MCC, or Merkel Cell Carcinoma, is a neuroendocrine-specific kind of rare and aggressive skin tumor. It takes place more frequently, being prevalent among elderly white men. The causative factors of MCC includes UV radiation, advanced age, and low immune response, Merkel cell polyomavirus.
Confirming MCC is done by taking a skin biopsy. Sentinel lymph node assessment is important to the tumor’s inherent rapid progression. Its therapy usually involves a tumor excision plus radiotherapy but monotherapy can also be implemented.
What is Merkel Cell Carcinoma?
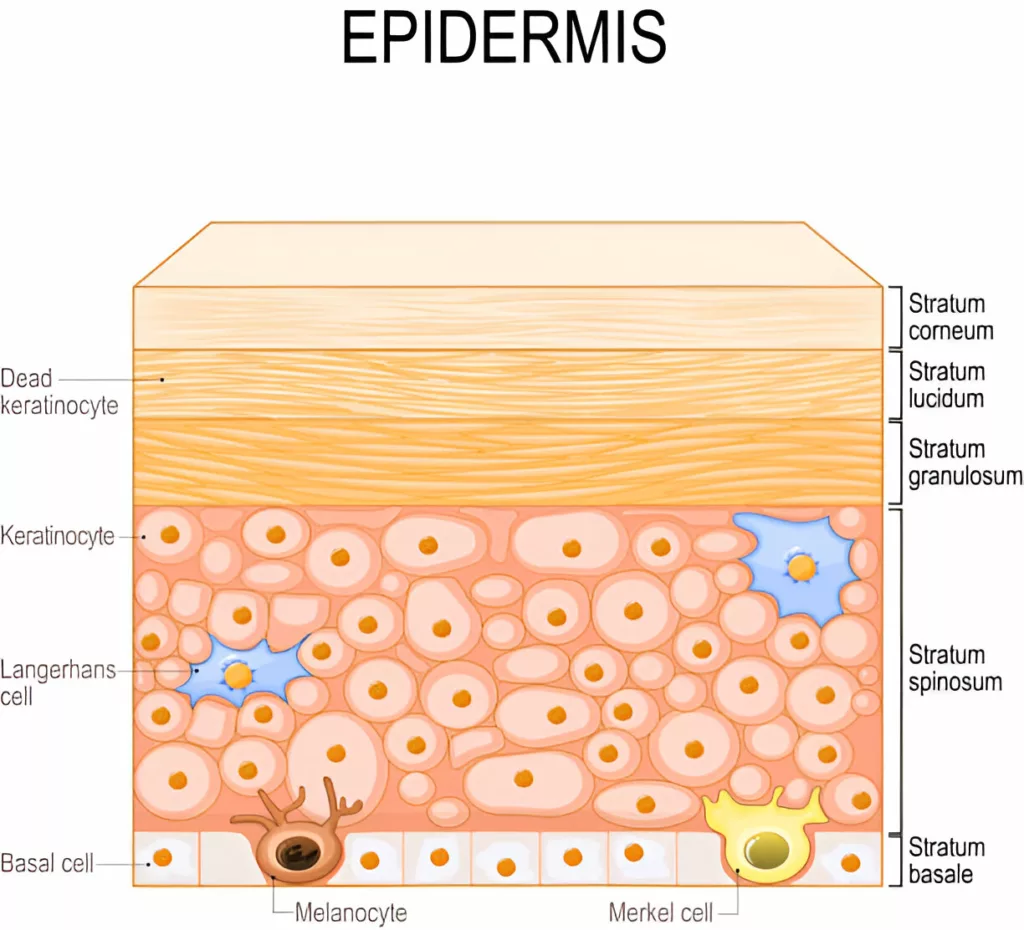
Merkel Cell Carcinoma is a rare form of skin cancer. It results from the uncontrolled proliferation of Merkel cells in the skin.1Brady M, Spiker AM. MCC of the Skin. [Updated 2023 Jul 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482329/ Its cells are located in the superficial layer of the skin. There, they are closely associated with nerve endings which are responsible for the perception of touch. Merkel cell carcinoma is also known as neuroendocrine carcinoma of the skin or trabecular cancer.
The symptoms of Merkel cell carcinoma appear late. By then, the cancer has spread to other parts of the body in 30% of patients.2Becker, J. C., Stang, A., DeCaprio, J. A., Cerroni, L., Lebbé, C., Veness, M., & Nghiem, P. (2017). MCC. Nature reviews. Disease primers, 3, 17077. https://doi.org/10.1038/nrdp.2017.77
Causes of Merkel Cell Carcinoma
The primary causes of Merkel Cell Carcinoma (MCC) include:
- Prolonged exposure to ultraviolet (UV) light, such as sunlight
- Infection with the Merkel cell polyomavirus3Liu, W., Krump, N. A., Buck, C. B., & You, J. (2019). Merkel Cell Polyomavirus Infection and Detection. Journal of visualized experiments: JoVE, (144), 10.3791/58950. https://doi.org/10.3791/58950
Merkel cell carcinoma (MCC) is an aggressive neuroendocrine skin cancer that primarily affects older adults with fair skin. The disease can be caused by the Merkel cell polyomavirus (MCV) in approximately 80% of cases, while the remaining 20% arise due to ultraviolet (UV) radiation-induced DNA damage.
Although both forms of MCC may appear similar under the microscope, viral MCC typically has fewer DNA mutations compared to UV-induced MCC, which carries a high mutation burden. UV exposure plays a significant role in the development of non-viral MCC by causing direct DNA damage and impairing immune surveillance. MCC usually appears as a painless, firm, red, or purple nodule on sun-exposed areas and has a high potential for metastasis, making early detection crucial.4Tello, T. L., Coggshall, K., Yom, S. S., & Yu, S. S. (2018). MCC: An update and review: Current and future therapy. Journal of the American Academy of Dermatology, 78(3), 445–454. https://doi.org/10.1016/j.jaad.2017.12.0045Ryu, W.-S. (2017). Polyomaviruses. Molecular Virology of Human Pathogenic Viruses, 85–95. https://doi.org/10.1016/b978-0-12-800838-6.00006-0
Risk Factors of Merkel Cell Carcinoma
MCC predominantly affects older adults with fair skin, particularly males. Although MCC can occur in individuals of any age or skin tone, more than 90% of cases are diagnosed in Caucasians.6Brady M, Spiker AM. Merkel Cell Carcinoma of the Skin. [Updated 2023 Jul 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482329/ The incidence of MCC has been rising, particularly in regions with aging populations and high ultraviolet (UV) exposure, such as the U.S. and Australia. This increase is attributed to improved diagnostic techniques, greater awareness, and a growing number of people with known risk factors. Despite advances in detection, MCC remains highly aggressive, with a significant risk of metastasis, contributing to its high mortality rate.7Brady M, Spiker AM. MCC of the Skin. [Updated 2023 Jul 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482329/
Symptoms of Merkel Cell Carcinoma
Merkel cell carcinoma (MCC) typically presents as a firm, rapidly growing nodule on sun-exposed skin, such as the face, neck, arms, or scalp. The lesion is usually painless at first but may become tender if it ulcerates or bleeds. The tumor can be skin-colored, red, purple, or bluish-red and may resemble a pimple, bug bite, or cyst.
Additional Symptoms of Merkel Cell Carcinoma:
The additional symptoms of Merkel cell carcinoma include:
- Fast-growing nodule (Typically grows rapidly over weeks to months, often resembling a pimple or a cyst).
- Red or purple patches on the skin.
- Tenderness or pain at the site of the lesion, especially if it becomes ulcerated or infected.
- Some lymph nodes may become enlarged and tender to the touch (If the cancer has spread to nearby regions).
- Itching or a burning sensation in the affected area.
- The tumor can ulcerate or bleed, leading to crusting or scabbing over the lesion.
Diagnosis & Tests for Merkel Cell Carcinoma
Diagnosis of MCC involves:
- Physical examination: Your doctor will check the skin for rapidly growing, painless nodules and examine nearby lymph nodes for swelling, as MCC commonly spreads early.
- Skin biopsy: A small piece of the suspicious skin is removed for analysis in a lab to check for cancer signs. Special immunohistochemical staining (such as CK20 and neuroendocrine markers) helps distinguish MCC from other skin cancers.8Patel, P., & Hussain, K. (2021). MCC. Clinical and experimental dermatology, 46(5), 814–819. https://doi.org/10.1111/ced.14530
To determine the extent of cancer spread, your doctor may use:
- Sentinel lymph node biopsy: A small amount of dye is injected near the tumor to identify the first lymph node(s) that may contain cancer. These nodes are surgically removed and examined microscopically for metastasis.
- Imaging tests: Chest X-ray and CT scans of the chest and abdomen can help detect cancer spread to other organs.
- Additional tests like PET scans or octreotide scans may also be considered to track cancer cell spread.
Stages of Merkel Cell Carcinoma
American Joint Committee on Cancer (AJCC) staging system is typically used for MCC, and it is based on tumor size (T), lymph node involvement (N), and metastasis (M).
The stages range from 0 (limited to the skin’s outer layer) to IV (involving distant organs). Because staging indicates prognosis and informs treatment recommendations, it is crucial.
This table breaks down the different stages of MCC and what they mean for the cancer’s progression and spread.
| Stage | Description |
|---|
| 0 | Cancer is in situ, meaning it is only in the top layer of the skin (epidermis) and has not invaded deeper tissues. |
| 1 | The tumor is ≤2 cm in size with no spread to lymph nodes. |
| 2A | The tumor is >2 cm but has not spread to lymph nodes. |
| 2B | The tumor has grown into nearby structures such as muscle, bone, or cartilage but has not reached lymph nodes. |
| 3A | Cancer has spread to lymph nodes, but the spread is only detected microscopically (not visible or palpable). |
| 3B | Cancer has spread to lymph nodes, which are visibly enlarged or detected via imaging. |
| 4 | Cancer has spread beyond regional lymph nodes to distant organs such as the liver, lungs, or bones. |
Treatment of Merkel Cell Carcinoma
The Merkel Cell Cancer’s stage determines how it will be treated. Compared to late-stage MCC (stages III and IV), early-stage MCC (stages 0 to II) responds better to treatment.
Basically, four treatment options are available for MCC treatment:
- Surgery: The primary treatment for localized MCC is wide local excision (WLE) with or without sentinel lymph node biopsy. Mohs micrographic surgery (MMS) may be considered for tumors on the face or cosmetically sensitive areas.9Nguyen, B. J., Meer, E. A., Bautista, S. A., Kim, D. H., Etzkorn, J. R., McGeehan, B., Miller, C. J., & Briceno, C. A. (2023). Mohs Micrographic Surgery for Facial MCC. Journal of cutaneous medicine and surgery, 27(1), 28–33. https://doi.org/10.1177/12034754221143080
- Radiation therapy: High-energy radiation is often used to target remaining cancer cells after surgery, particularly in cases with high-risk features (e.g., large tumors or lymph node involvement).
- Chemotherapy: Drugs are used to stop cancer cell growth. They can be taken orally, injected into a vein, or a muscle (systemic chemotherapy).
- Immunotherapy: Immune checkpoint inhibitors, such as pembrolizumab and avelumab, are now the preferred first-line treatment for advanced MCC, as they help the immune system recognize and destroy cancer cells.
Prognosis of Merkel Cell Carcinoma
Five years following diagnosis, experts estimate that 75% of people with localized carcinoma survive, compared to 25% of those with metastatic cancer. Current clinical studies are investigating novel medicines for this difficult-to-treat malignancy.10Nayak, A. L., Pickett, A. T., Delisle, M., Dingley, B., Mallick, R., Hamilton, T., Stuart, H., Talbot, M., McKinnon, G., Jost, E., Thiboutot, E., Francescutti, V., Samman, S., Easson, A., Schellenberg, A., Merchant, S., La, J., Vanderbeck, K., Wright, F., Berger-Richardson, D., … Johnson-Obaseki, S. (2023). Survival of Patients With Head and Neck Merkel Cell Cancer: Findings From the Pan-Canadian Merkel Cell Cancer Collaborative. JAMA network open, 6(11), e2344127. https://doi.org/10.1001/jamanetworkopen.2023.44127
Complications of Merkel Cell Carcinoma
Its treatment is more difficult because the cancer is aggressive and can spread fast to other places of the body. Metastatic cancer is the term used to describe cancer that has migrated beyond its original site. The lymphatic system, or lymph nodes, is where MCC metastasizes most frequently. It can move to the brain, lungs, bones, or other organs, where it can be fatal.
Life Expectancy of Merkel Cell Carcinoma
According to the American Cancer Society, the 5-year survival rate for MCC varies depending on the stage at diagnosis:11American Cancer Society. (2024). Survival rates for Merkel cell carcinoma. Retrieved from https://www.cancer.org/cancer/types/merkel-cell-skin-cancer/detection-diagnosis-staging/survival-rates.html
- For localized tumors (cancer that has not spread beyond the original site), the 5-year survival rate is around 70% to 80%.
- If the cancer has spread to nearby lymph nodes, the 5-year survival rate is about 50%.
- When the cancer has spread to distant organs or tissues, the 5-year survival rate is lower, around 20% to 40%.
Basal Cell Carcinoma (BCC) Vs Merkel Cell Carcinoma (MCC)
BCC originates from basal keratinocytes in the epidermis, while MCC arises from Merkel cells, which are neuroendocrine cells in the skin. Basal cell carcinoma is slow-growing and rarely metastasizes, whereas MCC is highly aggressive and often spreads early. It is usually treated with simple excision or Mohs surgery, whereas MCC requires more aggressive treatment, including surgery, radiation, and immunotherapy.
Although Merkel Cell Carcinoma is uncommon, it can have serious consequences. It is critical to place a high priority on prevention, early detection, and efficient treatment as we continue to explore this skin cancer and learn more about its complexity. If you have any concerns about changes to your skin, speak with your healthcare professional, stay informed, and shield your skin from damaging UV rays. We are winning the fight against Merkel Cell Carcinoma thanks to our devotion and medical improvements.
Refrences
- 1Brady M, Spiker AM. MCC of the Skin. [Updated 2023 Jul 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482329/
- 2Becker, J. C., Stang, A., DeCaprio, J. A., Cerroni, L., Lebbé, C., Veness, M., & Nghiem, P. (2017). MCC. Nature reviews. Disease primers, 3, 17077. https://doi.org/10.1038/nrdp.2017.77
- 3Liu, W., Krump, N. A., Buck, C. B., & You, J. (2019). Merkel Cell Polyomavirus Infection and Detection. Journal of visualized experiments: JoVE, (144), 10.3791/58950. https://doi.org/10.3791/58950
- 4Tello, T. L., Coggshall, K., Yom, S. S., & Yu, S. S. (2018). MCC: An update and review: Current and future therapy. Journal of the American Academy of Dermatology, 78(3), 445–454. https://doi.org/10.1016/j.jaad.2017.12.004
- 5Ryu, W.-S. (2017). Polyomaviruses. Molecular Virology of Human Pathogenic Viruses, 85–95. https://doi.org/10.1016/b978-0-12-800838-6.00006-0
- 6Brady M, Spiker AM. Merkel Cell Carcinoma of the Skin. [Updated 2023 Jul 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482329/
- 7Brady M, Spiker AM. MCC of the Skin. [Updated 2023 Jul 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482329/
- 8Patel, P., & Hussain, K. (2021). MCC. Clinical and experimental dermatology, 46(5), 814–819. https://doi.org/10.1111/ced.14530
- 9Nguyen, B. J., Meer, E. A., Bautista, S. A., Kim, D. H., Etzkorn, J. R., McGeehan, B., Miller, C. J., & Briceno, C. A. (2023). Mohs Micrographic Surgery for Facial MCC. Journal of cutaneous medicine and surgery, 27(1), 28–33. https://doi.org/10.1177/12034754221143080
- 10Nayak, A. L., Pickett, A. T., Delisle, M., Dingley, B., Mallick, R., Hamilton, T., Stuart, H., Talbot, M., McKinnon, G., Jost, E., Thiboutot, E., Francescutti, V., Samman, S., Easson, A., Schellenberg, A., Merchant, S., La, J., Vanderbeck, K., Wright, F., Berger-Richardson, D., … Johnson-Obaseki, S. (2023). Survival of Patients With Head and Neck Merkel Cell Cancer: Findings From the Pan-Canadian Merkel Cell Cancer Collaborative. JAMA network open, 6(11), e2344127. https://doi.org/10.1001/jamanetworkopen.2023.44127
- 11American Cancer Society. (2024). Survival rates for Merkel cell carcinoma. Retrieved from https://www.cancer.org/cancer/types/merkel-cell-skin-cancer/detection-diagnosis-staging/survival-rates.html

