Medulloblastoma is a rare but aggressive type of cancer. It is considered a brain cancer of childhood as it constitutes 20% of all cases of brain cancer in children.
What is Medulloblastoma?
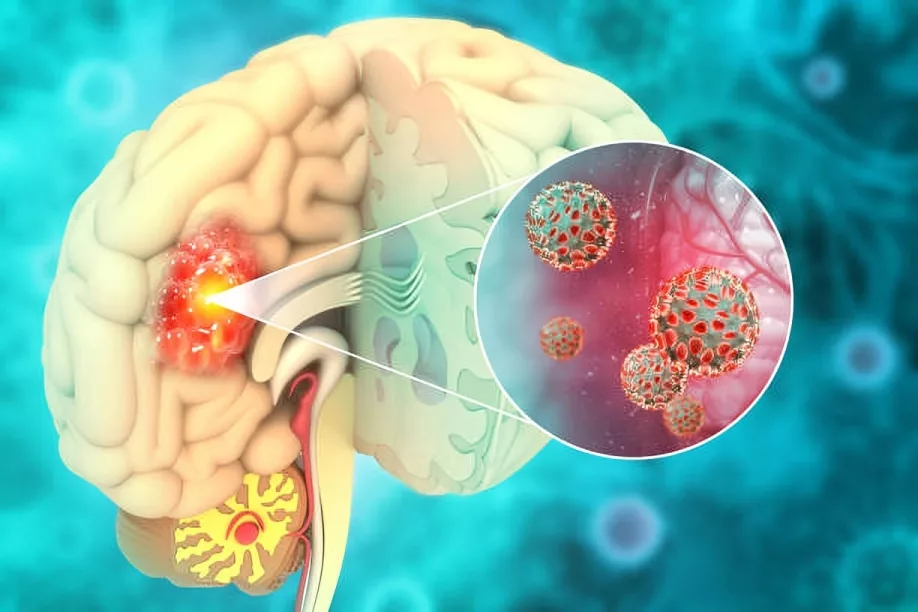
Medulloblastoma is a malignant tumor that develops in the brain, specifically in the cerebellum. The term medulloblastoma is a combination of “medulla” — referring to the medullary or lower portion of your brain where the cerebellum is located — and “blastoma” — a tumor made up of rapidly dividing young cells.
These are embryonal tumors that arise from leftover cells from early brain development. These cells are poorly differentiated and cannot mature into specialized brain tissue. Instead, they grow uncontrollably and form malignant tumors like medulloblastomas.1Medulloblastoma: Diagnosis and Treatment. (2024, August 20). Cancer.gov. https://www.cancer.gov/rare-brain-spine-tumor/tumors/medulloblastoma
How common is Medulloblastoma?
This cancer is a rare tumor, with approximately 6,000 people currently living with the condition worldwide. In the United States, around 435 new cases are diagnosed each year. Out of these, over 70% occur in children. It accounts for about 20% of all childhood brain tumors. The overall incidence in children is approximately 5 cases per million a year. Still, it is one of the most common brain cancers in children.
Most medulloblastoma cases are seen in children under the age of 10. The highest rates occur between those aged 1 to 4 and 5 to 9 years. It is more common in boys than girls and has a male-to-female ratio of 1.7:1.
In adults, this cancer is extremely rare. There is a reported incidence of only 0.05 cases per 100,000. 2Mahapatra, S., & Amsbaugh, M. J. (2023, June 26). Medulloblastoma. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK431069/
Causes of Medulloblastoma
Medulloblastoma is a result of rapid and unregulated growth of immature cells present in your brain. It begins in granule cell precursors in the developing cerebellum’s outer layer. It grows in the fourth ventricle of the brain until it fills the whole space. The tumor then spreads to nearby areas like the cerebellar vermis and brainstem.
In addition, this cancer can travel along the brain and spinal cord through the subarachnoid system. This phenomenon is called “drop mets” and is confined to the nervous system. Spread outside the nervous system is rare in children and only happens in about 7% of cases. When it happens, the most common sites of medulloblastoma are:
- Bone
- Lymph nodes
- Liver
- Lungs
These metastases typically develop around 20 months after surgery for medulloblastoma has already been performed, so survival after this spread is usually less than half a year.3Rochkind, S., Blatt, I., M Sadeh, & Goldhammer, Y. (1991). Extracranial metastases of medulloblastoma in adults: literature review. Journal of Neurology Neurosurgery & Psychiatry, 54(1), 80–86. https://doi.org/10.1136/jnnp.54.1.80
Risk Factors for Medulloblastoma:
Like other cancers, this can be triggered by a number of genetic and environmental factors:
- Inherited syndromes like Gorlin syndrome and Turcot syndrome increase the risk of medulloblastoma in children. These are linked to mutations in PTCH1 and APC genes.
- Mutations in genes like WNT, SHH, or TP53 disrupt normal cell growth and lead to tumors. Changes in chromosome 17p are also common in medulloblastoma.
- Radiation delivered to the head and neck during childhood is a major environmental risk factor. Exposure to certain chemicals or toxins is also under research as a cause of medulloblastoma.
- Prenatal factors like maternal medication use, infections, or exposure to toxins during pregnancy might increase the risk of medulloblastoma. In addition, childhood infections, e.g., cytomegalovirus and John Cunningham infections, have been noted in cases of the disease.
Stages of Medulloblastoma
Medulloblastoma is staged into standard-risk and high-risk tumors depending on various degrees of disease progression. It helps your doctors determine the best treatments according to possible outcomes.
Standard-Risk Medulloblastoma:
In standard-risk medulloblastoma, patients are typically over 3 years old. They have tumors that can be nearly or fully removed through surgery — leaving behind less than 1.5 cm² of residual tumor. These patients usually have no evidence of metastasis. The staging of metastasis in this group is typically classified as M0 because there is no spread of the tumor to other areas. These patients have an excellent prognosis. Their 5-year survival rate is over 80% when treated timely. In addition, standard-risk patients also respond well to the treatment protocols.
High-Risk Medulloblastoma:
High-risk medulloblastoma includes patients who are younger than 3 years old or those who have more advanced disease. These patients have complications such as incomplete tumor resection —over 1.5 cm² residual mass — or the cancer may have spread to other parts of the central nervous system. Metastasis in high-risk patients is further staged as follows:
- M1: the presence of tumor cells in the cerebrospinal fluid
- M2 spread within the intracranial sites beyond the primary tumor
- M3: spread to the spinal cord
- M4 spreads to organs outside the nervous system
These patients need more aggressive management. Even then, the 5-year survival rate for high-risk patients hovers between 50% and 70%, depending on factors like the extent of the disease and the response to treatment.4Orr, B. A. (2020). Pathology, diagnostics, and classification of medulloblastoma. Brain Pathology, 30(3), 664–678. https://doi.org/10.1111/bpa.12837
Genetic Classification of Medulloblastoma
Medulloblastoma is classified into four main molecular groups. As these groups are totally different from each other, differentiating between them is important in choosing the right treatment option for you. These groups include:
WNT-Activated Medulloblastoma
WNT-activated medulloblastoma patients have mutations in the CTNNB1 gene. This gene encodes for β-catenin, which is a protein involved in the WNT signaling pathway. This pathway regulates cell division and differentiation. WNT-activated medulloblastomas are located in the posterior fossa. Patients have 5-year survival rates reaching approximately 90%. Tumors are less likely to metastasize and rarely recur.
SHH-Activated Medulloblastoma
SHH-activated medulloblastomas are caused by abnormalities in the sonic hedgehog or SHH signaling pathway for cell proliferation. They are associated with mutations in genes like the PTCH1, SMO, SUFU, and TP53. This subgroup is further divided into two categories:
- SHH-activated medulloblastoma with mutations in TP53 is associated with a poor prognosis. The prognosis gets worse in older children and adults.
- SHH-activated medulloblastoma without mutations in TP53 can have more favorable outcomes.
Group 3 Medulloblastomas (Non-WNT Activated/ Non-SHH Activated)
Group 3 tumors are characterized by MYC overexpression — MYC is a well-known oncogene that causes abnormal cell proliferation. In addition, MYC overexpression also results in diminished cell death, which makes group 3 medulloblastomas highly aggressive, with poor prognosis. They mostly affect children under three and present with extensive metastasis at the time of diagnosis. They also have poor responses to treatments.
Group 4 Medulloblastomas (Non-WNT Activated/ Non-SHH Activated)
This subgroup is the most common yet still least understood. It is associated with chromosome 6p mutations. This group often presents with a high frequency of mutations in genes like DIP2B. It is less aggressive than Group 3 and more aggressive than WNT-activated and SHH-activated medulloblastoma. The prognosis is variable, and these tumors carry a moderate risk of recurrence and metastasis.5Molecular Genetics of Medulloblastoma in Children: Diagnostic, Therapeutic and Prognostic Implications. (2019). Future Neurology. https://doi.org/10.2217//fnl-2018-0030
Histological Types of Medulloblastoma
Experts have classified medulloblastomas into several types based on how they appear under a microscope. These subtypes differ in how they look, grow, and how they respond to treatment. Identifying what type of medulloblastoma you have helps doctors come up with the most suitable treatment plan for you.
Classic Medulloblastoma
This is the most common type, making up about 70% of cases. It has small, round cells accompanied by a high ratio of nucleus to cytoplasm. It is usually found in the middle of the cerebellum and is notorious for being aggressive and spreading fast. Treatment includes surgery, radiation, and chemotherapy.
Desmoplastic-Nodular (DN) Medulloblastoma
The DN subtype of medulloblastoma accounts for about 15% of all cases. Tumor cells occur in small clusters and are surrounded by a collagen-rich matrix. This tumor is less aggressive than classic medulloblastoma. Instead of the middle, it is usually found in the cerebellum’s sides. It often affects older children or adults and has better outcomes compared to classic medulloblastoma.
Large-Cell Anaplastic (LC/A) Medulloblastoma
The LC/A type makes up about 10% of cases of medulloblastoma. There are large cells with irregular shapes and a lot of cytoplasm. The cells divide rapidly, and they die off in large areas, resulting in considerable tissue damage. It is aggressive and often found in the cerebellar vermis. This type tends to spread to other body parts and is harder to treat. So it has poor survival rates.
Melanotic Medulloblastoma
This is a very rare form and forms less than 1% of cases. It contains a pigment called “melanin,” which makes it look dark. The tumor cells are similar to those in melanoma cancers, but it is still a form of medulloblastoma. It usually appears in the back of the brain in young children. Treatment is similar to other medulloblastomas.
Medullomyoblastoma
Another rare subtype, medullomyoblastomas, comprises about 1-5% of total medulloblastoma cases. They have both brain tumor cells and muscle-like cells. These tumors are often large and can spread to other areas. They are usually found in the cerebellum or sometimes outside of it. The prognosis is usually poor.6Orr, B. A. (2020). Pathology, diagnostics, and classification of medulloblastoma. Brain Pathology, 30(3), 664–678. https://doi.org/10.1111/bpa.12837
Signs & Symptoms of Medulloblastoma
- Clumsiness
- Gait disturbances
- Ataxia
- Early morning headaches that might improve throughout the day
- Nausea and vomiting
- Double or blurry vision.
- Cushing triad in severe cases.
- Hearing loss
- Facial weakness
- Head tilt
- Papilledema.
- Inability to abduct the eye
- Sun-setting sign (downward deviation of the eyes with visible sclera above the iris, caused by increased intracranial pressure due to tumor-induced hydrocephalus) and macrocephaly in infants
How is Medulloblastoma diagnosed?
Medulloblastoma is first suspected upon abnormal findings on neurological exam and imaging. It is confirmed through tissue biopsy, which is the gold standard in medulloblastoma diagnosis.
History & Physical Exam
A thorough history is required to help physicians determine whether or not you have medulloblastoma. They inquire about your symptoms, family history, and exposure to oral carcinogens before your birth or during your life. In addition, a thorough physical exam is also conducted, which includes the following:
- A thorough neurological examination points to a cerebellar tumor because of the presence of clear cerebellar signs. In addition, tests for cranial nerves can help identify palsies that cause double vision, facial weakness, and/or hearing loss. Such signs are an indication that the tumor has involved parts of the brain other than the cerebellum.
- Eye examination detects optic pallor or papilledema. This suggests an increased intracranial pressure due to tumor growth.
- The measurement of head circumference in infants helps identify macrocephaly (abnormally large head size), which may indicate swelling or pressure in the brain as a result of medulloblastoma.
- A general physical exam is also important for diagnosing severe cases. If intracranial pressure is high, the Cushing triad of hypertension, bradycardia, and irregular respirations can indicate severe brain herniation. It is a red flag that tells your doctor that you need immediate treatment.7Vinchon, & Leblond, P. (2019). Medulloblastoma: Clinical presentation. Neurochirurgie, 67(1), 23–27. https://doi.org/10.1016/j.neuchi.2019.04.006
Lab Tests
Routine lab tests for medulloblastoma evaluation include:
- Complete blood picture
- Thyroid profile
- Electrolytes panel
- Liver function tests
- Renal function tests
- Blood urea nitrogen
- Coagulation Profile
- Cerebrospinal fluid analysis (if lumbar puncture is performed to check leptomeningeal spread)
Imaging
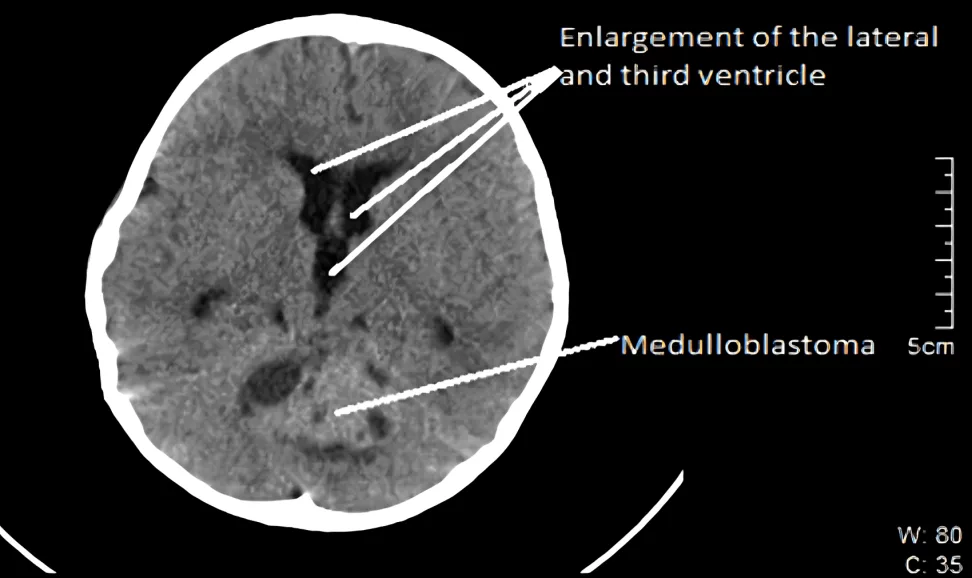
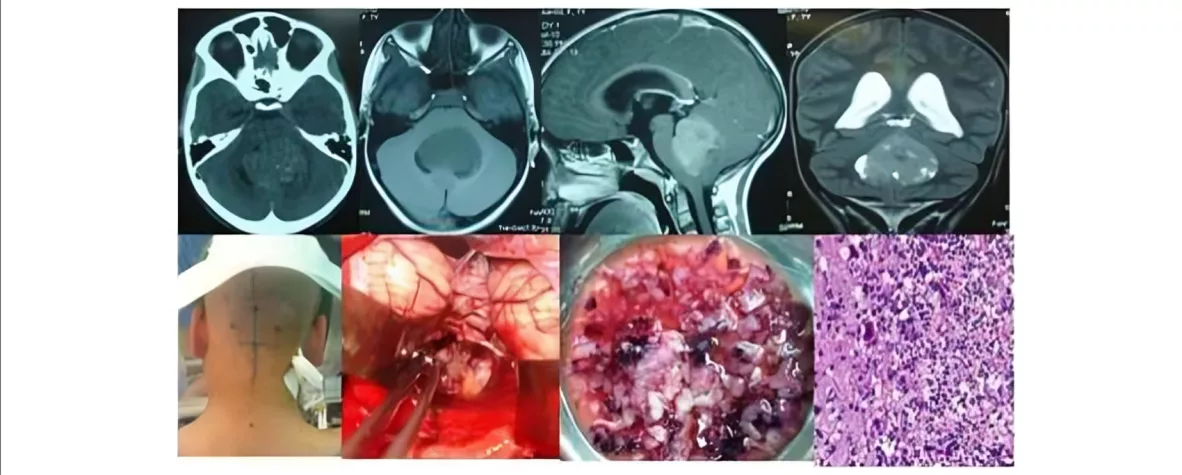
- A CT scan with contrast can reveal a mass in the fourth ventricle and detect hydrocephalus. Medulloblastomas are usually contrast-enhancing.
- MRI of the brain offers better anatomical detail than a CT scan and is crucial for detecting residual disease after surgery.
- A spinal MRI is used to check for metastasis along the spinal cord, which is common in medulloblastoma cases.
Tissue Biopsy
Once the presence of a tumor has been confirmed, a tissue biopsy is performed. Surgery is performed to remove a small fragment of the mass. Pathologists then carefully run tests to confirm whether the tumor is medulloblastoma or not. In addition, molecular and genetic testing is done to confirm the type of medulloblastoma you have.
Treatment for Medulloblastoma
There are several treatment options available for medulloblastoma. It is one of the cancers with a high cure rate when managed properly. Treatment typically involves a combination of different options, such as:
Medication
Chemotherapy with cisplatin and vincristine is common. Targeted therapies are being tested for specific subtypes. SMO inhibitors like vismodegib and sonidegib are used for the SHH subtype. WNT subtype patients may receive lower radiation doses. The non-SHH/WNT subtype is still being researched for treatment options.
Surgery
Surgery is the main treatment to remove medulloblastoma. Surgeons aim to remove as much of the cancer as safely possible. In cases with metastases, spinal surgery may be needed. Post-surgery monitoring is important for detecting any remaining disease.
Radiation Therapy
Radiation therapy is typically given after surgery to eliminate any remaining medulloblastoma cells. The radiations are most often directed at your brain and spinal cord to address potential spread. High doses can lead to long-term side effects like cognitive impairments and growth issues.
Palliative Care
Palliative care focuses on managing your symptoms if you have advanced medulloblastoma. It includes pain relief, nutrition support, and counseling. For end-of-life care, comfort and emotional support are the main goals.8Medulloblastoma. (2024, October 28). Hopkinsmedicine.org. https://www.hopkinsmedicine.org/health/conditions-and-diseases/brain-tumor/medulloblastoma
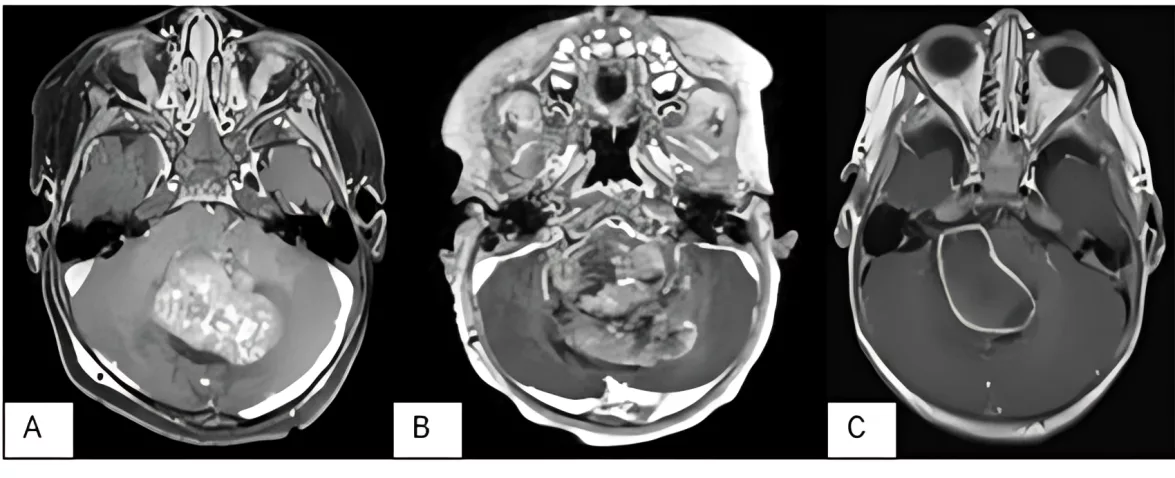
Image courtesy: Posterior Fossa Tumors in Infants: 13-year single-center retrospective review, Researchgate, 2023. Available at: Researchgate
How long does it take to recover from Medulloblastoma Treatment?
After treatment, lifestyle changes are essential. Survivors need regular check-ups for neurological issues and therapy for balance and memory. Hormone therapy may be necessary for growth hormone deficiencies.
Is Medulloblastoma Prognosis poor?
Cancer treatments have immensely improved the outcomes of medulloblastoma. Overall, the prognosis depends on factors like the tumor type and how much it has spread. Tumors of the WNT subgroup have a good prognosis, as over 90% of patients can survive five years or more. On the other hand, tumors that have metastasized have lower survival rates —around 50–70%. The rates further plummet if the patients are very young children.9Packer, R. J., & Vezina, G. (2008). Management of and Prognosis With Medulloblastoma. Archives of Neurology, 65(11), 1419–1419. https://doi.org/10.1001/archneur.65.11.1419
Medulloblastoma vs. Glioblastoma
Both medulloblastomas and glioblastomas are serious brain cancers. Medulloblastomas form in the cerebellum, whereas glioblastomas are tumors that grow from the glial cells, which are supportive cells of your nervous system.
| Medulloblastoma | Glioblastoma |
| Located in the cerebellum | Located in glial cells, mostly in the cerebral hemispheres. |
| Mostly affects children under 16 | Mostly affects adults over 45 |
| Symptoms include abnormalities in movement and headache | Symptoms include severe headaches, seizures, cognitive and behavioral problems |
| Better cure rate with treatment. | Poor prognosis with 1-1.5 year survival rate |
Conclusion
Medulloblastomas are brain tumors of the cerebellum. They mostly occur in children. Radiotherapy, chemotherapy, surgery, and palliative care are the treatment options for this condition, depending on the stage of the disease. Medulloblastomas have a high cure rate if diagnosed early and treated properly. However, a few subtypes can be aggressive and may reoccur after treatment.
Refrences
- 1Medulloblastoma: Diagnosis and Treatment. (2024, August 20). Cancer.gov. https://www.cancer.gov/rare-brain-spine-tumor/tumors/medulloblastoma
- 2Mahapatra, S., & Amsbaugh, M. J. (2023, June 26). Medulloblastoma. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK431069/
- 3Rochkind, S., Blatt, I., M Sadeh, & Goldhammer, Y. (1991). Extracranial metastases of medulloblastoma in adults: literature review. Journal of Neurology Neurosurgery & Psychiatry, 54(1), 80–86. https://doi.org/10.1136/jnnp.54.1.80
- 4Orr, B. A. (2020). Pathology, diagnostics, and classification of medulloblastoma. Brain Pathology, 30(3), 664–678. https://doi.org/10.1111/bpa.12837
- 5Molecular Genetics of Medulloblastoma in Children: Diagnostic, Therapeutic and Prognostic Implications. (2019). Future Neurology. https://doi.org/10.2217//fnl-2018-0030
- 6Orr, B. A. (2020). Pathology, diagnostics, and classification of medulloblastoma. Brain Pathology, 30(3), 664–678. https://doi.org/10.1111/bpa.12837
- 7Vinchon, & Leblond, P. (2019). Medulloblastoma: Clinical presentation. Neurochirurgie, 67(1), 23–27. https://doi.org/10.1016/j.neuchi.2019.04.006
- 8Medulloblastoma. (2024, October 28). Hopkinsmedicine.org. https://www.hopkinsmedicine.org/health/conditions-and-diseases/brain-tumor/medulloblastoma
- 9Packer, R. J., & Vezina, G. (2008). Management of and Prognosis With Medulloblastoma. Archives of Neurology, 65(11), 1419–1419. https://doi.org/10.1001/archneur.65.11.1419