What is Laparoscopic Cholecystectomy?
Laparoscopic cholecystectomy is the most commonly performed minimally invasive surgical procedure across the world which involves removal of the diseased gallbladder using laparoscopic technique. In this procedure, a laparoscope (a thin tube with a camera) is inserted to guide the surgeon in removing the gallbladder. Laparoscopic cholecystectomy was first invented in 1985. It is a common and effective method for treating gallbladder issues like gallstones or inflammation.1Hassler, K. R. (2023, January 23). Laparoscopic cholecystectomy. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK448145/
Prevalence of Laparoscopic Cholecystectomy
Cholelithiasis (gallstones) is the most prevalent disease in the United States of America (USA), affecting over 20-25 million people. Laparoscopic cholecystectomy is now the most dominant procedure to remove gallstones; in the USA and Europe, 98% of cholecystectomy is performed by laparoscopy. The overall frequency of laparoscopic cholecystectomy is higher than open cholecystectomy.2Sherwinter, D. A., MD. (n.d.). Laparoscopic cholecystectomy technique: Approach considerations, Conventional laparoscopic cholecystectomy, alternative minimally Invasive approaches. https://emedicine.medscape.com/article/1582292-technique#c3?form=fpf
What is Gallbladder, and how does it work?
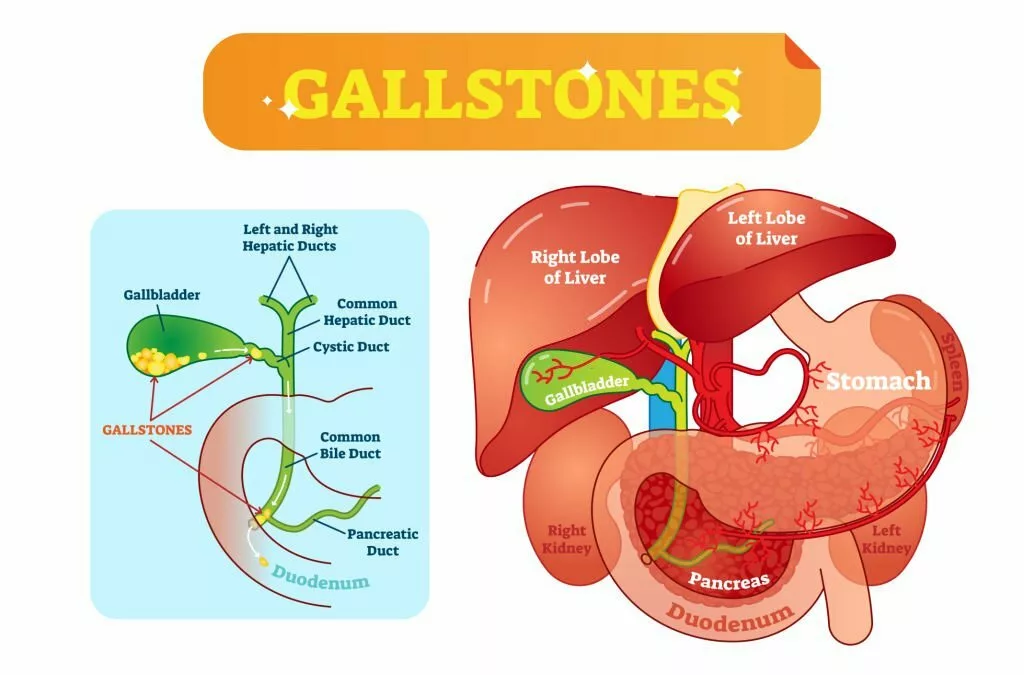
The gallbladder is a small pear-shaped organ (10 cm in size and 2-5 cm in diameter) located on the inferior aspect of the liver bed (segments 4 and 5) in the upper abdominal quadrant. Your liver produces bile used for lipolysis (breakdown of lipids). This bile is stored in the gallbladder. The average capacity of the gallbladder to hold fluid (bile) is about 50 cc, but it can have 200-300 ml in pathological conditions. When you eat food, your gallbladder contracts and drives the bile into the bile duct. Bile moves smoothly downwards From the bile duct and enters the second part of the duodenum.
Anatomically, the gallbladder is divided into four parts: neck, body, infundibulum, and fundus. The biliary duct system of the gallbladder shows variations. Cystic duct arises from the common bile duct and is inserted into the neck of the gallbladder. There is an outpouching in the neck of the gallbladder called the Hartman pouch. This pouch becomes dilated when there is inflammation of the gallbladder or a stone in the gallbladder. A large Hartman pouch can pressure the cystic duct, obstructing bile flow. The cystic artery, the branch of the right hepatic artery, supplies the gallbladder.
Calot’s Triangle:
This triangle is also called the triangle of safety or cystohepatic triangle. It has surgical importance due to its contents, including cystic artery, right hepatic artery, cystic lymph nodes (Lund’s node), and connective tissue. It should be identified during surgery, and its contents should be preserved. The anatomy of the calot’s triangle includes the common hepatic duct medially, cystic duct laterally, and liver superiorly.
Indications for Laparoscopic Cholecystectomy
The indication of laparoscopic cholecystectomy is the same as for open cholecystectomy. However, laparoscopic cholecystectomy is the most favored procedure nowadays. The indications of cholecystectomy are:
Acute Cholecystitis (Inflammation of the Gallbladder):
Acute cholecystitis is characterized by inflammation of the gallbladder with epigastric tenderness. Early diagnosis (within 72 hours) and treatment is necessary in case of acute cholecystitis. Because after 72 hours, multiple adhesions are formed due to inflammatory changes that make surgery difficult. If the patient is present after three days of onset of symptoms, then the interval (after 4-6 weeks) laparoscopic cholecystectomy is performed.
Mucocele of the Gallbladder:
Persistent blockage of the cystic for a long period results in the formation of the mucocele. The treatment of choice for mucocele of the gallbladder is laparoscopic cholecystectomy.
Empyema of the Gallbladder:
It is a very serious condition that requires early diagnosis and prompt management. Because infection of the gallbladder can spread into the bloodstream, causing multiple organ failure if it remains undiagnosed.
Biliary Colic:
Biliary colic is characterized by pain in the epigastrium. The ultrasonography findings show a stone in the common bile duct, which may require laparoscopic cholecystectomy.
Biliary Dyskinesia:
It is a pathological condition in which patients present with biliary colic, but on ultrasound report, there is no stone in the duct. In this case, a cholecystokinin diisopropyl iminodiacetic acid (CCK-DISIDA) is preferred to check the gallbladder’s ejection fraction. If the ejection fraction of the gallbladder is lower than 35% percent in 20 minutes, then it is considered abnormal, which is also an absolute indication of laparoscopic cholecystectomy.
Asymptomatic Gallstones:
In this condition, your ultrasonographic report shows stones, but you do not have symptoms. Cholecystectomy is not advised in patients having gallstones but is asymptomatic with no comorbidities. But if comorbidities are present, then prophylactic laparoscopic cholecystectomy can be performed. Indications of prophylactic laparoscopic cholecystectomy are:
- Obliteration of cystic duct
- Trauma to the gallbladder
- Sickle cell anemia
- Porcelain gallbladder (extensive calcification of the gallbladder wall)
- Functionless gallbladder
- Gallstone greater than 3-4 cm in diameter
- Polyp of the gallbladder
- Obesity
Gallstones Pancreatitis:
Gallstones can induce inflammation of the pancreas. If patients have gallstone-induced pancreatitis, imaging investigations are advised to rule out cholesochocholelithiasis. Imaging studies include magnetic resonance cholangiopancreatography (MRCP) and Endoscopic retrograde cholangiopancreatography (ERCP).
If there is a confirmation of acute pancreatitis, then your doctor will prefer the interval cholecystectomy (removal of the gallbladder after draining an infection).
Acalculous Cholecystitis:
It is a condition in which the flow of bile from the cystic duct is obstructed in the absence of stone. It is characterized by a triad of symptoms: high-grade fever, abdominal pain, and jaundice. In this condition, your doctor will advise a guided percutaneous cholecystostomy procedure.3Duca, S., Bãlã, O., Al-Hajjar, N., Lancu, C., Puia, I. C., Munteanu, D., & Graur, F. (2003). Laparoscopic cholecystectomy: incidents and complications. A retrospective analysis of 9542 consecutive laparoscopic operations. HPB : the official journal of the International Hepato Pancreato Biliary Association, 5(3), 152–158. https://doi.org/10.1080/13651820310015293
Contraindications for Laparoscopic Cholecystectomy
Laparoscopic cholecystectomy is contraindicated for some patients. They include patients who can not tolerate general anesthesia and have obstructive pulmonary disease, left heart failure, bleeding disorder, and liver failure.
In recent times, gallbladder cancer has been a contraindication of laparoscopic cholecystectomy. However, a modified radical laparoscopic cholecystectomy shows better results than an open cholecystectomy. During surgery, if there is a cancerous gallbladder, your doctor will convert simple laparoscopic cholecystectomy into open cholecystectomy.
Laparoscopic cholecystectomy is also contraindicated in hemodynamically unstable patients. Other contraindications include generalized peritonitis, multiple previous surgeries, and late pregnancy.4Rappaport, W. D., Gordon, P., Warneke, J. A., Neal, D., & Hunter, G. C. (1994). Contraindications and complications of laparoscopic cholecystectomy. American family physician, 50(8), 1707–1714.
Procedure of Laparoscopic Cholecystectomy
After a complete examination, your doctor tells you about the disease and its treatment. He will make a decision about surgery after discussing all the details with you. In case of symptomatic gallstones, the surgeon will advise surgical removal of the gallbladder. 5Comitalo J. B. (2012). Laparoscopic cholecystectomy and newer techniques of gallbladder removal. JSLS : Journal of the Society of Laparoendoscopic Surgeons, 16(3), 406–412. https://doi.org/10.4293/108680812X13427982377184
The preparation of patients undergoing laparoscopic cholecystectomy is the same as for open cholecystectomy. Before surgery, you will follow the following protocols:
Preoperative:
Before the operation, you will stay in the surgical Ward for evaluation and observation. Your doctor will advise some laboratory tests related to your surgery. These include the following:
- Complete blood count
- White blood cell count
- Random blood sugar
- Electrocardiography
- Viral markers
- Liver functions tests
- Renal function tests
- Clotting profile
- Chest X-ray
If your hemoglobin level is low, your doctor will ask you to arrange 1-2 pints of blood. If there is an infection, your surgeon will postpone your surgery. Your doctor may perform an Interval cholecystectomy to treat your infection.
Moreover, your surgeon will send you to an anesthesiologist for anesthesia fitness and your lab’s reports. After getting anesthesia fitness, your doctor will ask you not to eat before 6-8 hours of surgery.
Early in the morning, your doctor will send you to the operation theater along with the medical staff nurse. After reaching the theater, you will wear a sterile dressing before the operation.
Anesthesia:
The surgeons perform all the surgeries under anesthesia to create a pain-free environment. Your doctor will give general anesthesia to perform a Laparoscopic cholecystectomy.
Procedure:
During the operation, you will lie in the supine position. Your doctor will expose your abdomen and sterilize the skin with chlorhexidine.
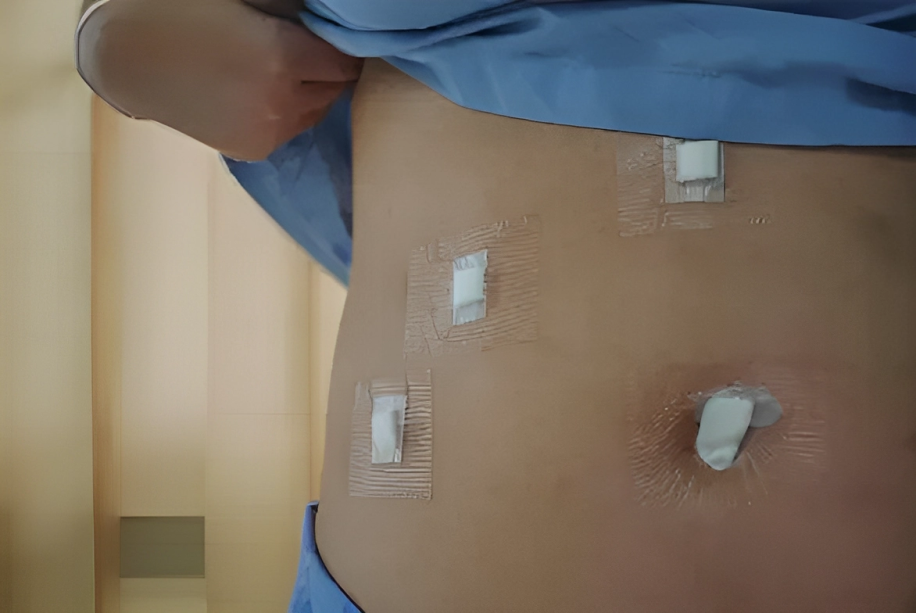
After anesthesia, your doctor will create pneumoperitoneum (air in the abdomen) with carbon dioxide. He will locate and insert the ports through your abdomen, identify the calot’s triangle, and dissect the gallbladder from the inferior aspect of the liver. Finally, he will remove the gallbladder, clean the area with normal saline, remove ports, and close your wounds.

Post-Operative Care:
After the completion of the surgery, your doctors will shift you into the intensive care unit for proper monitoring for 4-6 hours. If you are stable and can tolerate it orally, your doctor will discharge you after prescribing oral medications. Medication includes a three-day course of broad-spectrum antibiotics, painkillers, and sedatives.
After discharge, you’ll follow these instructions:
- Take your medicine regularly
- Apply antiseptic to cleanse your wound every other day
- Stay active to prevent deep venous thrombosis.
- Opt for a soft diet for your nutritional needs.
Recovery after Laparoscopic Cholecystectomy :
Laparoscopic cholecystectomy shortens the hospital stay of the patients. Patients can go home after 6-8 hours after surgery if they are vitally stable and have no complications. Patients can return to their normal work routine after 2-4 weeks of the surgery, depending upon the type of work.
Diet Plan after Laparoscopic Cholecystectomy:
Your doctor will give you a diet plan after surgery that you must follow until complete recovery. Avoid fatty and oil-cooked food, such as cream, chocolate, pizza, and butter. Additionally, eating a protein diet like fish, beef, chicken, and eggs is beneficial.
Difference between Laparoscopic & Open Cholecystectomy
Laparoscopic cholecystectomy is a less invasive procedure than open cholecystectomy. In open cholecystectomy, your doctor will give an incision on the right subcostal and paramedian incision and remove the diseased gallbladder. However, in laparoscopic cholecystectomy, usually, he will give four small incisions and insert a laparoscope through the umbilicus to see the gallbladder. Finally, he will remove the diseased gallbladder from one of the incisions.6Haribhakti, S. P., & Mistry, J. H. (2015). Techniques of laparoscopic cholecystectomy: Nomenclature and selection. Journal of minimal access surgery, 11(2), 113–118. https://doi.org/10.4103/0972-9941.140220
Cholecystectomy during Pregnancy
Usually, pregnancy is a contraindication for laparoscopic cholecystectomy due to its side effects on the Mother and fetus. However, your doctor can perform it during the second trimester with minimal operative risks.
Benefits of Laparoscopic Cholecystectomy
Laparoscopic cholecystectomy is more beneficial than open cholecystectomy due to the following reasons:
- Easy to proceed
- Less costly
- Less scarring
- Less discomforting
- Less hospital stay
- Small incision instead of a large one
- Fewer complications
- Cosmetically better outcome
Post-Laparoscopic Cholecystectomy Syndrome
Even after the surgery, post-cholecystectomy syndrome persists, marked by enduring symptoms such as right hypochondrium pain and biliary colic. It can also manifest new symptoms like:
- Intolerance of fatty food
- Indigestion
- Nausea and vomiting
- On and off abdominal pain
- Loose motion
- Jaundice
There can be multiple causes of postcholecystectomy syndrome that can be functional or organic. These include recurrent calculi in the common bile duct, stricture formation in the bile duct, biliary dyskinesia, stenosis, remnant of the cystic duct, extra biliary causes like peptic ulcer disease, reflux esophagitis, and irritable bowel syndrome. 7Zackria, R. (2022, August 29). Postcholecystectomy syndrome. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK539902/
Treatment of post-cholecystectomy syndrome includes pharmacological and surgical approaches. Pharmacotherapy includes antispasmodic medications, proton pump inhibitors, and antacids, depending on the cause. Your doctor will suggest surgery if a stone is present in the common bile duct. ERCP is suitable in such cases.
Complications of Laparoscopic Cholecystectomy
Every surgery has some minor or major complications. The complications of laparoscopic cholecystectomy are:8Radunovic, M., Lazovic, R., Popovic, N., Magdelinic, M., Bulajic, M., Radunovic, L., Vukovic, M., & Radunovic, M. (2016). Complications of Laparoscopic Cholecystectomy: Our Experience from a Retrospective Analysis. Open access Macedonian Journal of medical sciences, 4(4), 641–646. https://doi.org/10.3889/oamjms.2016.128
Intraoperative Complication:
These complications occur during the operation. These are:
- Excessive bleeding
- Injury to adjacent organs (liver, intestine, pancreas, stomach)
- Bile duct injury that causes leakage of bile in the surrounding
- Hematoma formation
- Carbon dioxide can gain entry into blood circulation, causing gas embolisms.
Postoperative Complication:
Complications that occur after the surgery are postoperative complications. These are:
- Reactionary hemorrhage (bleeding that occurs after 24-48 hours of surgery)
- Nausea and vomiting
- Postcholecystectomy syndrome
- Headache
- Deep venous thrombosis
- Chest infection
- Delayed wound healing
- Keloid scar formation
- Infection at the surgical site
Conclusion
To conclude, laparoscopic cholecystectomy is a gold-standard surgical procedure for the removal of a diseased gallbladder. This procedure has a quick recovery with the shortest hospital stay. Moreover, it is of greater cosmetic value as it doesn’t leave big scar marks on your belly. If you ever feel pain in the right upper quadrant of the abdomen, nausea, vomiting, and related symptoms, immediately consult your surgeon. In the case of cholelithiasis, you can confidently opt for laparoscopic cholecystectomy.
Refrences
- 1Hassler, K. R. (2023, January 23). Laparoscopic cholecystectomy. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK448145/
- 2Sherwinter, D. A., MD. (n.d.). Laparoscopic cholecystectomy technique: Approach considerations, Conventional laparoscopic cholecystectomy, alternative minimally Invasive approaches. https://emedicine.medscape.com/article/1582292-technique#c3?form=fpf
- 3Duca, S., Bãlã, O., Al-Hajjar, N., Lancu, C., Puia, I. C., Munteanu, D., & Graur, F. (2003). Laparoscopic cholecystectomy: incidents and complications. A retrospective analysis of 9542 consecutive laparoscopic operations. HPB : the official journal of the International Hepato Pancreato Biliary Association, 5(3), 152–158. https://doi.org/10.1080/13651820310015293
- 4Rappaport, W. D., Gordon, P., Warneke, J. A., Neal, D., & Hunter, G. C. (1994). Contraindications and complications of laparoscopic cholecystectomy. American family physician, 50(8), 1707–1714.
- 5Comitalo J. B. (2012). Laparoscopic cholecystectomy and newer techniques of gallbladder removal. JSLS : Journal of the Society of Laparoendoscopic Surgeons, 16(3), 406–412. https://doi.org/10.4293/108680812X13427982377184
- 6Haribhakti, S. P., & Mistry, J. H. (2015). Techniques of laparoscopic cholecystectomy: Nomenclature and selection. Journal of minimal access surgery, 11(2), 113–118. https://doi.org/10.4103/0972-9941.140220
- 7Zackria, R. (2022, August 29). Postcholecystectomy syndrome. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK539902/
- 8Radunovic, M., Lazovic, R., Popovic, N., Magdelinic, M., Bulajic, M., Radunovic, L., Vukovic, M., & Radunovic, M. (2016). Complications of Laparoscopic Cholecystectomy: Our Experience from a Retrospective Analysis. Open access Macedonian Journal of medical sciences, 4(4), 641–646. https://doi.org/10.3889/oamjms.2016.128

