Kaposi’s Sarcoma (KS) is a rare cancer that affects the skin, mucous membranes, and internal organs. It arises from endothelial cells lining blood or lymphatic vessels and is characterized by abnormal blood vessel proliferation, leading to tumor formation. While KS commonly presents as skin lesions, it can also affect lymph nodes, the lungs, liver, and gastrointestinal tract.1Cesarman, E., Damania, B., Krown, S. E., Martin, J., Bower, M., & Whitby, D. (2019). Kaposi sarcoma. Nature reviews. Disease primers, 5(1), 9. https://doi.org/10.1038/s41572-019-0060-9
Pathophysiology of Kaposi Sarcoma
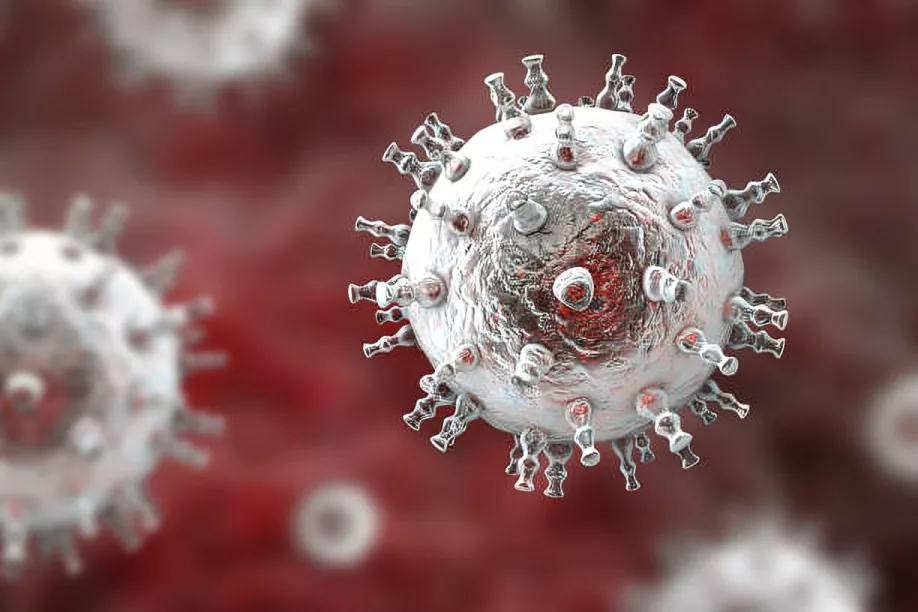
This condition affects human skin as well as mucous membranes. It is caused by human herpesvirus 8 (HHV-8) infection and HHV-8 primarily has a complex pathophysiology. Its pathophysiology includes the following:
- Transmission: The primary cause of HHV-8 transmission is exposure to the affected person’s saliva or sexual contact. It is also transmitted during organ transplantation and blood transfusions.
- Viral Entry: HHV-8 can also enter the host cells by binding viral envelope glycoproteins to host cell receptors.2Ruocco, E., Ruocco, V., Tornesello, M. L., Gambardella, A., Wolf, R., & Buonaguro, F. M. (2013). Kaposi’s sarcoma: etiology and pathogenesis, inducing factors, causal associations, and treatments: facts and controversies. Clinics in dermatology, 31(4), 413–422. https://doi.org/10.1016/j.clindermatol.2013.01.008
Phases of Kaposi Sarcoma
It has the following phases:
- Latent Phase: After the initial infection, HHV-8 enters into the latent phase, where it remains dormant in host cells, primarily in B lymphocytes and endothelial cells.
- Lytic Phase: Reactivation of HHV-8 leads to the lytic phase, which results in viral replication and produces new viral particles.
Molecular Mechanisms of Kaposi Sarcoma development
Once HHV-8 infects endothelial cells, it triggers several oncogenic pathways, including activating the mTOR signalling cascade. As a result, it leads to the growth of abnormal cells and angiogenesis. Consequently, it results in the development of Kaposi’s sarcoma. Furthermore, HHV-8 upregulates matrix metalloproteinases, facilitating tissue invasion and tumour progression. Interestingly, Kaposi sarcoma lesions are not monoclonal, meaning different nodules within the same patient arise from distinct cellular clones.
Causes of Kaposi Sarcoma
Main causes are:
- HHV-8 Infection: The primary risk factor for Kaposi sarcoma is HHV-8 infection.
- Immunosuppression: Individuals with weakened immune systems, for instance, patients with HIV/AIDS or organ transplant recipients, are typically at higher risk of developing Kaposi sarcoma.
- Genetic Predisposition: Certain populations in different regions, such as people of Mediterranean or African descent, can be at higher risk of developing KS due to genetic factors.
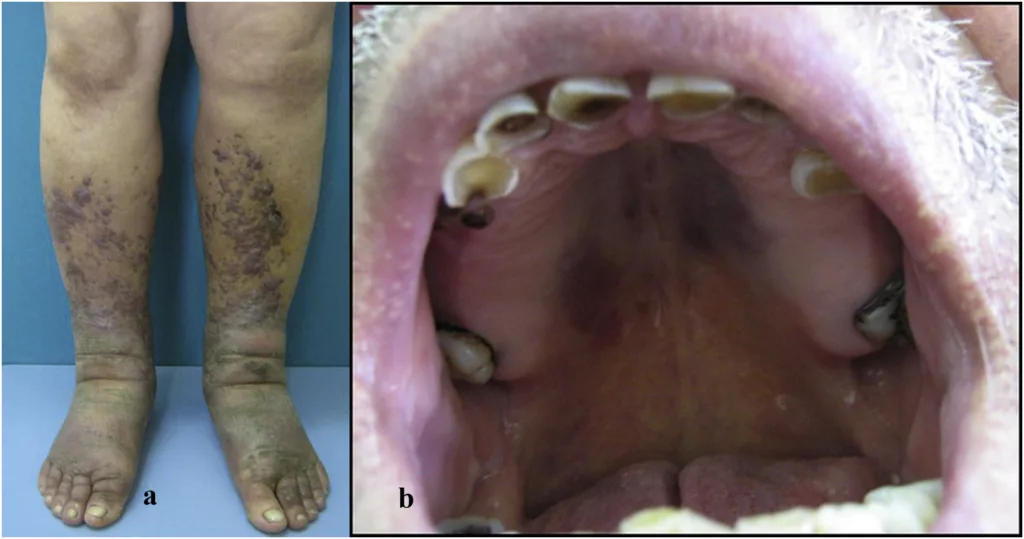
Symptoms of Kaposi Sarcoma
Patients of Kaposi Sarcoma present with:3Safai, B., Johnson, K. G., Myskowski, P. L., Koziner, B., Yang, S. Y., Cunningham-Rundles, S., Godbold, J. H., & Dupont, B. (1985). The natural history of Kaposi’s sarcoma in the acquired immunodeficiency syndrome. Annals of internal medicine, 103(5), 744–750. https://doi.org/10.7326/0003-4819-103-5-744
- Swelling in the legs, arms or face.
- Flat or raised, painless, discolored (red, purple, or brown) patches that may be smooth or bumpy. These lesions can appear in isolated areas or spread across multiple regions of the body. Over time, they may enlarge or merge.
- Difficulty in breathing.
- Abdominal pain.
- Lesions in the mouth.
- Chest pain in advanced cases..
- Lymphoedema may happen when a lesion blocks one of your lymph nodes.
- Coughing up blood because there can be lesions in the lungs.
- Blood in stool (gastric bleeding).
- Diarrhea from lesions in the digestive system.
- Constipation or vomiting from lesions blocking parts of the digestive system.
- Mouth pain when eating due to lesions in your mouth.4Polizzotto, M. N., Uldrick, T. S., Hu, D., & Yarchoan, R. (2012). Clinical Manifestations of Kaposi Sarcoma Herpesvirus Lytic Activation: Multicentric Castleman Disease (KSHV-MCD) and the KSHV Inflammatory Cytokine Syndrome. Frontiers in microbiology, 3, 73. https://doi.org/10.3389/fmicb.2012.00073
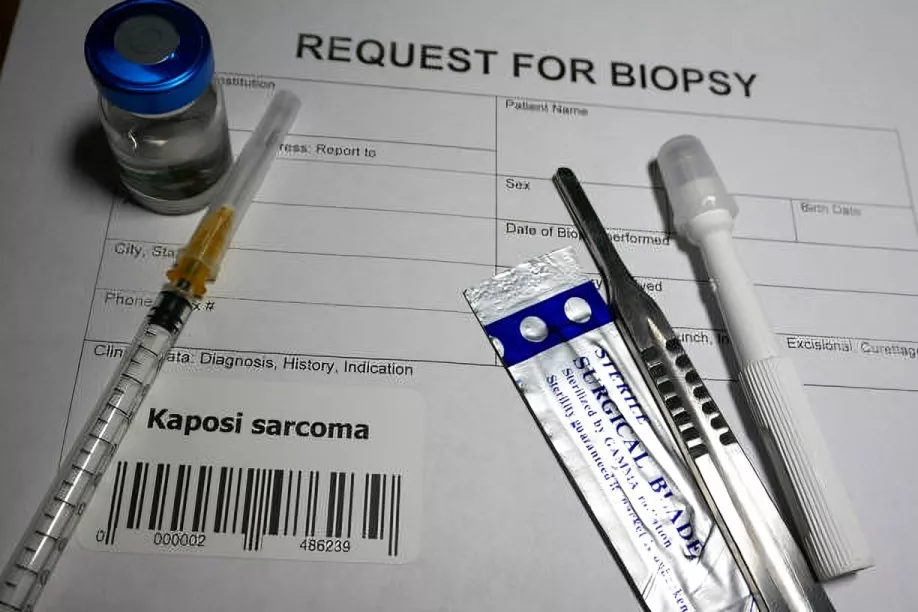
How to diagnose Kaposi Sarcoma?
This condition presents with the formation of a lesion on the body. These lesions are commonly purplish, reddish-blue, dark brown patches, plaques or nodules and are mainly present on the lower extremities. Other than the skin lesions, following methods also diagnose Kaposi Sarcoma:5Dupin, N., Jary, A., Boussouar, S., Syrykh, C., Gandjbakhche, A., Bergeret, S., & Palich, R. (2021). Current and Future Tools for Diagnosis of Kaposi’s Sarcoma. Cancers, 13(23), 5927. https://doi.org/10.3390/cancers13235927
Biopsy
A skin biopsy easily confirms the development of this condition in patients. A complete histological examination shows the presence of spindle-shaped cells. Apart from biopsy, some additional tests, such as polymerase chain reaction (PCR), can detect human herpesvirus 8 (HHV-8) DNA, while immunohistochemical staining for HHV-8 latency-associated nuclear antigen (LANA-1) further supports the diagnosis.6Hales, M., Bottles, K., Miller, T., Donegan, E., & Ljung, B. M. (1987). Diagnosis of Kaposi’s sarcoma by fine-needle aspiration biopsy. American journal of clinical pathology, 88(1), 20–25. https://doi.org/10.1093/ajcp/88.1.20
Imaging Studies
A biopsy is an important step in diagnosing this condition, but imaging is rarely helpful as it is only necessary when the patient has symptoms that suggest any visceral involvement. Routine radiographic screening is not very effective because classic Kaposi sarcoma typically follows an indolent course. Furthermore, patients with gastrointestinal symptoms may benefit from endoscopy procedures.
What are the differentials of Kaposi Sarcoma?
Classic Kaposi Sarcoma lesions sometimes also resemble other skin conditions involving vascular problems, particularly in the case of older adults since they are more vulnerable to peripheral vascular disease. A few different conditions that can mimic Kaposi Sarcoma include:7Blumenfeld, W., Egbert, B. M., & Sagebiel, R. W. (1985). Differential diagnosis of Kaposi’s sarcoma. Archives of pathology & laboratory medicine, 109(2), 123–127
Bacillary Angiomatosis:
It is a bacterial infection that is typically caused by the Bartonella species. Some red to purple papules in this disease appear initially, which may also grow in more prominent, friable nodules. A person having bacillary angiomatosis can experience specific symptoms, such as fever, fatigue, and loss of appetite. The intake of antibiotics can treat the disease.
Angiosarcoma:
Another disease that mimics Kaposi Sarcoma in terms of skin lesions is Angiosarcoma, as it also presents as skin plaques that sometimes look like bruises. That is why it becomes difficult to distinguish between both.
Benign Vascular Lesions:
Some conditions, such as the development of Benign vascular lesions, may also have specific overlapping symptoms of Kaposi sarcoma, such as hemangiomas.
Infectious Causes:
Skin infections from Sporothrix Schenckii (sporotrichosis) or Mycobacterium Marinum can sometimes resemble the skin lesions in nodular Kaposi sarcoma.
Stages of Kaposi Sarcoma
Contrary to the AIDS-related Kaposi sarcoma, classic Kaposi sarcoma has no universally accepted staging system. The American Joint Committee on Cancer (AJCC) tumour, node, metastasis (TNM) system does not apply to Kaposi sarcoma. However, researchers have proposed a classification system based on Kaposi’s sarcoma distribution and progress patterns. These stages are as follows:
- Stage I (Maculonodular Stage): It includes small macules and nodules primarily localised to the lower extremities.
- Stage II (Infiltrative Stage): Particular plaques primarily involving the lower extremities, occasionally with nodules.
- Stage III (Florid Stage): Multiple angiomatous plaques and nodules with ulceration affecting the lower extremities.
- Stage IV (Disseminated Stage): Angiomatous nodules and plaques extending beyond the lower extremities.8Mitsuyasu R. T. (1987). Clinical variants and staging of Kaposi’s sarcoma. Seminars in oncology, 14(2 Suppl 3), 13–18.
The first three stages have further divisions depending upon the progression of the condition:
- Slow Progression- Group A – During the progression stage, if the lesions remain stable over three months, the KS is in Group A.
- Rapid Progression- Group B – If the rate of plaques/nodules or the area of involvement increases over three months, it is categorized in Group B.
These categorizations are limited to the first three stages, and all cases at the fourth stage are in rapid progression. However, these stages have specific clinical implications:
Clinical Implications of Staging:
- Kaposi’s sarcoma patients during the I and II stages show a slower progression along with several complications and minimal visceral involvement.
- Kaposi’s sarcoma patients during the III and IV stages experience aggressive progress in the disease along with an increase in the rate of gastrointestinal or visceral involvement and functional impairment.
These staging and categorizations are not universally adopted due to their subjective classification although they offer a deeper understanding and provide a framework for assessing the intensity of the disease.
Alternative Staging Considerations:
Recent research suggests that identifying treatment strategies can be clinically relevant to the presence or absence of immunosuppression. During an extensive study of examining 600 KS patients, the researchers could not diagnose any significant difference in clinical, virologic, or immunologic characteristics between classic, endemic, or epidemic Kaposi sarcoma. However, this is not the final say in the matter, and more research in this area is explicitly required to determine and enhance the staging criteria for this disease.
What is the treatment of Kaposi Sarcoma?
Since the progress rate of this condition varies among patients, it is difficult to assess and determine the most effective treatment method and medications. Treatment generally depends on the extent of disease in the patient. It also strongly depends on the immune functioning of the patient. For this reason, there is no final or definitive treatment strategy for AIDS-related Kaposi sarcoma (KS-AIDS) because it is difficult to control the disease development while also ensuring that the immune system stays strong.
In the most ideal cases, it is suggested that the treatment should be mainly focused on restoring the immune function while targeting the malignancy. However, it’s still a considerable challenge to treat the children with this condition who are also affected by HIV.
General Treatment Approach:
Key considerations for the treatment include:
- Patients with limited, asymptomatic Kaposi sarcoma lesions are not immediately treated; they are generally monitored.
- Initiating antiretroviral therapy is the initial concern for tumor regression in patients who have developed AIDS-related Kaposi sarcoma.
- In the case of localized nodular Kaposi sarcoma, doctors usually recommend surgical excision, radiotherapy, or intralesional chemotherapy with low-dose vinblastine in an outpatient setting.
- The choice of treatment and therapy varies in each patient, depending on the severity of the disease as well as the immune system of the patient.
Other options to look for treatment are:
Radiotherapy:
For localized nodular Kaposi sarcoma, radiotherapy is the most suggested treatment option. However, physicians use it for palliative care instead of curative treatment in case of AIDS-related Kaposi sarcoma. Some significant elements in this include:9Tsao, M. N., Sinclair, E., Assaad, D., Fialkov, J., Antonyshyn, O., & Barnes, E. (2016). Radiation therapy for the treatment of skin Kaposi sarcoma. Annals of palliative medicine, 5(4), 298–302. https://doi.org/10.21037/apm.2016.08.03
Conventional radiotherapy is the most common and highly effective for localised nodular Kaposi sarcoma.
Electron beam radiation therapy (EBRT) detects the superficial lesions as it consists of limited penetration depth in the skin.
Alternative radiotherapy helps in case of deeper or resistant Kaposi sarcoma lesions.
Technetium-99m radioisotope scans and detects Kaposi sarcoma involvement in subcutaneous and muscular tissues. It also detects the lymph nodes in your body.
Radiotherapy can effectively respond to newly developed lesions but it may not be highly effective in the case of chronic disease. However, radiotherapy can help in the control of local KS-AIDS patients.

Other approaches include:
- Argon laser photocoagulation therapy responds better in successfully treating classic Kaposi sarcoma.
- Another treatment for classic Kaposi sarcoma patients is Long-pulse neodymium-doped yttrium Aluminium garnet (Nd: YAG) laser therapy.
- Low-voltage (100 kV) photon radiation is another effective approach.
- Alternative to cutaneous Kaposi sarcoma treatment, High-dose-rate brachytherapy can also be used for patients.
Chemotherapy:
Patients who reach later stages and the disease is widespread or symptomatic are recommended for chemotherapy. It can also be used for patients who do not respond to other treatments. Each patient’s severity of the disease, Kaposi sarcoma type, and immune system varies. Consequently, the choice of chemotherapy varies among them. Moreover, the choice of chemotherapy also depends on the availability of the resources in the hospital.10Freeman, E. E., McCann, N. C., Semeere, A., Reddy, K. P., Laker-Oketta, M., Byakwaga, H., Pei, P. P., Hajny Fernandez, M. E., Kiprono, S., Busakhala, N., Martin, J. N., Maurer, T., Bassett, I. V., Freedberg, K. A., & Hyle, E. P. (2022). Evaluation of four chemotherapy regimens for treatment of advanced AIDS-associated Kaposi sarcoma in Kenya: a cost-effectiveness analysis. The Lancet. Global health, 10(8), e1179–e1188. https://doi.org/10.1016/S2214-109X(22)00242-X
Vinblastine Therapy
For classic Kaposi sarcoma, the treatment plan is systemic vinblastine, at doses of 4–10 mg per week. In some cases, specifically AIDS-related Kaposi sarcoma, a single intralesional injection of 0.1 mg helps to treat the localized lesions.11Boudreaux, A. A., Smith, L. L., Cosby, C. D., Bason, M. M., Tappero, J. W., & Berger, T. G. (1993). Intralesional vinblastine for cutaneous Kaposi’s sarcoma associated with acquired immunodeficiency syndrome. A clinical trial to evaluate efficacy and discomfort associated with infection. Journal of the American Academy of Dermatology, 28(1), 61–65. https://doi.org/10.1016/0190-9622(93)70010-q
Topical Therapy
The topical therapy may also work for classic Kaposi Sarcoma. Doctors prescribe topical imiquimod 5% cream, which should be applied three times each week for at least 24 weeks.12Htet, K. Z., Waul, M. A., & Leslie, K. S. (2022). Topical treatments for Kaposi sarcoma: A systematic review. Skin health and disease, 2(2), e107. https://doi.org/10.1002/ski2.107
Chemotherapy for AIDS-Related Kaposi Sarcoma (KS-AIDS)
For KS-AIDS, Physicians typically recommend Antiretroviral therapy (HAART). At times, the local Kaposi sarcoma therapies go hand in hand with HAART. In some patients, Interferon alfa is effective in the treatment, especially in patients at early stages or those with CD4 counts above 200 cells/µL.
Managing Kaposi Sarcoma in Immunosuppressed Patients
Some patients develop this condition while they are dealing with immunosuppressive therapy (iatrogenic KS). In such cases, the experts must adjust or discontinue immunosuppression to treat the patient effectively.
The disease can be partially or wholly treated if the experts discontinue the immunosuppressive medications, particularly corticosteroids and cytotoxic drugs.
While initiating specific treatment for iatrogenic Kaposi sarcoma, it is better to stop the immunosuppressive therapy.
Conclusion
This disease is classified as one of the forms of cancer that affects human skin and mucous membranes. Medications and treatment are helpful in treating this disease. Radiotherapy, chemotherapy, and other local therapies are also helpful in preventing the spread of the disease. The selection of treatment methods and medication is based on the type of Kaposi sarcoma, the status of the patient’s immune system, and the facilities provided in the region. Significantly, people should get vaccinated, avoid alcohol, quit smoking, and acquire a healthy lifestyle to prevent diseases like Kaposi sarcoma. It is essential to visit a doctor if any one of you is experiencing symptoms or signs like skin lesions so that the treatment can begin as soon as possible.
Refrences
- 1Cesarman, E., Damania, B., Krown, S. E., Martin, J., Bower, M., & Whitby, D. (2019). Kaposi sarcoma. Nature reviews. Disease primers, 5(1), 9. https://doi.org/10.1038/s41572-019-0060-9
- 2Ruocco, E., Ruocco, V., Tornesello, M. L., Gambardella, A., Wolf, R., & Buonaguro, F. M. (2013). Kaposi’s sarcoma: etiology and pathogenesis, inducing factors, causal associations, and treatments: facts and controversies. Clinics in dermatology, 31(4), 413–422. https://doi.org/10.1016/j.clindermatol.2013.01.008
- 3Safai, B., Johnson, K. G., Myskowski, P. L., Koziner, B., Yang, S. Y., Cunningham-Rundles, S., Godbold, J. H., & Dupont, B. (1985). The natural history of Kaposi’s sarcoma in the acquired immunodeficiency syndrome. Annals of internal medicine, 103(5), 744–750. https://doi.org/10.7326/0003-4819-103-5-744
- 4Polizzotto, M. N., Uldrick, T. S., Hu, D., & Yarchoan, R. (2012). Clinical Manifestations of Kaposi Sarcoma Herpesvirus Lytic Activation: Multicentric Castleman Disease (KSHV-MCD) and the KSHV Inflammatory Cytokine Syndrome. Frontiers in microbiology, 3, 73. https://doi.org/10.3389/fmicb.2012.00073
- 5Dupin, N., Jary, A., Boussouar, S., Syrykh, C., Gandjbakhche, A., Bergeret, S., & Palich, R. (2021). Current and Future Tools for Diagnosis of Kaposi’s Sarcoma. Cancers, 13(23), 5927. https://doi.org/10.3390/cancers13235927
- 6Hales, M., Bottles, K., Miller, T., Donegan, E., & Ljung, B. M. (1987). Diagnosis of Kaposi’s sarcoma by fine-needle aspiration biopsy. American journal of clinical pathology, 88(1), 20–25. https://doi.org/10.1093/ajcp/88.1.20
- 7Blumenfeld, W., Egbert, B. M., & Sagebiel, R. W. (1985). Differential diagnosis of Kaposi’s sarcoma. Archives of pathology & laboratory medicine, 109(2), 123–127
- 8Mitsuyasu R. T. (1987). Clinical variants and staging of Kaposi’s sarcoma. Seminars in oncology, 14(2 Suppl 3), 13–18.
- 9Tsao, M. N., Sinclair, E., Assaad, D., Fialkov, J., Antonyshyn, O., & Barnes, E. (2016). Radiation therapy for the treatment of skin Kaposi sarcoma. Annals of palliative medicine, 5(4), 298–302. https://doi.org/10.21037/apm.2016.08.03
- 10Freeman, E. E., McCann, N. C., Semeere, A., Reddy, K. P., Laker-Oketta, M., Byakwaga, H., Pei, P. P., Hajny Fernandez, M. E., Kiprono, S., Busakhala, N., Martin, J. N., Maurer, T., Bassett, I. V., Freedberg, K. A., & Hyle, E. P. (2022). Evaluation of four chemotherapy regimens for treatment of advanced AIDS-associated Kaposi sarcoma in Kenya: a cost-effectiveness analysis. The Lancet. Global health, 10(8), e1179–e1188. https://doi.org/10.1016/S2214-109X(22)00242-X
- 11Boudreaux, A. A., Smith, L. L., Cosby, C. D., Bason, M. M., Tappero, J. W., & Berger, T. G. (1993). Intralesional vinblastine for cutaneous Kaposi’s sarcoma associated with acquired immunodeficiency syndrome. A clinical trial to evaluate efficacy and discomfort associated with infection. Journal of the American Academy of Dermatology, 28(1), 61–65. https://doi.org/10.1016/0190-9622(93)70010-q
- 12Htet, K. Z., Waul, M. A., & Leslie, K. S. (2022). Topical treatments for Kaposi sarcoma: A systematic review. Skin health and disease, 2(2), e107. https://doi.org/10.1002/ski2.107