Multiple Myeloma is a severe blood cancer in which plasma cells and their products grow uncontrollably. This overproduction causes damage to vital organs and can even cause death.
What is Multiple Myeloma?
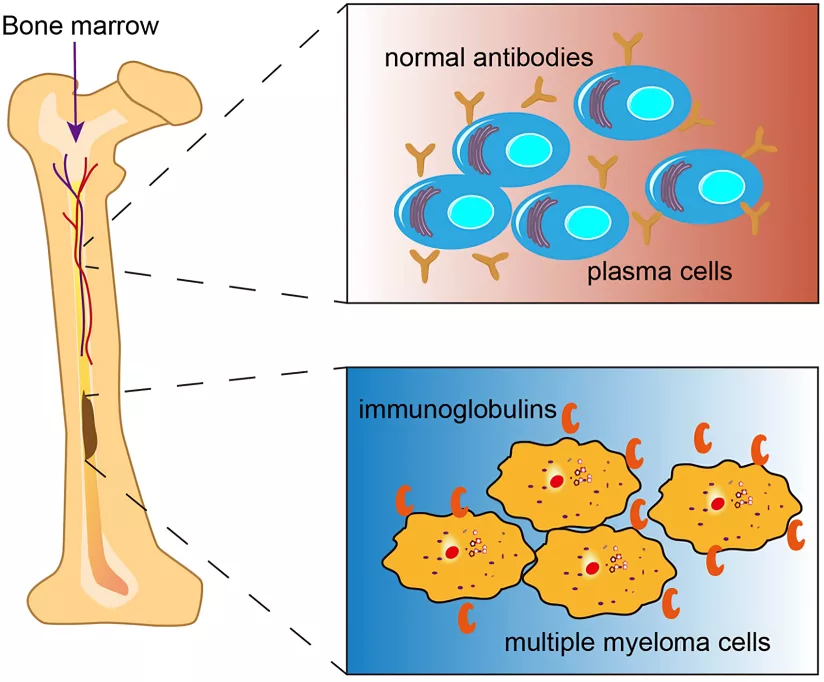
It is a type of cancer that arises from plasma cells. Plasma cells are white blood cells present in the bone marrow. They produce various immunoglobulins or antibodies, such as the IgA and IgG antibodies, to help fight infections.
When abnormal plasma cells multiply uncontrollably, they produce a defective protein called monoclonal “M” protein. This protein abnormality disrupts normal blood cell production and damages bones, kidneys, and the immune system.
Why is it called Multiple Myeloma?
“Multiple” shows how this cancer often impacts several areas of the bone marrow across the body, including the spine, skull, pelvis, and ribs. It also highlights the various stages of disease progression. “Myeloma,” on the other hand, is derived from the Greek words “myelo,” meaning bone marrow, and “-oma,” meaning tumor. So, “myeloma” refers to a cancer originating in the bone marrow. Some other names include:
- Plasma cell myeloma
- Kahler’s disease
- Myelomatosis
- Medullary plasmacytoma
How common is Multiple Myeloma?
The lifetime risk of an American for developing this condition is less than 1%, which makes it a relatively rare cancer. Globally, multiple myeloma accounts for 10% of all blood cancers. Worldwide, about 160,000 people are diagnosed with multiple myeloma each year. The number of new cases varies depending on the country, with 0.54 to 5.3 cases per 100,000 people. The incidence is 7.3 per 100,000 in America, which is higher than in many other parts of the world. 1Ludwig, H., Durie, S. N., Meckl, A., Hinke, A., & Durie, B. (2020). Multiple Myeloma Incidence and Mortality Around the Globe; Interrelations Between Health Access and Quality, Economic Resources, and Patient Empowerment. The Oncologist, 25(9), e1406–e1413. https://doi.org/10.1634/theoncologist.2020-0141
What causes Multiple Myeloma?
No pinpointed cause for this condition has been established. However, scientists have discovered that it is mainly a result of genetic mutations influenced by environmental and hereditary factors.
These abnormalities cause changes in plasma cell proliferation through several mechanisms:
- Translocations—where parts of chromosomes are swapped—and deletions—where parts of chromosomes simply do not exist—are commonly seen in multiple myeloma. These lead to the overproduction of abnormal plasma cells and more aggressive forms of disease.
- The overexpression of oncogenes such as the MYC also causes more serious complications in this condition.
- Like other cancers, multiple myeloma has been associated with gene mutations, such as the KRAS, NAS, TP53, and BRAF. These alterations affect cell growth, including the growth of plasma cells, which becomes abnormal in multiple myeloma.
- As a result of all these changes, the genes encoded for heavy chain regions of antibodies are affected. These genes instruct the body to produce abnormal plasma cell proteins, which is the hallmark diagnostic feature of multiple myeloma. 2Prideaux, S. M., O’Brien, E. C., & Chevassut, T. J. (2014). The Genetic Architecture of Multiple Myeloma. Advances in Hematology, 2014, 1–16. https://doi.org/10.1155/2014/864058
Who is at Greatest Risk for Multiple Myeloma?
There are strong associations between certain diseases and lifestyles that highly increase the risk of this condition.
- Most people with multiple myeloma are over 65. It’s rare in younger adults and almost unheard of before age 40.
- African Americans are more likely to develop this cancer than white Americans. It’s also more common in the Middle East, North Africa, and the Mediterranean.
- Men have a slightly higher risk of multiple myeloma than women.
- If someone in your family has had multiple myeloma, your risk might be higher.
However, most cases are sporadic and not associated with family history. - If you’ve had a plasma cell disorder or tumor before, you’re more likely to develop multiple myeloma in the future. For instance, monoclonal gammopathy of undetermined significance or MGUS is a preliminary stage of multiple myeloma development. It does not have symptoms, but it can increase your chances of getting multiple myeloma.
- Exposure to high radiation levels or chemicals — benzene, pesticides, or herbicides —can raise your risk.
- Certain jobs, like carpentry or furniture making, can increase your chances of developing multiple myeloma.
- Being overweight or obese could also make you more likely to develop this
Types of Multiple Myeloma
Two of the key types that doctors use to classify this condition are hyperdiploid and non-hyperdiploid. Understanding multiple myeloma types can help explain why the disease behaves differently and how to improve disease outcomes in different individuals.
Hyperdiploid Multiple Myeloma
Hyperdiploid multiple myeloma accounts for approximately 50–60% of all multiple myeloma cases. It
is characterized by the gain of odd-numbered chromosomes, such as chromosomes 3, 5, 7, 9, 11, 15, 19, and 21. The total chromosome count in cells affected by hyperdiploid myeloma is greater than 46, the usual number of chromosomes in a human. It is generally associated with a better prognosis because patients react favorably to standard treatments. Hyperdiploid multiple myeloma is more common in older patients.
Non-Hyperdiploid Multiple Myeloma
Non-hyperdiploid multiple myeloma represents approximately 40–50% of cases. This subtype can occur across a broader age range. It is often associated with chromosomal abnormalities instead of an increase in the number of chromosomes. Abnormalities include translocations or deletions rather than gains, like translocations of the IgH gene at 14q32, often with partner chromosomes such as 4p16 or 11q13.
It generally has a worse prognosis compared to hyperdiploid multiple myeloma since it is more rapidly spreading and often exhibits resistance to therapy. Non-hyperdiploid multiple myeloma needs closer monitoring. It benefits from newer, more aggressive treatments due to its higher risk of progression.3Ravindran Ankathil, Foong, E., Ismail Siti-Mariam, Ramli Norhidayah, Mohd Yunus Nazihah, Vijay Sangeetha, Hariharan, S., & Husin Azlan. (2021). Hyperdiploid Multiple Myeloma with Novel Complex Structural Chromosome Abnormalities Associated with Poor Prognosis : A Rare Case Report. International Journal of Hematology-Oncology and Stem Cell Research. https://doi.org/10.18502/ijhoscr.v15i3.6852
Stages of Multiple Myeloma
It is a progressive disease. It progresses through a series of stages as described:
MGUS or Monoclonal Gammopathy of Undetermined Significance
MGUS is a condition in which the hallmark of multiple myeloma, the myeloma protein, is present in the blood without causing any symptoms. This stage is relatively stable and affects about 5% of people aged 70 and above.
Most people with MGUS never develop multiple myeloma, but it can be an early precursor — it is known to progress to multiple myeloma at a rate of 0.5–1% per year.
Smoldering Multiple Myeloma
Smoldering multiple myeloma is the second stage in the progression of multiple myeloma. Even though it is asymptomatic, it is a more advanced stage than MGUS. It progresses to full-blown multiple myeloma at a rate of 10% per year within the first 5 years of development. After this particularly risky period, the risk of active multiple myeloma drops to about 3% per year for the next 5 years. Then, the risk further declines to around 1% per year.
Active Multiple Myeloma
Multiple myeloma is the active cancer stage. It is the most serious stage in the progression from MGUS and smoldering multiple myeloma.
Plasma Cell Leukemia
Almost 2-4% of multiple myeloma cases are complicated by plasma cell leukemia, which is a rare and aggressive form of blood. In plasma cell leukemia, malignant plasma cells proliferate so much that they circulate in the bloodstream. It’s often associated with poor prognosis.4Rajkumar, S. V. (2009). Multiple Myeloma. Current Problems in Cancer, 33(1), 7–64. https://doi.org/10.1016/j.currproblcancer.2009.01.001
Signs & Symptoms of Multiple Myeloma
The CRAB acronym represents the most common clinical presentation of multiple myeloma:
| Acronym | Signs and symptoms |
| C (for increased serum calcium levels) |
|
| R (for renal impairment) |
|
| A (for anemia) |
|
| B (for bone lesions) |
|
Other than these hallmark features, multiple myeloma patients also have generalized symptoms of malignancy, such as weight loss and night sweats.5Kyle, R. A., Gertz, M. A., Witzig, T. E., Lust, J. A., Lacy, M. Q., Dispenzieri, A., Fonseca, R., Rajkumar, S. V., Offord, J. R., Larson, D. R., Plevak, M. E., Therneau, T. M., & Greipp, P. R. (2003). Review of 1027 Patients With Newly Diagnosed Multiple Myeloma. Mayo Clinic Proceedings, 78(1), 21–33. https://doi.org/10.4065/78.1.21
How does Multiple Myeloma kill you?
This condition has a survival rate of around 57%. Since it is a blood cancer, cancerous cells, and abnormal blood,d strictures travel to all parts of your body and cause damage to your vital organs. Complications result in each organ system, with organs beginning to shut down, eventually plunging the body into irreversible multi-organ failure.
| Systems | Complications |
| Bones and muscle |
|
| Blood |
|
| Kidneys |
|
| Immunity |
|
| Heart and blood vessels |
|
| Hormones and metabolism |
|
| Gut |
|
| Brain and nerves |
|
How does Multiple Myeloma get diagnosed?
It can have a vague presentation, especially in its early stages. Various clinical and lab methods are used to diagnose it.
History & Exam
The first step in diagnosing this condition involves a thorough medical history and physical examination. Like other patients, you may present with symptoms such as unexplained bone pain, fatigue, infections, or weight loss. The doctor will inquire about all these problems.
In addition, they will perform a complete physical exam. This will reveal bone tenderness, enlarged lymph nodes, and signs of kidney problems.
Imaging
Once your doctor suspects you have multiple myeloma, they will order imaging and lab tests to further assess you. A variety of imaging modalities are used for this purpose:
- X-rays are used to detect the hallmark osteolytic bone lesions of multiple myeloma. These appear as punched-out, round, radiolucent zones on the radiographs.
- Whole-body low-dose CT or PET CT are even more sensitive for these lesions.
- MRI findings are much more accurate and find lesions that are often missed on traditional X-rays.
Lab Investigations
Many key lab tests are important in confirming the diagnosis of this condition. They also help doctors determine the severity of the disease and predict its outcomes for you. General tests include:
- Complete blood count
- Renal function tests
- Liver function tests
- Serum electrolytes
- Infectious disease panel
Similarly, a variety of specific tests are also performed to detect abnormal proteins in your blood and urine, such as:
- Beta-2 microglobulin and serum immunoglobulin levels
- Serum protein electrophoresis
- Serum immunofixation electrophoresis
- 24-hour proteinuria
- Serum-free light chain assay
Bone Marrow Biopsy
Bone marrow biopsy is the gold standard investigation for diagnosing this condition. A needle is used to draw out a liquid sample of bone marrow. This sample is examined under a microscope for abnormal plasma cells. In addition, once the diagnosis is confirmed, genetic testing such as plasma cell fluorescence in situ hybridization or FISH is performed to identify specific chromosomal abnormalities.7Tests for Multiple Myeloma. (2024). Cancer.org. https://www.cancer.org/cancer/types/multiple-myeloma/detection-diagnosis-staging/testing.html
How does Multiple Myeloma Get Treated?
It is treated with chemotherapeutic drugs and transplantation of stem cells. However, patients usually present with acute illness, which requires urgent stabilization.
Acute Management
To get you stable and ready for treatment, acute management of this condition focuses on fixing immediate issues.
- High calcium levels are treated with IV fluids to rehydrate and drugs like calcitonin or bisphosphonates, which lower body calcium.
- Renal involvement is managed by avoiding nephrotoxic medication, adjusting doses, consulting a kidney specialist, and, in severe cases, dialysis.
- Spinal cord or nerve compression caused by fractures or growths needs urgent surgery to relieve pressure and prevent permanent damage. Hyperviscose blood is treated with plasmapheresis to improve flow.
Chemotherapy
Once the urgent flareup is under control, chemotherapy is the next step. Drug choice depends on your risk category:
- High-risk patients often start with a combination of four drugs: daratumumab, bortezomib, lenalidomide, and dexamethasone.
- A simpler three-drug regimen will be used if you are a standard-risk patient.
- If a transplant is not an option, you might get these therapies for a longer time, followed by maintenance with meds like lenalidomide or daratumumab to keep the disease in check.
Transplant
A stem cell transplant is the most effective treatment for this condition. If you are eligible for a transplant, you will first go through a few months of chemo to shrink the cancer. Then, doctors will collect your stem cells, give you more high-dose chemo, and put the stem cells back in to help you recover. Afterward, you’ll stay on maintenance therapy to keep things under control and stop the disease from progressing.8Albagoush, S. A., Shumway, C., & Azevedo, A. M. (2023, January 30). Multiple Myeloma. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK534764/
What is Multiple Myeloma Prognosis by Age & by Stage?
The prognosis depends on various factors, including your age, the stage of the disease at diagnosis, genetic abnormalities, and your overall health. Younger individuals are usually diagnosed early and are mostly fit for novel treatments. Older individuals (over 65) usually have advanced disease and cannot tolerate aggressive treatments with lots of side effects. Similarly, the prognosis becomes poorer with increasing stages of this condition — the survival rate is 82% for stage I, 62% for stage II, and 40% for stage III.9Palumbo, A., Hervé Avet-Loiseau, Oliva, S., Lokhorst, H. M., Goldschmidt, H., Rosinol, L., Richardson, P., Caltagirone, S., Lahuerta, J. J., Thierry Facon, Bringhen, S., Gay, F., Attal, M., Passera, R., Spencer, A., Massimo Offidani, Kumar, S., Musto, P., Sagar Lonial, & Petrucci, M. T. (2015). Revised International Staging System for Multiple Myeloma: A Report From International Myeloma Working Group. Journal of Clinical Oncology, 33(26), 2863–2869. https://doi.org/10.1200/jco.2015.61.2267
Conclusion
Multiple myeloma is a severe blood cancer that is a result of abnormal proliferation of plasma cells. It presents with vague symptoms but is marked by increased blood calcium, kidney disease, anemia, and bone disease. Treatment includes chemotherapy, transplant, and management of complications. Survival rates can be poor or moderate depending on your overall health and the rate of disease progression if timely treatment is begun.
Refrences
- 1Ludwig, H., Durie, S. N., Meckl, A., Hinke, A., & Durie, B. (2020). Multiple Myeloma Incidence and Mortality Around the Globe; Interrelations Between Health Access and Quality, Economic Resources, and Patient Empowerment. The Oncologist, 25(9), e1406–e1413. https://doi.org/10.1634/theoncologist.2020-0141
- 2Prideaux, S. M., O’Brien, E. C., & Chevassut, T. J. (2014). The Genetic Architecture of Multiple Myeloma. Advances in Hematology, 2014, 1–16. https://doi.org/10.1155/2014/864058
- 3Ravindran Ankathil, Foong, E., Ismail Siti-Mariam, Ramli Norhidayah, Mohd Yunus Nazihah, Vijay Sangeetha, Hariharan, S., & Husin Azlan. (2021). Hyperdiploid Multiple Myeloma with Novel Complex Structural Chromosome Abnormalities Associated with Poor Prognosis : A Rare Case Report. International Journal of Hematology-Oncology and Stem Cell Research. https://doi.org/10.18502/ijhoscr.v15i3.6852
- 4Rajkumar, S. V. (2009). Multiple Myeloma. Current Problems in Cancer, 33(1), 7–64. https://doi.org/10.1016/j.currproblcancer.2009.01.001
- 5Kyle, R. A., Gertz, M. A., Witzig, T. E., Lust, J. A., Lacy, M. Q., Dispenzieri, A., Fonseca, R., Rajkumar, S. V., Offord, J. R., Larson, D. R., Plevak, M. E., Therneau, T. M., & Greipp, P. R. (2003). Review of 1027 Patients With Newly Diagnosed Multiple Myeloma. Mayo Clinic Proceedings, 78(1), 21–33. https://doi.org/10.4065/78.1.21
- 6Terpos, Kleber, M., Engelhardt, M., S. Zweegman, Gay, F., E. Kastritis, van, Bruno, B., Sezer, O., A. Broijl, S. Bringhen, M. Beksac, Larocca, A., Hajek, R., Musto, P., Johnsen, H. E., Morabito, F., Ludwig, H., Cavo, M., & H. Einsele. (2015). European Myeloma Network Guidelines for the Management of Multiple Myeloma-related Complications. Haematologica, 100(10), 1254–1266. https://doi.org/10.3324/haematol.2014.117176
- 7Tests for Multiple Myeloma. (2024). Cancer.org. https://www.cancer.org/cancer/types/multiple-myeloma/detection-diagnosis-staging/testing.html
- 8Albagoush, S. A., Shumway, C., & Azevedo, A. M. (2023, January 30). Multiple Myeloma. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK534764/
- 9Palumbo, A., Hervé Avet-Loiseau, Oliva, S., Lokhorst, H. M., Goldschmidt, H., Rosinol, L., Richardson, P., Caltagirone, S., Lahuerta, J. J., Thierry Facon, Bringhen, S., Gay, F., Attal, M., Passera, R., Spencer, A., Massimo Offidani, Kumar, S., Musto, P., Sagar Lonial, & Petrucci, M. T. (2015). Revised International Staging System for Multiple Myeloma: A Report From International Myeloma Working Group. Journal of Clinical Oncology, 33(26), 2863–2869. https://doi.org/10.1200/jco.2015.61.2267