.14744/anatoljcardiol.2020.99148
- 8Facc, V. Q. N. M. (n.d.). Dilated Cardiomyopathy Treatment & Management: approach considerations, blood pressure control, ACE inhibitors and ARBs. https://emedicine.medscape.com/article/152696-treatment#d25
- 9Pearle DL. Pharmacologic management of ischemic heart disease with beta-blockers and calcium channel blockers. Am Heart J. 1990 Sep;120(3):739-42; discussion 743-5. doi: 10.1016/0002-8703(90)90046-z. PMID: 1975155.
- 10Facc, V. Q. N. M. (n.d.). Dilated Cardiomyopathy Treatment & Management: approach considerations, blood pressure control, ACE inhibitors and ARBs. https://emedicine.medscape.com/article/152696-treatment#d25

