Ocular melanoma, also known as intraocular melanoma, is a rare but aggressive eye cancer that originates from melanocytes, the pigment-producing cells of the eye. It is the most common primary eye cancer in adults, with an annual incidence of approximately 5–6 cases per million individuals. The condition is more prevalent in fair-skinned individuals and is most commonly reported in Europe and North America.1Wu, M., Yavuzyiğitoğlu, S., Brosens, E., Ramdas, W. D., Kiliç, E., & Rotterdam Ocular Melanoma Study Group. (2023). Worldwide incidence of ocular melanoma and correlation with pigmentation-related risk factors. Investigative Ophthalmology & Visual Science, 64(13), 45-45. The most common subtype of ocular melanoma is Uveal melanoma (constitutes around 80% of cases). Like skin melanomas, ocular melanomas are malignant (spread to other body parts). Therefore, timely treatment is important. The mainstay of the treatment is surgery. However, radiotherapy may also be employed.
Types Of Ocular Melanoma
Based on the anatomy, there are different types of ocular melanoma:
Uveal Melanoma:
This type of melanoma accounts for about 85% of the cases and is the most common type of ocular melanoma. The uvea is composed of different structures, thus, further classification of melanoma is as follows:
- Iris melanoma is a cancer of the colored part of the eye i.e., the iris.
- Ciliary body melanoma is a cancer of the ring of muscle fibers that control the shape of the lens i.e., the ciliary body which is present behind the iris.
- Choroid melanoma is a cancer of a thin sheet of tissue that contains blood vessels i.e., choroid. Choroidal melanoma is the most common.2Soliman, N., Mamdouh, D., & Elkordi, A. (2023). Choroidal melanoma: a mini-review. Medicines, 10(1), 11.
Since uveal melanoma is significantly more common than conjunctival melanoma, the terms ocular melanoma and uveal melanoma are often used interchangeably.
Conjunctival Melanoma:
Very rarely, cancer can affect melanocyte cells of the conjunctival membrane. Less than 10% of the malignant eye tumor cases present with conjunctival melanoma.
Ocular Melanoma Staging
Doctors usually use the TNM staging to stage ocular melanomas. In a cancer report, you will get the TNM stage mentioned. This determines the extent of treatment required.
Tumor:
Tx
No primary tumor assessed
T0
No evidence of a primary ocular tumor
T1
Tumor base ≤ 9mm and thickness is ≤ 6mm
The tumor base is 9.1-12mm with a thickness of ≤ 3mm
Based on slight differences, T1 is further subclassified into:
- T1a: T1 without ciliary body involvement and extraocular extension
- T1b: T1+ciliary body involvement
- T1c: T1+extraocular extension (≤5mm in diameter) but without ciliary involvement
- T1d: T1+extraocular extension (≤5mm in diameter) with ciliary body involvement
T2
The tumor base is ≤ 9mm and the thickness is 6.1-9mm
The base of the tumor is 9.1-12mm and the thickness is 3.1-9mm
The tumor base is 12.1-15mm and the thickness is ≤ 6mm
The base of the tumor is 15.1-18mm and the thickness is ≤ 3mm
- T2a: T2 + without ciliary body involvement and extraocular extension
- T2b: T2 + with ciliary body involvement
- T2c: T2 + extraocular extension (≤5mm in diameter) but without ciliary involvement
- T2d: T 2+ extraocular extension (≤5mm in diameter) with ciliary body involvement
T3
The tumor base is 3.1-9mm and the thickness is 9.1-12mm
The base of the tumor is 9.1-12mm and the thickness is 9.1-15mm
The tumor base is 12.1-15mm and the thickness is 6.1-15mm
The base of the tumor is 15.1-18mm and the thickness is 3.1-12mm
- T3a: T3+without ciliary body involvement and extraocular extension
- T3b: T3+with ciliary body involvement
- T3c: T3+extraocular extension (≤5mm in diameter) but without ciliary involvement
- T3d: T3+extraocular extension (≤5mm in diameter) with ciliary body involvement
T4
The tumor base is 12.1-15mm and the thickness is >15mm
The base of the tumor is 15.1-18mm and the thickness is >12mm
The tumor base is >18mm with any thickness
- T4a: T4+without ciliary body involvement and extraocular extension
- T4b: T4+with ciliary body involvement
- T4c: T4+extraocular extension (≤5mm in diameter) but without ciliary involvement
- T4d: T3+extraocular extension (≤5mm in diameter) with ciliary body involvement
- T4e: Any tumor size with extraocular extension >5mm
Node:
Nx: Regional lymph nodes can not be assessed
N0: No regional lymph node is involved
N1: Regional lymph nodes are involved or there are discrete tumor deposits in the orbit
- N1a: Metastasis is on one or more regional lymph nodes.
- N1b: There is no involvement of regional lymph nodes but there is a discrete tumor presence in the orbit (which is not contagious to the eye)
Metastasis:
M0: No distant metastasis is present
M1: Distant metastasis
- M1a: The largest diameter of the largest metastasis is ≤3 cm
- M1b: The maximum diameter of the largest metastasis is 3.1-8.0cm
- M1c: The largest diameter of the largest metastasis is ≥8.1cm
Ocular Melanoma Symptoms
In several cases, there are no symptoms or the symptoms are difficult to spot. When present, you can notice the following symptoms:
Blurred/Distorted Vision & Diplopia:
Numerous patients with melanoma report blurred vision. In a clinical case, the patient reported only blurred vision. Investigations by clinicians revealed primary ciliary melanoma with invasion of the iris. The study concluded that even very small ciliary melanomas can do fast local invasion and lead to blurred vision.3Costache, M., Patrascu, O. M., Adrian, D., Costache, D., Sajin, M., Ungureanu, E., & Simionescu, O. (2013). Ciliary body melanoma–a particularly rare type of ocular tumor. Case report and general considerations. Maedica, 8(4), 360. In another report of 25 diffuse iris melanoma cases, 52% of participants had blurred vision.4Demirci, H., Shields, C. L., Shields, J. A., Eagle Jr, R. C., & Honavar, S. G. (2002). Diffuse iris melanoma: a report of 25 cases. Ophthalmology, 109(8), 1553-1560. Several patients also complain of having dual vision (diplopia).
Eye Pain:
Cancers of the ciliary body and choroid can present with pain. Eye pain is not very common; as per a study, only 2% of melanoma patients experienced eye pain.5Kaliki, S., & Shields, C. L. (2017). Uveal melanoma: relatively rare but deadly cancer. Eye, 31(2), 241-257.
 However, another study concluded the percentage of eye pain to be 11.5% in patients with choroidal cancer.6Muradova, E., Hine, A. M., Falcone, M., Kels, J. M. G., & Weston, G. (2024). Malignancies with a tendency to metastasize to the eyelid or ocular structures. Clinics in Dermatology.
However, another study concluded the percentage of eye pain to be 11.5% in patients with choroidal cancer.6Muradova, E., Hine, A. M., Falcone, M., Kels, J. M. G., & Weston, G. (2024). Malignancies with a tendency to metastasize to the eyelid or ocular structures. Clinics in Dermatology.
Dark Spot & Floaters:
One of the common symptoms of eye cancer is dark spots in vision. Patients report floating shadowy specks with dark colors. These may be shaped like threads, webs, or just like a small dot.7Richards, Z., Nguyen, M. L., Kutteh, M., Ahmad, S., Henson, C., Firestone, B., … & Herman, T. D. L. F. (2022). Ocular malignancies treated with iodine-125 low dose rate (LDR) brachytherapy at a single high-volume institution: A retrospective review. Medical Dosimetry, 47(3), 273-279.
Reduced Field Of Vision:
The growth of ocular melanoma in the middle layers of the eye can interfere with or obstruct peripheral vision. Occasionally, iris melanomas lead to secondary glaucoma due to the seeding of melanoma in the trabecular meshwork. This chronic glaucoma can cause peripheral visual field loss.8Shields, C. L., Kels, J. G., & Shields, J. A. (2015). Melanoma of the eye: revealing hidden secrets, one at a time. Clinics in dermatology, 33(2), 183-196.
Flashing Lights (Photopsia):
According to a survey conducted by the Ocular Melanoma Foundation, a lot of patients see flashing lights as a symptom of eye melanoma. The phenomenon is usually an initial presentation and continues to increase with time.9Afshar, A. R., Deiner, M., Allen, G., & Damato, B. E. (2018). The patient’s experience of ocular melanoma in the US: a survey of the ocular melanoma Foundation. Ocular Oncology and Pathology, 4(5), 280-290.
Changes in Pupils:
Uveal melanoma is linked to changes in the color and the shape of pupils. Cancer of the melanocytes can bring about significant changes in eye color (due to abrupt production of pigments).
Eye Displacement (Within The Socket)
A few eye cancer patients also report displacement of the eye. Exophthalmos is the protrusion of the eyes from the orbit. It is an unusual symptom of uveal melanoma.10Grzegorczyk, A., Pachla, M., & Mazur, E. (2025). What should every doctor know about ocular melanoma?-review of literature. Journal of Education, Health and Sport, 77, 56890-56890.
Retinal Detachment
There have been reports of coexistence of retinal detachment and choroidal melanoma in patients which raises suspicion of melanoma being the cause of the detachment.11Pokawattana, N., Prasert, W., & Silpa-Archa, S. (2023). Coexistence of choroidal melanoma and rhegmatogenous retinal detachment: a case report and literature review. Annals of Medicine and Surgery, 85(11), 5709-5715. Retinal detachment is more significant in cases of large choroidal tumors.12Kivelä, T., Eskelin, S., Mäkitie, T., & Summanen, P. (2001). Exudative retinal detachment from malignant uveal melanoma: predictors and prognostic significance. Investigative ophthalmology & visual science, 42(9), 2085-2093.
Complete Loss Of Vision
Complete vision loss only occurs in advanced cases of eye melanoma. This occurs only when the tumors grow significantly large and damage the critical structures of the eye (macula, etc,). This can potentially lead to significant visual impairment and even vision loss. A complete loss of vision is mostly seen in long-standing melanomas.
Ocular Melanoma Causes
The exact cause of eye melanoma is unknown, however, experts believe abnormalities in the DNA of melanocytes lead to abnormal (uncontrolled) multiplication and formation of tumors.
Risk Factors:
Certain groups of individuals are at a greater risk of developing ocular melanoma:
Fair/Pale Skin
The skin houses a significant number of melanocytes. Fair-skinned people are more likely to fall prey to cutaneous melanomas. Astonishingly, multiple studies have found a link between fair or pale skin and ocular melanoma too.13Brănișteanu, D. E., Porumb-Andrese, E., Stărică, A., Munteanu, A. C., Toader, M. P., Zemba, M., … & Brănișteanu, D. C. (2023). Differences and similarities in epidemiology and risk factors for cutaneous and uveal melanoma. Medicina, 59(5), 943.
Family History
Though rarely, a family history of melanomas (cutaneous or ocular) serves as a novel risk factor for uveal melanomas.14Nisanova, A., Park, S. S., Amin, A., Zako, C., Wilson, M. D., Scholey, J., … & Mishra, K. K. (2024). Novel risk factors for uveal melanoma in adolescent and young adult patients: a comprehensive case-control analysis. Ophthalmology Science, 100687.
Light-Colored Eyes
Individuals with light-colored eyes are prone to developing eye melanoma. Grey, green, and blue eyes fall in the highest risk group while brown eyes have a moderate risk of intraocular melanoma. Studies suggest there are greater chances of ocular melanoma in people with a fair complexion and blue or green eyes.15Shields, C. L., Lally, S. E., Dalvin, L. A., Sagoo, M. S., Pellegrini, M., Kaliki, S., … & Blumenkranz, M. S. (2021). White paper on ophthalmic imaging for choroidal nevus identification and transformation into melanoma. Translational Vision Science & Technology, 10(2), 24-24.

Sunlight/UV Light Exposure
Some believe that exposure to sunlight (artificial sunlight tanning beds) can cause eye melanoma. There is a weak link between ultraviolet radiation (UVR) exposure and uveal melanoma.16Chalada, M., Ramlogan-Steel, C. A., Dhungel, B. P., Layton, C. J., & Steel, J. C. (2021). The impact of ultraviolet radiation on the etiology and development of uveal melanoma. Cancers, 13(7), 1700. As children/infants have thinner eye layers, experts suspect that the high rate of pediatric uveal melanoma is attributed to UV exposure.17Gallagher, R. P., & Lee, T. K. (2006). Adverse effects of ultraviolet radiation: a brief review. Progress in biophysics and molecular biology, 92(1), 119-131.Gallagher, R. P., & Lee, T. K. (2006). Adverse effects of ultraviolet radiation: a brief review. Progress in biophysics and molecular biology, 92(1), 119-131.
Inherited Skin Conditions
Individuals suffering from inherited dermal disorders like dysplastic nevus syndrome and moles are more likely to develop uveal melanoma. A nevus is a dark-colored growth in the eye commonly known as the “eye freckle”. People with melanocytic nevi are at a greater risk of developing ocular melanoma.
Old Age
Senile individuals are more prone to developing uveal
Ocular Melanoma Diagnosis
As most ocular melanomas are rare and asymptomatic, diagnosis is usually made during a routine eye checkup. Ophthalmologists opt for different types of tests and scans to diagnose ocular melanoma.
Eye Examination:
For an eye exam, your doctor will dilate your eye via special eye drops. This way the doctor can look into the structures of the eye.
Ultrasound:
An ultrasound aids in measuring the size of the ocular structures. Any abnormality in the size can correlate with tumorous growth. Your doctor will gently place a small probe on the eye surface after numbing it with anesthetic drops. Ultrasounds provide details about the size of the melanoma.
Fluorescein Angiography:
It is a study of the ocular vessels done via a special camera. Doctors inject a dye into your arm which is taken up by the blood vessels. The camera then takes pictures of the eye indicating any vascular blockage or leakage.
Fundus autofluorescence: Carried out with a special camera, this ophthalmic test highlights the areas of damage by turning them into small points of light in the photograph.
Optical Coherence Tomography (OCT):
An OCT is an imaging test that provides an extensively detailed picture of the inside of the eye (including cancerous masses).
After a comprehensive diagnosis of the condition, doctors perform the staging of the cancer to determine the size and extent of the cancer’s spread to other parts of the body.
Ocular Melanoma Treatment
Like with most cancers, the ideal treatment plan for ocular melanoma depends on multiple factors. The aspects that determine the type of treatment include:
- Size (and thickness)
- Location
- Spread of cancer (metastasis)
- Age
- Overall health (presence of co-morbidities, immune health, etc.)
Watchful Waiting:
If your tumor is asymptomatic and has a thickness of less than 2.5mm, you may not need immediate treatment. In such cases, eye doctors advise you to monitor the development of symptoms carefully. This period is called “watchful waiting”.
Radiation Therapy:
Powerful ionizing radiations are frequently used to kill the cancerous cells. Several patients prefer non-invasive procedures like radiation therapy. Based on the location and size of the carcinoma, your healthcare provider can opt for either internal or external radiation therapy:
Internal Radiation Therapy
In internal radiation therapy, the doctor implants a radiation source (a radioactive seed) inside the eye i.e., near the tumor. The most common type of radiation therapy is Plaque radiation therapy in which the doctor places a metal disk (plaque) directly on the wall of the eye. Made out of gold, the plaque resembles a bottle cap in shape. Professionals use temporary stitches to hold the seed in place for 4-5 days.
Research indicates that plaque brachytherapy is an effective treatment for uveal (especially choroidal) melanoma. It provides excellent control of localized/focal tumors and serves as a feasible alternative to enucleation (for medium-sized tumors). The treatment modality has good survival rates.18Thomas, G. N., Chou, I. L., & Gopal, L. (2024). Plaque Radiotherapy for Ocular Melanoma. Cancers, 16(19), 3386.
External Radiation Therapy
As the name indicates, the source delivers radiation from outside the body. Therapies like Proton beam radiation effectively target the eye tumor while being minimally damaging to the neighboring structures (eye and brain).
Surgery:
Surgeons can perform different types of surgeries for uveal melanoma:
External Resection
This involves removing the tumor and some of the neighboring tissues (healthy). It is indicated for small-sized tumors.
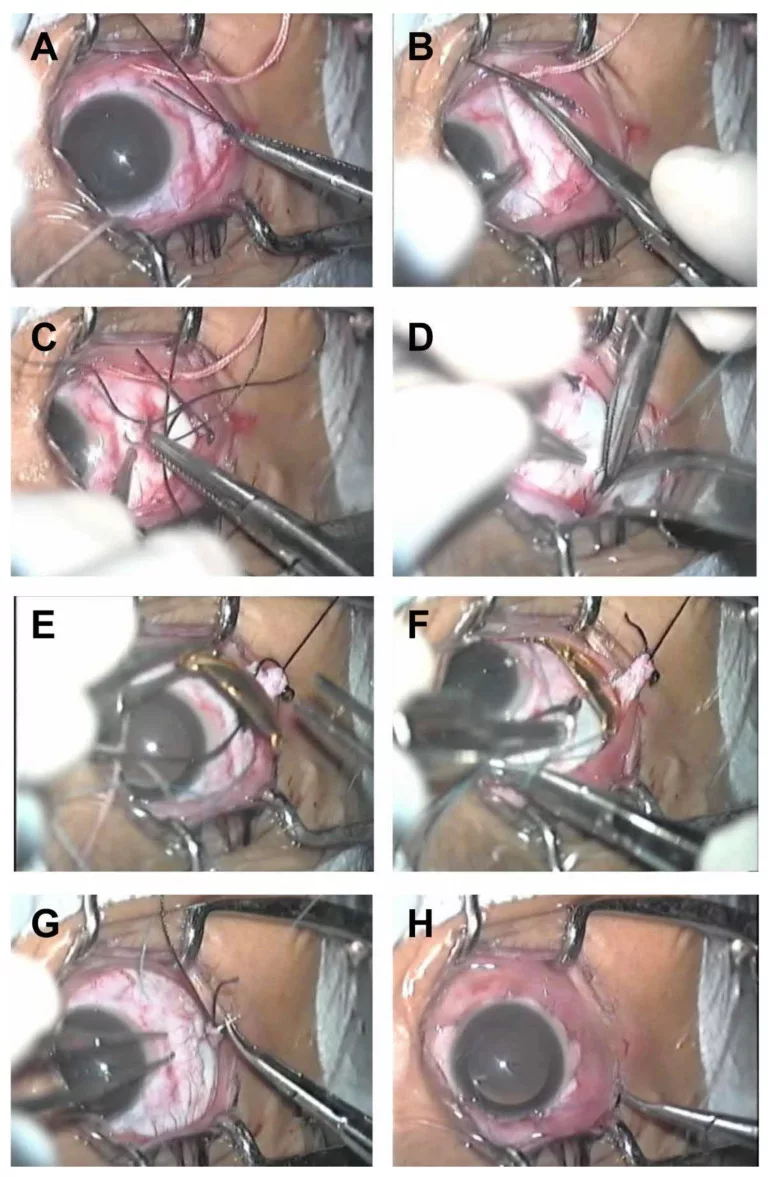
Enucleation
Doctors opt for enucleation i.e., complete removal of the eye in cases of large, painful tumors or tumors involving the optic nerve. After the removal of the eye, ophthalmologists replace the space with an artificial (prosthetic) eye.
Endoresection
In localized choroidal melanomas, doctors scoop out the part/area of the choroid affected by the tumor via a small incision. In this technique, the tumor is removed from within the eye, and the treatment type is effective for posteriorly localized uveal melanomas.19Vidoris, A. A., Maia, A., Lowen, M., Morales, M., Isenberg, J., Fernandes, B. F., & Belfort, R. N. (2017). Outcomes of primary endoresection for choroidal melanoma. International Journal of retina and vitreous, 3, 1-6.
Thermal Therapy:
Transpupillary thermal therapy utilizes lasers to generate heat. This directed heat aims to destroy eye tumors. Doctors deliver electromagnetic radiation via an infrared laser in a dilated eye.
Ocular Melanoma Prognosis
The prognosis of eye uveal melanoma relies heavily on the stage of cancer at the time of diagnosis/treatment. Localized tumors have a good prognosis and survival rates. However, the 5-year survival rate drops significantly in cases with metastasis (cancer spread).
Conclusion
Ocular melanoma is a rare eye cancer affecting pigment-producing melanocytes, most commonly in the uvea (uveal melanoma). It is often asymptomatic, but symptoms like eye pain, blurred vision, dark spots, and vision loss may occur. Genetic mutations in melanocytes contribute to its development, with risk factors including fair skin, light-colored eyes, family history, age, male sex, and UV exposure. Diagnosis relies on imaging techniques like OCT, ultrasound, and angiography. Treatment options include radiation therapy for small tumors and surgical removal or enucleation for larger ones. Prognosis is good for non-metastatic cases but poor if metastasis occurs, particularly to the liver.
Refrences
- 1Wu, M., Yavuzyiğitoğlu, S., Brosens, E., Ramdas, W. D., Kiliç, E., & Rotterdam Ocular Melanoma Study Group. (2023). Worldwide incidence of ocular melanoma and correlation with pigmentation-related risk factors. Investigative Ophthalmology & Visual Science, 64(13), 45-45.
- 2Soliman, N., Mamdouh, D., & Elkordi, A. (2023). Choroidal melanoma: a mini-review. Medicines, 10(1), 11.
- 3Costache, M., Patrascu, O. M., Adrian, D., Costache, D., Sajin, M., Ungureanu, E., & Simionescu, O. (2013). Ciliary body melanoma–a particularly rare type of ocular tumor. Case report and general considerations. Maedica, 8(4), 360.
- 4Demirci, H., Shields, C. L., Shields, J. A., Eagle Jr, R. C., & Honavar, S. G. (2002). Diffuse iris melanoma: a report of 25 cases. Ophthalmology, 109(8), 1553-1560.
- 5Kaliki, S., & Shields, C. L. (2017). Uveal melanoma: relatively rare but deadly cancer. Eye, 31(2), 241-257.
- 6Muradova, E., Hine, A. M., Falcone, M., Kels, J. M. G., & Weston, G. (2024). Malignancies with a tendency to metastasize to the eyelid or ocular structures. Clinics in Dermatology.
- 7Richards, Z., Nguyen, M. L., Kutteh, M., Ahmad, S., Henson, C., Firestone, B., … & Herman, T. D. L. F. (2022). Ocular malignancies treated with iodine-125 low dose rate (LDR) brachytherapy at a single high-volume institution: A retrospective review. Medical Dosimetry, 47(3), 273-279.
- 8Shields, C. L., Kels, J. G., & Shields, J. A. (2015). Melanoma of the eye: revealing hidden secrets, one at a time. Clinics in dermatology, 33(2), 183-196.
- 9Afshar, A. R., Deiner, M., Allen, G., & Damato, B. E. (2018). The patient’s experience of ocular melanoma in the US: a survey of the ocular melanoma Foundation. Ocular Oncology and Pathology, 4(5), 280-290.
- 10Grzegorczyk, A., Pachla, M., & Mazur, E. (2025). What should every doctor know about ocular melanoma?-review of literature. Journal of Education, Health and Sport, 77, 56890-56890.
- 11Pokawattana, N., Prasert, W., & Silpa-Archa, S. (2023). Coexistence of choroidal melanoma and rhegmatogenous retinal detachment: a case report and literature review. Annals of Medicine and Surgery, 85(11), 5709-5715.
- 12Kivelä, T., Eskelin, S., Mäkitie, T., & Summanen, P. (2001). Exudative retinal detachment from malignant uveal melanoma: predictors and prognostic significance. Investigative ophthalmology & visual science, 42(9), 2085-2093.
- 13Brănișteanu, D. E., Porumb-Andrese, E., Stărică, A., Munteanu, A. C., Toader, M. P., Zemba, M., … & Brănișteanu, D. C. (2023). Differences and similarities in epidemiology and risk factors for cutaneous and uveal melanoma. Medicina, 59(5), 943.
- 14Nisanova, A., Park, S. S., Amin, A., Zako, C., Wilson, M. D., Scholey, J., … & Mishra, K. K. (2024). Novel risk factors for uveal melanoma in adolescent and young adult patients: a comprehensive case-control analysis. Ophthalmology Science, 100687.
- 15Shields, C. L., Lally, S. E., Dalvin, L. A., Sagoo, M. S., Pellegrini, M., Kaliki, S., … & Blumenkranz, M. S. (2021). White paper on ophthalmic imaging for choroidal nevus identification and transformation into melanoma. Translational Vision Science & Technology, 10(2), 24-24.
- 16Chalada, M., Ramlogan-Steel, C. A., Dhungel, B. P., Layton, C. J., & Steel, J. C. (2021). The impact of ultraviolet radiation on the etiology and development of uveal melanoma. Cancers, 13(7), 1700.
- 17Gallagher, R. P., & Lee, T. K. (2006). Adverse effects of ultraviolet radiation: a brief review. Progress in biophysics and molecular biology, 92(1), 119-131.Gallagher, R. P., & Lee, T. K. (2006). Adverse effects of ultraviolet radiation: a brief review. Progress in biophysics and molecular biology, 92(1), 119-131.
- 18Thomas, G. N., Chou, I. L., & Gopal, L. (2024). Plaque Radiotherapy for Ocular Melanoma. Cancers, 16(19), 3386.
- 19Vidoris, A. A., Maia, A., Lowen, M., Morales, M., Isenberg, J., Fernandes, B. F., & Belfort, R. N. (2017). Outcomes of primary endoresection for choroidal melanoma. International Journal of retina and vitreous, 3, 1-6.

