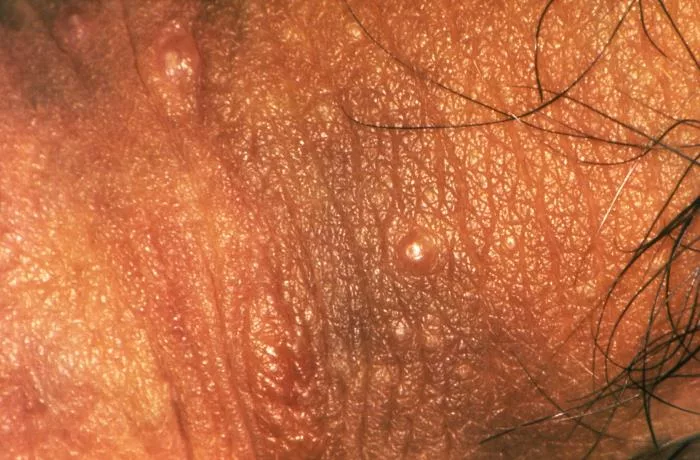
Molluscum Contagiosum is a viral skin condition in which there is the formation of multiple raised, smooth, pearl-like bumps (papules) on the skin. These papules can last anywhere from several months to a few years. Molluscum Rash is highly contagious and spreads easily. However, treatment can help clear the infection. Medical intervention is not always required, as the infection often resolves on its own over time.
What is Molluscum Contagiosum?
Molluscum Contagiosum is a common viral skin infection affecting millions worldwide. It causes raised, umbilicated, round, firm, painless bumps. This disease is mostly seen in children between the ages of 1 and 10, but it can also occur in adults who are immunocompromised or healthy individuals who have sexual activity with an infected person. Even though this condition is benign, it can lead to psychological distress because of its physical appearance. Molluscum Contagiosum Virus (MCV), a member of the Poxviridae family, causes this infection.1 Hanson, Daniel, and Dayna G. Diven. “Molluscum contagiosum.” Dermatology online journal 9.2 (2003). Understanding the pathophysiology and clinical features of Molluscum Contagiosum is necessary to effectively manage and treat this disease.

Causes of Molluscum Contagiosum
Molluscum Contagiosum Virus has double-stranded DNA and four further subtypes. MCV-1 is the most common subtype found in children. Children aged 1-14 years have the highest incidence rate of this disease.2 Olsen, Jonathan R., et al. “Epidemiology of molluscum contagiosum in children: a systematic review.” Family Practice 31.2 (2014): 130-136 Below are some factors that contribute to the spread of this disease.
Skin-to-Skin Contact
This is the primary route of infection that can occur, especially when people are in proximity, such as children in schools, daycares, and community centers.
Contact with Infected Objects (Fomites)
The Molluscum Contagiosum Virus can survive on surfaces such as towels, bedding, and clothes. Moreover, sharing personal hygiene items and communal equipment can increase the chances of contracting this disease.
Swimming in Pools
This virus thrives in warm and humid environments, making swimming pools and saunas a particularly common mode of transmission. Furthermore, direct contact with water-based activities increases the likelihood of acquiring this disease.
Sexual Activity with an Infected Person
Molluscum Contagiosum is a sexually transmitted disease in adults. As a result, lesions occur in the groins, inner things, and genitals when a person is involved in sexual activity with an infected person.3 Brown, Tricia J., Angela Yen-Moore, and Stephen K. Tyring. “An overview of sexually transmitted diseases. Part II.” Journal of the American Academy of Dermatology 41.5 (1999): 661-680. In particular, young adults who have unprotected contact with multiple partners are at higher risk of getting infected.

Autoinoculation
Autoinoculation happens when a person scratches or touches a lesion and then spreads the infection to other parts of their body. Additionally, shaving over lesions can also facilitate the spread of infection.
Risk factors of Molluscum Contagiosum
Immunocompromised individuals who have HIV/AIDS,4 Schwartz, Joseph J., and Patricia L. Myskowski. “Molluscum contagiosum in patients with human immunodeficiency virus infection: a review of twenty-seven patients.” Journal of the American Academy of Dermatology 27.4 (1992): 583-588. cancers or those undergoing immunosuppressive therapies, for example, post-transplant patients, are significantly at a higher risk of contracting Molluscum contagiosum.
Children and adults with eczema and atopic dermatitis are also more susceptible to getting molluscum contagiosum. Their skin barrier is compromised, which facilitates viral entry.5 Olsen, Jonathan R., et al. “Molluscum contagiosum and associations with atopic eczema in children: a retrospective longitudinal study in primary care.” British Journal of General Practice 66.642 (2016): e53-e58.
Symptoms of Molluscum Contagiosum
The hallmark of Molluscum Contagiosum is the presence of distinct, raised skin lesions often referred to as Molluscum papules. These bumps are generally painless, but they cause psychological and emotional distress due to their appearance and, in some cases, physical irritation, especially in adults when the papules are formed on the genitals and adjacent areas. Symptoms vary in severity based on multiple factors like age, hygiene, and the patient’s immunity.
Papules:
Lesions are typically smooth, dome-shaped, and flesh-colored or slightly pink. They can vary in size from 2-5 millimeters but can grow larger too. A defining feature of these lesions is a central dimple or depression, giving them a “pearl-like” or umbilicated appearance.
Lesions can occur on any part of the body but are most common on the face, trunk, arms, and legs in children. In adults, inner thighs and genitals are more commonly affected if the virus is spread sexually. The palms and soles are usually spared, differentiating Molluscum from other skin conditions like warts.
Lesion Distribution & Cluster Formation:
Cluster formation
Papules often appear as clusters. Clustering occurs because of autoinoculation, where the individual spreads the virus to different parts of their own body through scratching or touching.
Localized vs. Generalized Lesions
In healthy individuals, lesions are typically localized, but in immunocompromised people, more widespread lesions across larger areas of the body can be seen.
Itching & Irritation:
Usually, the lesions are painless, but mild to moderate itching is a complaint, especially in children. Scratching the papules can lead to secondary bacterial infections or exacerbate the spread of the virus.
Inflammation:
In some cases, lesions become red and inflamed this can happen during the body’s immune response or due to irritation caused by rubbing clothes, friction, and scratching.
Secondary Infection:
If the lesions are scratched, bacterial infection may occur, leading to complications such as crusting, pus formation, and pain.
Psychological Impact:
Although molluscum contagiosum is primarily a cosmetic concern, the visible nature of the lesion can cause emotional distress, particularly in older children and adolescents. Individuals may feel embarrassed and self-conscious.
Asymptomatic Nature:
In some cases, individuals may not experience any visible symptoms, especially in the early stages. This asymptomatic nature can delay diagnosis and increase the likelihood of unintentional spread of the virus.
Symptoms in Immune-Compromised Individuals:
The lesions are usually larger, numerous, and resistant. They appear in atypical locations like the scalp and oral mucosa or around the eyes.
When to Seek Medical Help for Molluscum Contagiosum
While Molluscum contagiosum resolves on its own without medical intervention, consult a healthcare professional if:
- Lesions become painful and inflamed and indicate infection
- The number of lesions increases rapidly
- If, due to a weakened immune system, the lesions are persistent or extensive
- Vision concerns occur due to lesions near the eye
Stages
Molluscum Contagiosum progresses through various stages, from initial infection to final resolution. Understanding these stages is crucial for correct diagnosis and effective management of the symptoms. While the exact timelines vary among individuals, the stages typically include the following:
Incubation or Asymptomatic Stage:
It usually averages two to three months but may range from one week to six months. After the virus enters the skin, it replicates in the epidermal cells. During this stage, no visible symptoms are present. However, the person unknowingly can spread the virus through contact as the virus can still be contagious even before lesions appear.
Initial Appearance:
At the end of the incubation period, small papules begin to appear on the skin. Lesions are typically flesh-colored, dome-shaped, and smooth, with a diameter of 1-2 millimeters. These lesions are painless and non-itchy, but they may cluster depending on the site of infection.
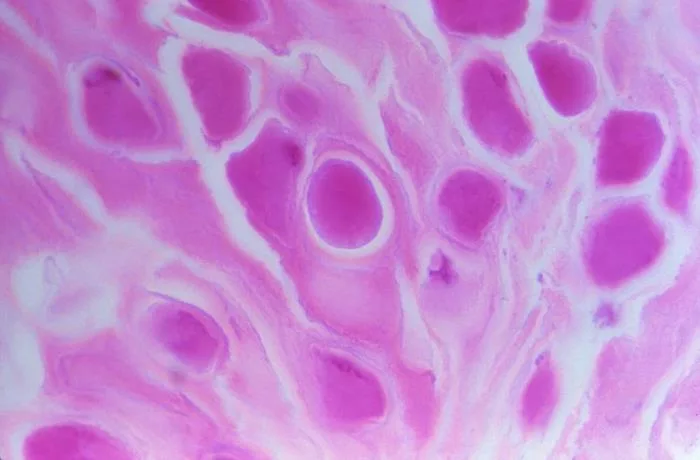
Growth & Maturation Stage:
This may appear weeks to months after the initial lesion. The lesions grow larger, reaching their full size of 2-5 millimeters in diameter and with characteristic umbilication or central dimple.6Leung, Alexander KC, Benjamin Barankin, and Kam LE Hon. “Molluscum contagiosum: an update.” Recent patents on inflammation & allergy drug discovery 11.1 (2017): 22-31. Clusters may form and become mildly itchy during this phase due to scratching. Furthermore, cosmetic concerns may occur at this stage.
Resolution:
The time frame for resolution varies from individual to individual. In healthy individuals, it resolves on its own within 6 to 12 months, but it can take up to 4 years in immunocompromised patients. Eventually, lesions shrink and flatten over time leaving behind slight discoloration or scarring.
Recurrence:
In people with weak immune systems, the virus may bypass the resolution stage, causing persistent or recurrent lesions.
Treatment
As molluscum contagiosum is considered a self-limiting disease, debate continues about whether lesions associated with the disease should be treated or allowed to resolve spontaneously. However, treatment may be required in cases where the lesions cause discomfort, emotional distress, or secondary infection.
Treatment options are as follows.
Topical Therapies:
Topical treatments aim to destroy the infected skin cells or stimulate an immune response to clear the virus. Common options include:
Salicylic Acid
It’s a keratolytic agent that helps break down the skin layers of lesions. Salicylic acid is effective in reducing lesion size but may cause irritation or a burning sensation.
Cantharidin
This may be used in adults and children. It is a blistering agent and is applied by the healthcare provider. Blistering of the lesion by cantharidin facilitates its removal. It is the treatment of choice in most cases.7Robinson, Gabrielle, Steven Townsend, and Marla N. Jahnke. “Molluscum contagiosum: review and update on clinical presentation, diagnosis, risk, prevention, and treatment.” Current Dermatology Reports 9 (2020): 83-92.
Imiquimod
It is not recommended for young kids. A prescription is required to purchase it. Imiquimod is an immune response modifier that stimulates the body’s defenses to attack the virus. It may take weeks or months to be effective.
Potassium Hydroxide 10-20%
The lesion dissolves by breaking down the skin cells after using this strong alkali. However, careful application is required to avoid irritation of surrounding skin.
Physical Removal Methods:
For patients who desire quicker results, physical removal methods may be performed by a dermatologist or healthcare provider. These include:
Cryotherapy (Freezing)
The process includes applying liquid nitrogen to the lesion, causing it to scab and fall off. It is effective for smaller clusters, but it may require multiple sessions. Temporary discomfort and scarring can be a few side effects of this treatment. It may be an uncomfortable or a bit painful process so it is not a good option for young children.

Curettage (Surgical Scraping)
This procedure needs to be done by a well-trained healthcare provider. The lesion is physically scraped off using a curette (a surgical instrument designed for scraping or debriding biological tissue) after numbing the area; it provides immediate removal but can be painful and may leave scars. This procedure can be done in older children, teens, and adults.
Laser Therapy
This effective but expensive treatment is typically reserved for extensive or resistant cases. A focused light is used to destroy the lesions, particularly in cases where other treatments have failed. Pulsed Dye Laser (PDL) is recommended for patients with difficult-to-treat molluscum (e.g., patients with AIDS); it may cause temporary hyper- or hypopigmentation in the skin.8Hebert, Adelaide A., Neal Bhatia, and James Q. Del Rosso. “Molluscum contagiosum: epidemiology, considerations, treatment options, and therapeutic gaps.” The Journal of Clinical and Aesthetic Dermatology 16.8 Suppl 1 (2023): S4.
Systemic Treatments:
Systemic treatments are rarely required but may be considered in immunocompromised individuals or cases of widespread infection. These include:
Antiviral Medication
This is used in severe cases and for people with compromised immunity, such as those with HIV/AIDS.
Oral Immune Modulators
These boost the immune response to help the body clear the infection.
Supportive Care:
Supportive care plays a vital role in managing Molluscum Contagiosum. It not only helps alleviate symptoms but also prevents complications. Below are some of the steps that can be taken to significantly improve the recovery process:
Hygiene Practices
Maintaining proper hygiene is crucial. Avoid scratching to minimize autoinoculation (spreading the virus to other areas of your skin). Regularly cleaning the affected areas with gentle soap and water helps reduce the chance of infection. Additionally, lesions should be kept dry and covered with bandages, particularly when in communal spaces like schools, gyms, or swimming pools.

Preventing Spread
Another key focus of supportive care is preventing the virus from spreading to others. Avoid sharing personal items like towels, razors, and bedding. Ensure these items are for personal use only and washed regularly.
Until lesions are fully resolved, it is advisable to avoid contact sports (e.g., wrestling, martial arts) and swimming in communal pools.
Treating Secondary Infections
Occasionally, lesions may become irritated or infected due to scratching or friction. Monitor signs of infection and use antibiotic oral or topical as advised by the healthcare provider if necessary.
Comparison of Molluscum Contagiosum and Warts
Molluscum Contagiosum and warts are both common skin conditions caused by viral infections, but they differ in appearance, causes, and treatment approaches. The table below highlights the key differences to help distinguish between the two conditions.
| Feature | Molluscum Contagiosum | Warts |
| Cause | Molluscum Contagiosum Virus (MCV) | Human Papillomavirus (HPV) 9Jabłonska, Stefania, et al. “Cutaneous warts.” Clinics in Dermatology 15.3 (1997): 309-319. |
| Appearance | Smooth, dome-shaped with a central dimple | Rough, raised, sometimes flat or spiky |
| Location | Common on face, torso, limbs | Often on hands, feet, and face |
| Contagiousness | Highly contagious through direct contact | Contagious, but typically less than MC |
| Transmission via Objects | Easily transmitted through shared items | Transmitted, but less common via objects |
| Symptoms | Usually painless, mild itching | It can be painful (e.g., plantar warts) |
| Duration | 6–12 months (can last longer) | Varies, from months to years without treatment |
Conclusion
Molluscum Contagiosum is a skin condition caused by a highly contagious virus that spreads easily through contact and communal settings. While the lesions are typically painless and self-limiting, understanding the symptoms, stages, and preventive measures is essential for controlling their spread. Differentiating between MC and other similar skin conditions allows for more accurate diagnosis and effective management.
Refrences
- 1Hanson, Daniel, and Dayna G. Diven. “Molluscum contagiosum.” Dermatology online journal 9.2 (2003).
- 2Olsen, Jonathan R., et al. “Epidemiology of molluscum contagiosum in children: a systematic review.” Family Practice 31.2 (2014): 130-136
- 3Brown, Tricia J., Angela Yen-Moore, and Stephen K. Tyring. “An overview of sexually transmitted diseases. Part II.” Journal of the American Academy of Dermatology 41.5 (1999): 661-680.
- 4Schwartz, Joseph J., and Patricia L. Myskowski. “Molluscum contagiosum in patients with human immunodeficiency virus infection: a review of twenty-seven patients.” Journal of the American Academy of Dermatology 27.4 (1992): 583-588.
- 5Olsen, Jonathan R., et al. “Molluscum contagiosum and associations with atopic eczema in children: a retrospective longitudinal study in primary care.” British Journal of General Practice 66.642 (2016): e53-e58.
- 6Leung, Alexander KC, Benjamin Barankin, and Kam LE Hon. “Molluscum contagiosum: an update.” Recent patents on inflammation & allergy drug discovery 11.1 (2017): 22-31.
- 7Robinson, Gabrielle, Steven Townsend, and Marla N. Jahnke. “Molluscum contagiosum: review and update on clinical presentation, diagnosis, risk, prevention, and treatment.” Current Dermatology Reports 9 (2020): 83-92.
- 8Hebert, Adelaide A., Neal Bhatia, and James Q. Del Rosso. “Molluscum contagiosum: epidemiology, considerations, treatment options, and therapeutic gaps.” The Journal of Clinical and Aesthetic Dermatology 16.8 Suppl 1 (2023): S4.
- 9Jabłonska, Stefania, et al. “Cutaneous warts.” Clinics in Dermatology 15.3 (1997): 309-319.

