A teratoma is a type of tumor that contains different types of body tissues. It forms from special cells that can grow into any structure—hair, teeth, muscle, or even bone. These tumors can appear in body parts like the tailbone, ovaries, or testes.
What is a Teratoma?
A teratoma is a tumor originating from germ cells— the precursor cells responsible for producing sperm or eggs. These germ cells are pluripotent, which means they differentiate into various tissues derived from all three germ layers:
- The ectoderm gives rise to tissues like skin, hair, and components of the nervous system
- Mesoderm forms connective tissues, muscles, bones, and blood vessels.
- Endoderm forms the epithelium which lines the gut and respiratory tracts, as well as glandular tissues.
Through combining these cells, teratomas can contain well-differentiated and fully developed structures. This diversity occurs because the germ cells retain their embryonic potential to differentiate into any tissue type found in your body. However, some serious teratomas may also contain poorly differentiated embryonic tissues.1NCI Dictionary of Cancer Terms. (2025). Cancer.gov. https://www.cancer.gov/publications/dictionaries/cancer-terms/def/teratoma
How does a Teratoma develop?
Teratomas result from abnormal differentiation of pluripotent cells present in the lining of your reproductive organs, called the germ layers. These cells form in the epiblast phase during embryonic development and then migrate to the ovaries and testes.
If these embryonic cells do not migrate properly, they can linger in out-of-place locations such as your abdomen, chest, or abdomen. Here, they can attach and continue to differentiate abnormally. As a result, they give rise to various tissues from the multiple germ layers—ectoderm, endoderm, and mesoderm.
Then, these cells persist in an undifferentiated state and do not specialize further in a normal pattern. There is no development of specialized organs; it is just a tumor, a lump of different types of tissues that leads to the development of a teratoma.2Ahmed, A., & Lotfollahzadeh, S. (2023, June 3). Cystic Teratoma. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK564325/
Causes of Teratoma
The formation of a teratoma is complex, and its causes are various and still under research. Some major causes and risk factors of teratomas are:
- Disruption of key signaling pathways of cell development causes teratomas. Abnormalities in the Notch, Wnt, and BMP pathways prevent germ cells from differentiating properly. As a result, teratomas contain cells that are not typically found at the site of origin.
- Transcription factors like OCT4, SOX2, and NANOG are responsible for maintaining pluripotency. Their unregulated overexpression causes germ cells to continue dividing and differentiate uncontrollably.
- Changes in DNA formation and metabolism patterns alter your genetic code and contribute to abnormal cell differentiation. As a result, your body does not destroy teratomas.
- Some conditions can put patients at risk due to genetic predisposition, such as:
o Down syndrome
o Pachyonychia congenita
o Beckwith-Wiedemann syndrome
o Ehlers-Danlos syndrome - Conditions of pregnancy,y such as maternal diabetes or exposure to toxic, ns can put your fetus at risk of teratomas in some studies.
- Exposure to certain environmental toxins or teratogenic substances during pregnancy may contribute to the abnormal development of germ cells, potentially increasing the risk of teratomas.3Surti, U., Hoffner, L., Chakravarti, A., & Ferrell, R. E. (1990). Genetics and biology of human ovarian teratomas. I. Cytogenetic analysis and mechanism of origin. American Journal of Human Genetics, 47(4), 635. https://pmc.ncbi.nlm.nih.gov/articles/PMC1683780/
Symptoms of Teratoma
Teratoma symptoms vary widely depending on the location of the tumor. Generalized symptoms usually arise because of the compression of nearby structures.
- Ovarian teratomas are the most common type of teratomas and cause symptoms like:
o Bloating
o Pelvic pain
o Increased estrogen
o Early puberty
o Menstrual irregularities
o Breast tenderness
o Nausea and vomiting
o Urinary incontinence - Testicular teratomas usually develop in one testicle and cause:
o Testicular mass
o Testicular pain
o Pubic heaviness
o Asymmetrical testicle swelling
o Hormonal imbalance - Sacrococcygeal teratomas are present at the base of the spine and are more common in newborns. Their symptoms are:
o Visible mass at the tailbone
o Lower back pain
o Weakness
o Numbness - Mediastinal teratomas are present in the central part of your chest and can cause various respiratory symptoms such as:
o Coughing
o Wheezing
o Difficulty breathing
o Shortness of breath
o Painful breathing
o Chest pain
o Chest heaviness - Abdominal teratomas can occur in various organs in the abdominal cavity and cause:
o Abdominal swelling
o Abdominal pain
o Digestive problems
o Loss of appetite - Cranial teratomas develop within your skull (mostly in your brain) and are extremely rare. They can cause headaches and focal symptoms depending on the part of brain they have affected.4Teratoma: Types, Symptoms & Treatment. (2021, November 24). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/22074-teratoma
Types of Teratoma
Teratomas are often classified on the basis of their composition and location; for example:
Mature Teratoma:
Mature teratomas consist of tissues that are well-developed. All three germ layers are visible. They have clearly differentiated masses of skin, hair, or teeth. They are usually benign and noninvasive. So, other than compressing tissues and causing secondary symptoms, they are not dangerous. Mature teratoma examples include:
Dermoid Cyst
A dermoid cyst teratoma or mature cystic teratoma is a common teratoma which occurs in:
- Ovaries (10-20% of all ovarian tumors are dermoid cysts)
- Testes
- The base of the spine
- Chest cavity
- Behind the abdominal cavity
- Brain
Most dermoid cysts are asymptomatic. When they are too large or too many, they can cause abdominal pain, swelling, or complications due to their size, like ovaries getting twisted, compressed, ruptured, or infected in less than <1% of the cases, and they can become cancerous.
Struma ovarii
Struma ovarii is a specialized type of teratoma that mainly consists of thyroid tissue instead of all three germ layers. It makes up about 3% of all ovarian teratomas. Most patients remain asymptomatic other than generalized abdominal discomfort and pain. However, sometimes, this thyroid tissue starts producing thyroid hormones and causes symptoms of hyperthyroidism.
Epignathus
Epignathus teratomas are huge teratomas of the face. They are located in your oral cavity, hard palate, or the base of your skull. They cause significant facial deformities, as well as symptoms such as:
- Airway obstruction
- Difficulty breathing
- Difficulty feeding in newborns.
- Polyhydramnios, if a fetus has it and is unable to take up amniotic fluid due to impaired swallowing.
Gliomatosis Peritoneii
Gliomatosis peritoneii tumors are a rare condition in which mature glial tissue spreads to the peritoneal surfaces that line the abdominal cavity. They occur when there is implantation of glial tissue (brain tissue derived from the ectoderm) after rupture or leakage of a teratoma, as well as from direct peritoneal spread.
These tumors usually occur in association with other teratomas, such as dermoid cysts and struma ovarii. Most cases are asymptomatic, but multiple tumors can cause abdominal swelling and discomfort.
Fetus in fetu teratomas are rare teratomas in which there is a “parasitic” teratoma twin.
Fetiform Teratoma (Teratoma Twin):
A fetiform teratoma is an extremely rare type of teratoma — only 1 in 5,00,000 is said to be affected by it. It is a highly differentiated tumor. Even though they lack vital organs because of the absence of proper organogenesis, fetiform teratomas are still so well-developed that they resemble fetuses. It usually occurs in the abdomen, chest, or back and is named accordingly.5Durning, V. (2017, May 19). What Is a Teratoma? Types, Causes, Symptoms, and More. WebMD. https://www.webmd.com/a-to-z-guides/what-is-teratoma
Immature Teratoma:
Unlike mature teratomas, immature teratomas are poorly differentiated and mostly composed of embryonic cells. They most commonly consist of neuroepithelium derived from the mesenchyme — an immature embryonic layer. They invade nearby tissues and have a high risk of cancer.
Immature Teratoma Grading
Immature teratomas are graded to determine their risk of spread, malignancy, and possible disease outcomes. They are graded according to the Norris system of tumor grading under x40 microscopic magnification:6Teratoma-immature. (2023). Pathologyoutlines.com. https://www.pathologyoutlines.com/topic/ovarytumorteratomaimmature.html
| Immature Teratoma Grade | Immature Teratoma Characteristics |
| Grade I Immature Teratoma | These are low-grade tumors with small amounts of well-differentiated tissue, which still have a degree of immaturity. Their prognosis is great if they can be removed completely by surgery and rarely reoccur. |
| Grade II Immature Teratoma | Grade II tumors are less differentiated than Grade I tumors. They also contain more amounts of abnormal tissue. They often need to be monitored after removal, and adjunct therapies are given if they recur. |
| Grade III Immature Teratoma | These teratomas are high-grade tumors. They need urgent, aggressive combination treatment in addition to surgery. Even then, their prognosis is uncertain, and tumors often recur. |
How is a Teratoma Diagnosis Established?
Teratomas are usually incidental findings. They are often asymptomatic until they are large enough to cause symptoms. They are usually discovered during surgery, especially among women undergoing C-sections, and doctors go straight to tests instead of an exam.
History & Physical Exam
Patients often visit doctors for generalized symptoms caused by large tumors compressing nearby organs. When you first visit your doctor, they will want to know your age and sex, as certain teratomas tend to occur more commonly in specific groups. Your doctor will ask if you’ve noticed lumps or swelling anywhere and if the lump is causing you any pain and discomfort.
Once your doctor has interviewed you, they will examine you for any visible or palpable lumps in the region where you are experiencing discomfort. Depending on where the teratoma is, they might tell you that it seems firm, fluid-filled, or does not move upon touch.
Lab Investigations
If your doctor suspects you might have a teratoma, they will order some routine blood tests as well as tests to check for tumor markers specific to different tumors.
- Complete blood count
- Liver function tests
- Renal function tests
- Serum electrolytes
- Infectious disease panel
- Alpha-fetoprotein/ AFP levels are markers for ovarian and sacrococcygeal teratomas
- Human chorionic gonadotropin/ hCG levels analysis for ovarian teratomas and testicular teratomas.
- Lactate dehydrogenase/LDH is an enzyme that determines if you have a rapidly growing, complicated teratoma
Imaging
Teratomas are easily detectable on different types of radiological imaging. For instance:
- Ultrasound scans are the first diagnostic imaging used to check for teratomas, especially ovarian teratomas. They appear as a mixture of echogenic/bright and anechoic/ dark areas due to their combination of different solid tissues and fluids.
- During X-ray scans, over 30% of teratomas have calcifications because of the presence of bone and tooth tissue. Large ones seem to change the position of nearby organs, and mediastinal teratomas can show a mediastinal shift.
- On CT, teratomas are well-circumscribed masses with a variety of tissue densities. They often have well-defined margins. Mature teratomas are often fatty and appear as hallmark areas of low-density CT. Irregular calcifications often indicate cancer.
- MRI scans can portray the soft tissue composition of teratomas more accurately than any other imaging. The presence of fat and fluid gets marked as hyperintense on T1 weighted MRI scans.
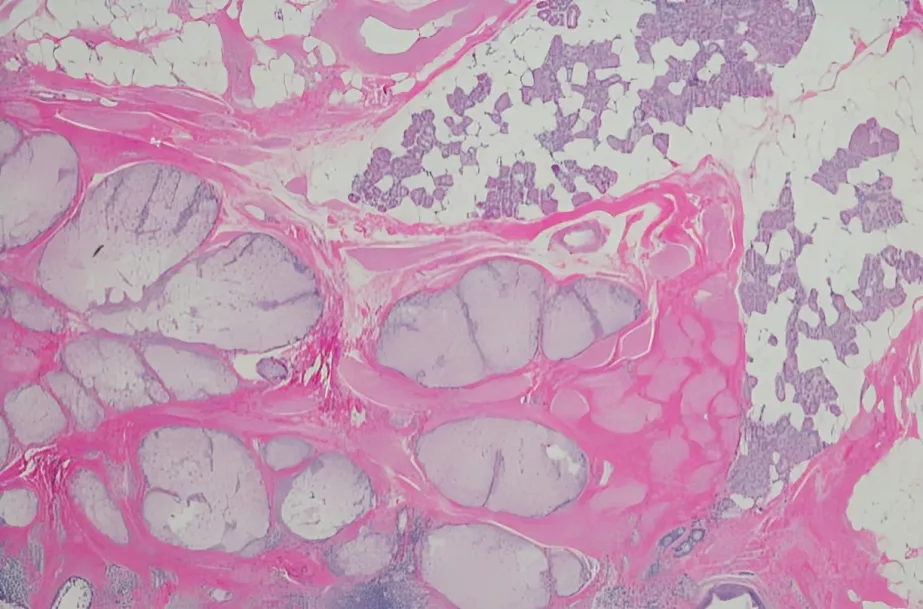
Tissue Biopsy
Once the presence of a teratoma has been confirmed, doctors take a small sample of tissue to perform a tissue biopsy. Tissue biopsies are the gold standard for teratoma diagnosis. Samples are taken surgically or through fine needle aspiration. They are observed under a microscope, analyzed by pathology experts, and analyzed genetically to confirm the type of teratoma you have.7Hamilton, C. A. (2024, October 28). Cystic Teratoma: Practice Essentials, Background, Pathophysiology. Medscape.com; Medscape. https://emedicine.medscape.com/article/281850-overview
Are there any Treatments available for Teratoma?
Teratomas are usually treated surgically. However, chemotherapy and radiation are often used to improve outcomes.
Surgery
Surgical excision is the first-line treatment for teratomas. For benign tumors, it has an excellent prognosis.
- High-grade ovarian tumors usually require the removal of ovaries and fallopian tubes.
- For the complete cure of testicular teratoma, the affected testis gets removed.
- Other forms of teratomas, like sacrococcygeal teratomas, are completely excised, too.
- Teratomas which are or carry the risk of cancer, require removal of nearby tissues. Surgeons also check nearby lymph nodes for cancer spread.
Chemotherapy
Chemotherapy is used for teratomas, which can recur, or those that are not completely managed with surgery. The BEP regimen, which consists of bleomycin, etoposide, and cisplatin, is often used. In addition, the VIP regimen (etoposide, ifosfamide, cisplatin) is also employed.
Radiation Therapy
Radiation is not a first-line treatment for teratomas. However, it is used to kill remaining abnormal cells after surgical tumor removal.
Monitoring
Teratomas are recurrent and require monitoring. This way doctors can find and treat them early. Monitoring is usually done via routine ultrasound scans and blood tests. Sometimes, MRI and CT scans are also used.8Mueller, D. K. (2024, October 28). Teratomas and Other Germ Cell Tumors of the Mediastinum Treatment & Management: Approach Considerations, Medical Therapy, Surgical Therapy. Medscape.com; Medscape. https://emedicine.medscape.com/article/427395-treatment
What is the survival rate for Teratoma?
Mature teratomas are not associated with mortality. However, a very small number of individuals pass away because of surgical complications each year. Immature teratomas have a survival rate of over 70-80%. Sacrococcygeal teratomas present before birth have survival rates of 54-77%.9Varlas, V. N., Cloțea, E. M., Varlas, R. G., Pop, A., Ovidiu Peneș, Dragoș Crețoiu, Dima, V., & Bălănescu, L. (2024). Immature Sacrococcygeal Teratoma: A Case Report and Extensive Review of the Literature. Diagnostics, 14(3), 246–246. https://doi.org/10.3390/diagnostics14030246
Dermoid Cyst vs Teratoma
Dermoid cysts are a subtype of teratoma that commonly affects the ovaries. They sometimes occur in the hair follicles and skin. They are mature teratomas, so they are benign and rarely cause cancer or serious symptoms. Teratomas have other types, too, which can be more dangerous and require urgent medical attention.
Conclusion
Teratomas are tumors derived from the germ cells of your reproductive organs. They contain tissues formed by all three germ layers — the endoderm, ectoderm, and mesoderm. Although they can be located anywhere in the body, they often occur in the ovaries. They are usually benign, though some can be cancerous. Teratomas are usually asymptomatic unless they grow too big and affect nearby organs. Treatment usually involves surgery. Cancerous teratomas require chemotherapy and radiation alongside surgery. Teratomas have a high recurrence rate and require monitoring. Despite that, the prognosis is usually favorable, especially for mature teratomas.
Refrences
- 1NCI Dictionary of Cancer Terms. (2025). Cancer.gov. https://www.cancer.gov/publications/dictionaries/cancer-terms/def/teratoma
- 2Ahmed, A., & Lotfollahzadeh, S. (2023, June 3). Cystic Teratoma. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK564325/
- 3Surti, U., Hoffner, L., Chakravarti, A., & Ferrell, R. E. (1990). Genetics and biology of human ovarian teratomas. I. Cytogenetic analysis and mechanism of origin. American Journal of Human Genetics, 47(4), 635. https://pmc.ncbi.nlm.nih.gov/articles/PMC1683780/
- 4Teratoma: Types, Symptoms & Treatment. (2021, November 24). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/22074-teratoma
- 5Durning, V. (2017, May 19). What Is a Teratoma? Types, Causes, Symptoms, and More. WebMD. https://www.webmd.com/a-to-z-guides/what-is-teratoma
- 6Teratoma-immature. (2023). Pathologyoutlines.com. https://www.pathologyoutlines.com/topic/ovarytumorteratomaimmature.html
- 7Hamilton, C. A. (2024, October 28). Cystic Teratoma: Practice Essentials, Background, Pathophysiology. Medscape.com; Medscape. https://emedicine.medscape.com/article/281850-overview
- 8Mueller, D. K. (2024, October 28). Teratomas and Other Germ Cell Tumors of the Mediastinum Treatment & Management: Approach Considerations, Medical Therapy, Surgical Therapy. Medscape.com; Medscape. https://emedicine.medscape.com/article/427395-treatment
- 9Varlas, V. N., Cloțea, E. M., Varlas, R. G., Pop, A., Ovidiu Peneș, Dragoș Crețoiu, Dima, V., & Bălănescu, L. (2024). Immature Sacrococcygeal Teratoma: A Case Report and Extensive Review of the Literature. Diagnostics, 14(3), 246–246. https://doi.org/10.3390/diagnostics14030246

