Medullary thyroid carcinoma (MTC) is a rare type of thyroid cancer that develops from the parafollicular cells, also known as C-cells, of the thyroid gland. These specialized cells are responsible for producing the hormone calcitonin, and their abnormal growth gives rise to this form of thyroid cancer. MTC is generally considered more aggressive than other common types of thyroid cancer, such as papillary or follicular carcinoma. It accounts for about 1 to 5% of all thyroid cancer cases.1Caillé, S., Debreuve-Theresette, A., Vitellius, G., Deguelte, S., La Manna, L., & Zalzali, M. (2024). Medullary thyroid cancer: epidemiology and characteristics according to data from the Marne-Ardennes Register 1975-2018. Journal of the Endocrine Society, 8(6), bvae084.
In most cases, small tumors go unnoticed. When large, patients notice a lump in the neck and experience cervical lymphadenopathy. You may inherit the carcinoma, as a consequence of some inherited conditions like multiple endocrine neoplasia, or develop it sporadically (later in life) due to a mutation in the RET gene. Oncologists treat medullary thyroid carcinomas with a variety of strategies, including radiotherapy, chemotherapy, and surgery (thyroidectomy), depending on the stage and severity of your condition.
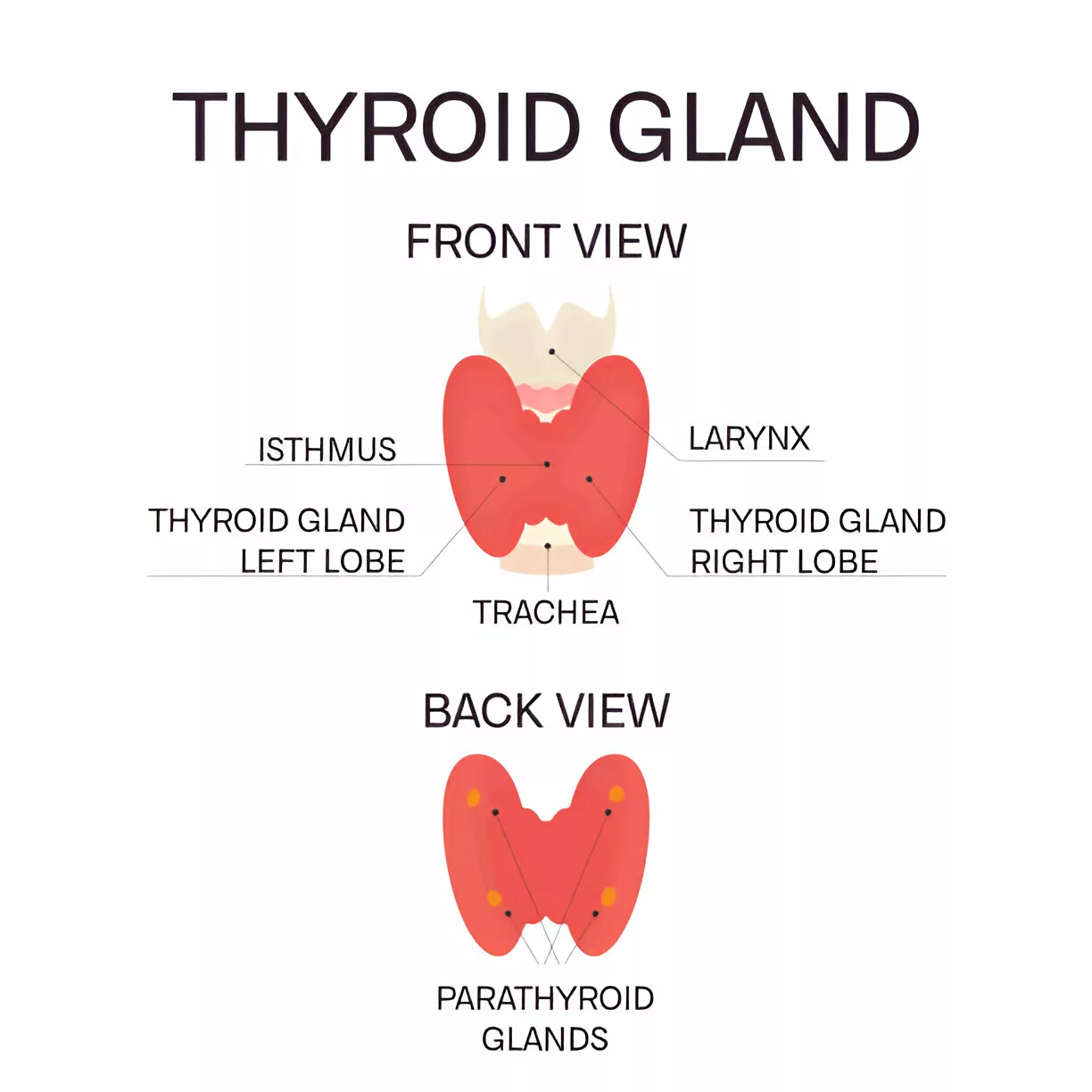
Anatomy Of The Thyroid Gland:
The thyroid is a butterfly-shaped gland present in the anterior (front) region of your neck. The endocrine gland wraps around your windpipe, i.e., trachea. Therefore, thyroid pathologies that cause overgrowth/enlargement of the gland tend to impact breathing and voice.
It consists of two lobes, which are connected by a narrow tissue band called the isthmus. The inside of the gland contains parafollicular C cells. Cancer arising in these parafollicular cells is called the medullary thyroid carcinoma (named after the C-cells, also called medullary cells; some sources refer to them as being in the “inner part” of the thyroid, but medically, the thyroid doesn’t have a defined medulla like other organs).
Medullary Thyroid Carcinoma Symptoms
Small tumors do not cause any evident symptoms. Therefore, most people don’t know about the underlying pathology. When present, patients most commonly report the following symptoms:
Neck Lump:
The vast majority of individuals report having a nodule in the neck. Radiographic images of the affected thyroid glands are in line with patients’ complaints. Around 75-90% of patients report having a neck mass and thyroid nodules.2Kushchayev, S. V., Kushchayeva, Y. S., Tella, S. H., Glushko, T., Pacak, K., & Teytelboym, O. M. (2019). Medullary thyroid carcinoma: an update on imaging. Journal of thyroid research, 2019(1), 1893047.
Swollen Lymph Nodes:
Lymph node swelling is seen in different types of cancers. In medullary thyroid carcinoma, lymph nodes in the neck swell and can be felt by the patient. About 70% of patients diagnosed with medullary carcinoma experience lymph node swelling. Thus, cervical lymphadenopathy is a common finding in MTC. This condition arises when MTC metastasizes (spreads) to the nearest lymph nodes, i.e., cervical nodes.3Fan, W., Xiao, C., & Wu, F. (2018). Analysis of risk factors for cervical lymph node metastases in patients with sporadic medullary thyroid carcinoma. Journal of International Medical Research, 46(5), 1982-1989.
Hoarseness:
Voice hoarseness can sometimes be an early symptom of medullary thyroid carcinoma, especially when the tumor grows large enough to compress or invade the recurrent laryngeal nerve, which controls the vocal cords. While hoarseness has also been documented as a presenting sign in other tumors, such as thymic carcinoma4Takeuchi, S., Yoshino, N., & Usuda, J. (2019). Hoarseness as an Initial Symptom of Thymic Carcinoma: A Case Report. Journal of Nippon Medical School, 86(6), 357-359., in the case of thyroid cancer, the proximity of the recurrent laryngeal nerve to the thyroid gland makes it particularly vulnerable. Enlarged thyroid nodules, including those seen in MTC, can affect this nerve, leading to vocal changes.
Breathing & Swallowing Issues:
Enlargement of the thyroid gland can press on the neighboring structures like the trachea and the esophagus (food pipe). This consequently causes breathing difficulties and dysphagia, respectively.
Medullary Thyroid Carcinoma Causes
MTC is a neuroendocrine neoplasm because the parafollicular cells originate from the neural crest cells. The uncontrolled division of these parafollicular cells leads to carcinoma formation. Researchers have found that MTC arises as a consequence of inherited disorders or develops sporadically due to gene mutations.
Sporadic:
The vast majority of MTC cases are sporadic. This means that they occur without a known inherited genetic mutation or family history.
As per estimates, around 75% of individuals with medullary cancer have no family history of MTC. It is believed that about half (40-50%) of these individuals fall prey to the disorder due to genetic mutations in the RET gene.
Inherited:
Around 25% of cases arise due to a condition called multiple endocrine neoplasia type 2 (MEN2). This inherited disorder leads to the formation of tumors in the endocrine glands (such as the thyroid, adrenal, and parathyroid glands). The underlying cause for this inherited disorder is a mutation in the RET proto-oncogene.5Krampitz, G. W., & Norton, J. A. (2014). RET gene mutations (genotype and phenotype) of multiple endocrine neoplasia type 2 and familial medullary thyroid carcinoma. Cancer, 120(13), 1920-1931. There are three different subtypes of MEN2:
MEN2A
Issues like hyperparathyroidism and pheochromocytoma are present in this subtype. This type is seen in 95% of inherited cases. Individuals with MEN2A disorder have a 90% chance of developing cancer. MEN2A patients have mutations in Codon 634 in exon 11, which leads to uncontrolled division of parafollicular cells.6Accardo, G., Conzo, G., Esposito, D., Gambardella, C., Mazzella, M., Castaldo, F., … & Pasquali, D. (2017). Genetics of medullary thyroid cancer: an overview. International journal of surgery, 41, S2-S6.
MEN2B
Some cases of MEN2B are inherited from parents. Individuals with MEN2B have a 100% of developing medullary thyroid carcinoma. Usually, there is a high risk of mutation and early onset of the carcinoma.
Familial Medullary Thyroid Cancer
This is a subvariant of MEN2B in which patients have a RET gene mutation, but develop only one type of cancer, i.e., MTC.
If doctors identify a RET gene mutation, preventive surgical removal of the thyroid gland can save you from cancer development. A surgeon nips the evil in the bud and prevents the aggressive tumor from developing (and going ablaze).
Medullary Thyroid Carcinoma Diagnosis
In several cases, diagnosis is made during routine examination (radiographic imaging) of the thyroid because very small tumors of the thyroid medulla do not cause any symptoms. When symptoms are present, a healthcare provider takes a history of symptoms, i.e., a lump in the neck and swelling of lymph nodes.
If presenting with a history of a neck lump and swollen lymph nodes, your healthcare provider will perform a physical examination to check the location of the swellings. When a thyroid pathology, such as a carcinoma, is suspected, your doctor will order the following tests:
Imaging Tests:
Several imaging tests help locate and identify nodules in the thyroid. Advanced MRI and CT scans do a decent job of aiding diagnosis. Studies show that functional imaging (primarily 18F-DOPA PET/CT scans) plays a vital role in the identification of tumors within the thyroid body and also aids in the detection of metastases.7Kushchayev, S. V., Kushchayeva, Y. S., Tella, S. H., Glushko, T., Pacak, K., & Teytelboym, O. M. (2019). Medullary thyroid carcinoma: an update on imaging. Journal of thyroid research, 2019(1), 1893047. An ultrasound scan may also be helpful in reaching a diagnosis.
Blood Tests:
The parafollicular cells are responsible for the production of the calcitonin hormone. An excess of C-cells eventually leads to overproduction of the hormone. Therefore, healthcare providers advise serum levels of calcitonin. Imaging scans paired with raised serum calcitonin levels point to underlying MTC.8Klain, M., Hadoux, J., Nappi, C., Finessi, M., Ambrosio, R., Schlumberger, M., … & Salvatore, D. (2022). Imaging medullary thyroid cancer patients with detectable serum markers: state of the art and future perspectives. Endocrine, 1-8.
A protein called the carcinoembryonic antigen (CEA) becomes significantly raised in cases of cancers like medullary thyroid carcinoma. Therefore, your doctor might also order serum CEA. The latest research shows that serum CEA is not a specific biomarker for the disease. However, it can provide vital information about the progression of the disease.9Passos, I., Stefanidou, E., Meditskou-Eythymiadou, S., Mironidou-Tzouveleki, M., Manaki, V., Magra, V., … & Sapalidis, K. (2021). A review of the significance in measuring preoperative and postoperative carcinoembryonic antigen (CEA) values in patients with medullary thyroid carcinoma (MTC). Medicina, 57(6), 609. Another study revealed that the rise in serum calcitonin and CEA levels correlates with the extent of MTC.10Turkdogan, S., Forest, V. I., Hier, M. P., Tamilia, M., Florea, A., & Payne, R. J. (2018). Carcinoembryonic antigen levels correlated with advanced disease in medullary thyroid cancer. Journal of Otolaryngology-Head & Neck Surgery, 47(1), 55.
Fine Needle Aspiration:
In fine needle aspiration biopsy, the doctor withdraws a small tissue sample from the thyroid nodule via a very thin needle. This test is not done very frequently.
Genetic Testing:
You might be advised to undergo genetic testing (analysis of one’s DNA) to identify genetic variations that may increase your propensity to get a medullary thyroid cancer.
Medullary Thyroid Carcinoma Staging
Doctors perform staging of the cancer to evaluate the progression of the tumor and its spread to other tissues (fat, muscle, lymph nodes, etc.). Healthcare workers commonly use the American Joint Committee on Cancer (AJCC) TNM system to stage thyroid cancer, which is as follows:11American Joint Committee on Cancer. (2017). AJCC cancer staging manual (8th ed.). Springer.
Tumor (T):
It denotes the size of the tumor.
Tx: Primary tumor can not be assessed.
T0: There is no evidence of primary tumor.
T1: The size of the tumor is 2cm across or smaller and has not grown beyond the thyroid.
T1a: The tumor size is 1cm (or smaller).
T1b: The tumor size is larger than 1 cm (but not larger than 2cm).
T2: The tumor size lies between 2 and 4 cm across and has not grown out of the thyroid gland.
T3: The tumor size is larger than 4 cm across and has started to grow outside the gland (into nearby tissues).
T4a: There is moderately advanced disease. The tumor is of any size and now extends beyond the thyroid gland. It has grown into nearby structures like the neck, the voice box, the windpipe, or the foodpipe. This stage also denotes extension of the tumor into the nerve supplying the larynx.
T4b: There is a very advanced disease. The tumor is of any size and has grown into the nearby blood vessels or the spine.
Node (N):
It denotes the involvement of lymph nodes by the tumor.
Nx: Nearby lymph nodes can not be assessed.
N0: The cancer hasn’t spread to nearby lymph nodes.
N1: The cancer has spread to the lymph nodes.
N1a: Spread to neck lymph nodes around the thyroid, including pretracheal, paratracheal, and prelaryngeal.
N1b: Spread to cervical (neck) lymph nodes, retropharyngeal (behind the throat) nodes, and superior mediastinal (upper chest) lymph nodes.
Metastasis:
Mx: No distant metastasis can be assessed.
M0: There is no distant metastasis.
M1: The cancer has metastasized (spread) to other body parts such as internal organs, bones, and distant lymph nodes, etc.
Stage Grouping:
Stages are declared based on the combination of TNM.
| Stage | Criteria |
|---|---|
| I | T1, N0, M0 |
| II | T2 or T3, N0, M0 |
| III | T1–T3, N1a, M0 |
| IVA | T4a, any N, M0 or T1–T3, N1b, M0 |
| IVB | T4b, any N, M0 |
| IVC | Any T, any N, M1 |
Differential Diagnosis:
Medullary Thyroid Carcinoma Vs Papillary Thyroid Carcinoma (PTC)
Both are types of thyroid cancer. However, MTC develops in the parafollicular cells while PTC originates from the follicular cells. MTC is more aggressive and raises calcitonin/carcinembryonic antigen levels, while PTC may raise thyroglobulin production is not as aggressive. Other diseases that may resemble MTC include:
- Follicular thyroid carcinoma
- Anaplastic thyroid carcinoma
- Oncocytic thyroid carcinoma
- Graves disease
- Thyrotoxicosis
Does Medullary Thyroid Carcinoma Spread To Other Body Parts?
Yes, medullary thyroid carcinoma is malignant and can spread to distant structures. The most common sites of metastasis include:
- Liver
- Lung
- Mediastinum
- Bone
Unusual sites of cancer metastasis include the breast, pancreas, and mandible.12Kazakou, P., Simeakis, G., Alevizaki, M., & Saltiki, K. (2021). Medullary thyroid carcinoma (MTC): unusual metastatic sites. Endocrinology, Diabetes & Metabolism Case Reports, 2021(1).
Medullary Thyroid Carcinoma Treatment
There are different approaches to treating medullary thyroid carcinoma. Generally, a multidisciplinary approach is ideal in treating this type of cancer.
Observation:
Hereditary patients with a low risk of cancer are put under regular monitoring. Doctors carry out ultrasounds routinely and keep an eye on the serum calcitonin levels. The surveillance helps keep unwanted surgery at bay. However, a rise in cancer biomarkers warrants immediate surgery.
Surgery:
Surgeons prophylactically remove the thyroid in high-risk inherited patients to prevent damage. Patients with high-risk RET mutations (especially MEN2A) are ideal candidates for early thyroidectomy. Most doctors perform the surgery before the patient reaches 5 years of age.
Thyroidectomy (removal of the thyroid gland) is the treatment of choice for localized tumors. However, in case of neck lymph node involvement, surgeons remove the nodes as well in a procedure called neck dissection.
Most surgeons perform total thyroidectomy (removal of the entire gland) for sporadically arising small tumors, i.e., having a size smaller than 1 cm and unilateral disease. However, for tumors larger than 1 cm with bilateral involvement, doctors usually go for total thyroidectomy with bilateral neck dissection.
Note: After a total thyroidectomy, you will need to take thyroid hormone medications for the rest of your life.
Radiation Therapy:
Radiotherapy is an adjuvant treatment for medullary thyroid carcinoma. External beam radiation therapy is considered when surgery is not feasible.
Chemotherapy:
Sometimes, doctors prescribe chemotherapeutic drugs to eliminate non-resectable cancerous growths. Commonly used drugs for MTC include doxorubicin and dacarbazine, etc.
Targeted Therapy:
Another modern strategy that has shown promising results in targeted therapy. It involves giving drugs for unresectable and symptomatic MTC. Vandetanib and cabozantinib are tyrosine kinase inhibitors that act on changes in the DNA structure. Other drugs of targeted therapy, such as selpercatinib, pralsetinib, and pembrolizumab, have shown great efficiency in alleviating symptoms and improving quality of life.13Priya, S. R., Dravid, C. S., Digumarti, R., & Dandekar, M. (2017). Targeted therapy for medullary thyroid cancer: a review. Frontiers in oncology, 7, 238.
Medullary Thyroid Carcinoma Prognosis
The prognosis is medullary thyroid carcinoma is not as good as other thyroid cancers, like papillary cancer. Therefore, early diagnosis and treatment can be helpful. Moreover, the prognosis of cancer therapy relies on the following factors:
- Patient’s age and generalized health: Worse prognosis for patients above 65 years
- Stage of the cancer: Terminal stage cancers have a poor prognosis
- Metastasis: Prognosis is poor if the cancer has spread to other parts of the body
- The extent of the tumor excised during the surgery: Incomplete removal of cancer can cause recurrence, and consequently, poor results
Medullary Thyroid Carcinoma Survival Rate
As per the latest research, the five-year survival rate for stages 1-3 of medullary thyroid carcinoma is 93%. However, the survival rate drops to 28% for stage 4 cases.
Final Word
Medullary thyroid carcinoma is a rare neuroendocrine cancer of the thyroid gland. This aggressive tumor arises in the parafollicular C cells (responsible for calcitonin hormone production) present in the medulla of the gland. In most cases, the cancers develop sporadically due to mutations in the RET gene. However, in a small portion of cases, inherited genetic mutation conditions like multiple endocrine neoplasm type 2 (MEN2A and MEN2B) lead to thyroid cancer. Small tumors are asymptomatic, while large tumors present with neck lumps that interfere with swallowing and breathing. Doctors mainly treat it with surgical excision of the gland (thyroidectomy). Radiation and chemotherapy can serve as adjuvants. Advanced targeted therapies (vandetanib and cabozantinib) are aiding in improving the life quality of patients.
Refrences
- 1Caillé, S., Debreuve-Theresette, A., Vitellius, G., Deguelte, S., La Manna, L., & Zalzali, M. (2024). Medullary thyroid cancer: epidemiology and characteristics according to data from the Marne-Ardennes Register 1975-2018. Journal of the Endocrine Society, 8(6), bvae084.
- 2Kushchayev, S. V., Kushchayeva, Y. S., Tella, S. H., Glushko, T., Pacak, K., & Teytelboym, O. M. (2019). Medullary thyroid carcinoma: an update on imaging. Journal of thyroid research, 2019(1), 1893047.
- 3Fan, W., Xiao, C., & Wu, F. (2018). Analysis of risk factors for cervical lymph node metastases in patients with sporadic medullary thyroid carcinoma. Journal of International Medical Research, 46(5), 1982-1989.
- 4Takeuchi, S., Yoshino, N., & Usuda, J. (2019). Hoarseness as an Initial Symptom of Thymic Carcinoma: A Case Report. Journal of Nippon Medical School, 86(6), 357-359.
- 5Krampitz, G. W., & Norton, J. A. (2014). RET gene mutations (genotype and phenotype) of multiple endocrine neoplasia type 2 and familial medullary thyroid carcinoma. Cancer, 120(13), 1920-1931.
- 6Accardo, G., Conzo, G., Esposito, D., Gambardella, C., Mazzella, M., Castaldo, F., … & Pasquali, D. (2017). Genetics of medullary thyroid cancer: an overview. International journal of surgery, 41, S2-S6.
- 7Kushchayev, S. V., Kushchayeva, Y. S., Tella, S. H., Glushko, T., Pacak, K., & Teytelboym, O. M. (2019). Medullary thyroid carcinoma: an update on imaging. Journal of thyroid research, 2019(1), 1893047.
- 8Klain, M., Hadoux, J., Nappi, C., Finessi, M., Ambrosio, R., Schlumberger, M., … & Salvatore, D. (2022). Imaging medullary thyroid cancer patients with detectable serum markers: state of the art and future perspectives. Endocrine, 1-8.
- 9Passos, I., Stefanidou, E., Meditskou-Eythymiadou, S., Mironidou-Tzouveleki, M., Manaki, V., Magra, V., … & Sapalidis, K. (2021). A review of the significance in measuring preoperative and postoperative carcinoembryonic antigen (CEA) values in patients with medullary thyroid carcinoma (MTC). Medicina, 57(6), 609.
- 10Turkdogan, S., Forest, V. I., Hier, M. P., Tamilia, M., Florea, A., & Payne, R. J. (2018). Carcinoembryonic antigen levels correlated with advanced disease in medullary thyroid cancer. Journal of Otolaryngology-Head & Neck Surgery, 47(1), 55.
- 11American Joint Committee on Cancer. (2017). AJCC cancer staging manual (8th ed.). Springer.
- 12Kazakou, P., Simeakis, G., Alevizaki, M., & Saltiki, K. (2021). Medullary thyroid carcinoma (MTC): unusual metastatic sites. Endocrinology, Diabetes & Metabolism Case Reports, 2021(1).
- 13Priya, S. R., Dravid, C. S., Digumarti, R., & Dandekar, M. (2017). Targeted therapy for medullary thyroid cancer: a review. Frontiers in oncology, 7, 238.

