Orchiopexy is a surgical procedure in which the testicles that remain undescended during development are brought to their normal position (inside the scrotum). Most of the time, patients come with complaints of empty scrotal bags (hidden testes). This condition is known as cryptorchidism. Cryptorchidism is a condition when testes fail to descend into the scrotum.1Leslie, S. W., Sajjad, H., & Villanueva, C. A. (2023, June 5). Cryptorchidism. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK470270/
Cryptorchidism most commonly occurs in premature infants (30%) and can also occur in full-term infants (9%). In 80% of the cases, undescended testis migrates into the scrotum within 3-6 months of life. Cryptorchidism can be unilateral or bilateral. In 80% of the patients, the testes are palpable and are present along the inguinal canal. In 20 % of the cases, testicles are not palpable.2Prevalence and natural history of cryptorchidism. (1993, July 1). PubMed. https://pubmed.ncbi.nlm.nih.gov/8100060/
Types of Undescended Testes
There can be multiple types of undescended testes that your doctor will identify by physical examination, imaging, and laparoscopic intervention. There are two most common types of undescended testes:
- True undescended testes
- Ectopic undescended testes
True Undescended Testes:
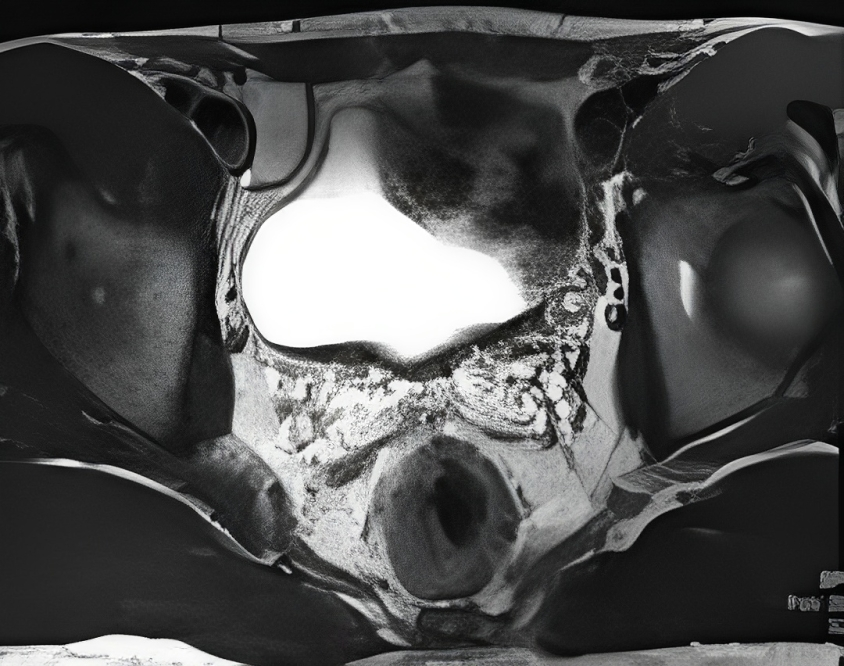
Testicles that are present along the pathway of the inguinal canal or along the natural descent pathway are called true undescended testes. These tests are located in the intra-abdominal, retroperitoneum (behind the peritoneum), inguinal canal, and superior aspect of the scrotum.
Ectopic Undescended Testes:
In this type of cryptorchidism, the undescended testes are not present along the natural migratory pathway. Ectopic undescended tests are located in the perineum, opposite side of the scrotum, and femoral canal.
In some cases, testes migrate into the scrotum but return back toward the inguinal canal; this is called an ascent of the testis. Moreover, in some patients, testes are retractable (they come inside the scrotum and then go back frequently). If the tests are absent on palpation and even after laparoscopy, this condition is known as vanishing testes syndrome.
Risk Factors of Cryptorchidism
Cryptorchidism is a multifactorial disease. The risk factors that increase the chance of cryptorchidism are the following:3Tseng, C. S., Chiang, I. N., Hong, C. H., Lu, Y. C., Hong, J. H., Chang, H. C., Huang, K. H., & Pu, Y. S. (2017). Advantage of early orchiopexy for undescended testis: Analysis of testicular growth percentage ratio in patients with unilateral undescended testicle. Scientific reports, 7(1), 17476. https://doi.org/10.1038/s41598-017-17825-w
- Low birth weight infants
- Premature infants
- Twin pregnancy
What Causes Cryptorchidism?
Cryptorchidism is an idiopathic disease. It means its exact cause is still unknown. However, this congenital defect can occur due to genetics, environmental factors, and maternal stress that influence the normal development of an infant in the prenatal period.
Normally, during development, the testes are inside the abdomen and migrate into the scrotum by passing through the inguinal canal via the gubernaculum before birth. Migration can be arrested anywhere along the path that causes undescended testes.
Indications & Contraindications of Orchiopexy
The indications of orchiopexy are:
- Unilateral or bilateral undescended testes that do not migrate into the scrotum after eight months of life
- Testicular torsion – It is a painful condition in which your testes become twisted, and your blood supply is compromised. It can occur in 1/4000 patients under the age of 30 years.
If the testes are atrophic, they are not suitable for performing orchiopexy.
At what age can your child have Orchiopexy?
In some infants, testicles migrate down to the scrotum after 6 to 8 months of age but if it remains undescended, your doctor will advise orchiopexy. It is preferable to perform surgery at 6 to 8 months of life. It is not advisable to delay surgery after 18 months of age as it can cause infertility. Moreover, surgery can preserve fertility and protect against testicular cancer.
The earlier the surgery is done, the more beneficial it will be for your child.4
Mohammad Alnoaiji, M. S., Alrashidi, T. N., Ghmaird, A. S., Alsalem, S. S., Alanazi, M. S., Albazei, A. I., Alenzi, M. O., Aljuhani, M. A., Alotaibi, R. S., Alanazi, S. A., Althomali, A. M., Almohammadi, A. M., & Alshahrani, E. H. (2019). Age at Surgery and Outcomes of Undescended Testes at King Salman Armed Forces Hospital, Tabuk, Saudi Arabia. Cureus, 11(12), e6413. https://doi.org/10.7759/cureus.6413
If you or your child has testicular torsion it is an emergency condition that should be treated as soon as possible to ensure the viability of the testes.
How to Prepare Your Child for Surgery?
Before surgery, you meet with your doctor, who will evaluate your child by taking his vitals (blood pressure, temperature, and pulse) and advising on some tests to check for any infection and hemoglobin level. After evaluation, your doctor will examine your child to palpate the tests and see other abnormalities. If your child is on medication, tell your doctor about the medication.
After that, you will be sent to an anesthesiologist along with your child to get anesthesia fitness. After getting fitness your doctor will give you the checklist for eating and drinking before surgery that you have to follow before the surgery. It includes:
- Stop giving solid food and non-clear fluids (juices) at midnight before surgery in children with ages greater than 12 months
- In children ages less than 12 months, you can give formula milk up to 6 hours before surgery and breastfeed him up to 4 hours before surgery
- To take medications, you can allow a sip of water
Follow these instructions should be strictly otherwise, your surgeon may call off your surgery.5Orchiopexy for testicle torsion: Before your surgery. (n.d.). https://myhealth.alberta.ca/Health/aftercareinformation/pages/conditions.aspx?hwid=abk8820
Procedure of Orchiopexy
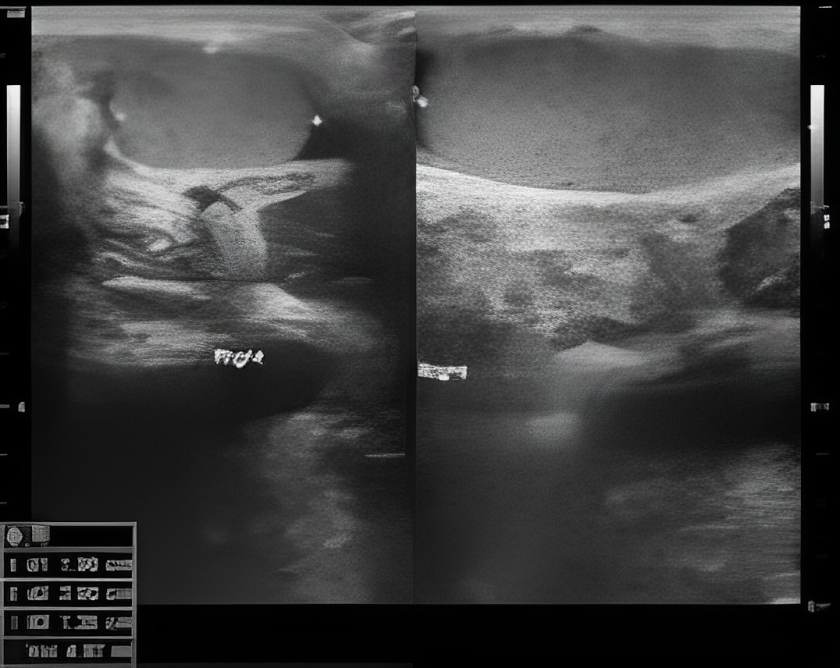
There are three methods to perform orchiopexy depending on the location of the testes. If the testes are not palpable, your doctor will advise laparoscopic orchiopexy. If the testes are retractable or present at the upper end of the scrotum, your surgeon will recommend the scrotal orchiopexy, If the testes are present in the inguinal canal, inguinal orchiopexy will be suitable for you.
Before surgery, an anesthesiologist will sedate your child to make a pain-free environment.
Laparoscopic Orchiopexy:
Your doctor will advise Laparoscopic orchiopexy when the testes are not palpable during physical examination. In this procedure, your doctor will make an abdominal approach with the help of two or three small holes, locate the testes, and check viability and vascularity. Afterward, he will create a pouch with the help of the incision in the scrotum, hang the testes, and fix it with the Dartous facial with the help of absorbable stitches.
Scrotal Orchiopexy:
During scrotal orchiopexy, your doctor will give an incision in the groin region and locate the testes. Avoid injury to the ileoinguinal nerve. After locating the testes, he will check the viability of the testes if the testicle is non-viable, he will remove it and replace it with a testicle prosthesis.6Taran, I., & Elder, J. S. (2006). Results of orchiopexy for the undescended testis. World journal of urology, 24(3), 231–239. https://doi.org/10.1007/s00345-006-0056-4
If the testes are viable (alive) your doctor makes another incision in the scrotal region to create a pouch known as a Dartous pouch that holds your child’s testicle. A grasping tool is then inserted up to the level of the groin that pulls the testes down into the Dartous pouch.
If there is a hernia or process vaginallis present during the operation they should be managed accordingly. In the end, your doctor closes the incision with dissolvable stitches.
Inguinal Orchiopexy:
In this procedure, the surgeon makes an incision in the inguinal area to access the undescended testes. After assessing the viability of the testes, the surgeon creates a small pouch in the scrotum to position the testes correctly. The testes are then secured using absorbable sutures to hold them in place.
The surgeon also makes a small incision in the scrotum, which is typically closed using absorbable stitches under the skin. In some cases, surgical glue may be used to close the incision. Steri-strips are placed over the incision to aid in healing and usually fall off within 7-10 days, typically when the patient starts bathing.
The bandage covering the incision can usually be removed 24 hours after the surgery. However, healing and care instructions may vary depending on the specific procedure and surgeon’s recommendations.7Elseth, A. (2023, August 8). Orchiopexy. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK560904/
Orchiopexy in Testicular Torsion
Testicular torsion needs emergency management to avoid devascularization of the testis. In this procedure, your surgeon makes an incision on the scrotum, untwists the spermatic cord, attaches it to the muscle to avoid future torsion, and checks its viability. If the testicle is non-viable, he will remove it and place a testicle prosthesis.
At-home care for your Child
Orchiopexy is a minimally invasive surgery. Your child can return home after the surgery as soon as he becomes stable. At home, you have to take care of your child according to the doctor’s instructions:
- Encourage his oral intake
- Keep him hydrated
- Keep his wound clean and dry
- Check his vital three times a day
- Give him pain medication to avoid pain
- Give him a soft diet to avoid constipation
- Don’t let him do strenuous activities like heavy weight lifting, doing exercises, or riding a bicycle for at least one month
- Your child should not go for swimming after the surgery for at least two weeks
- Do not soak the incision with water for 5 days after the surgery8Philadelphia, C. H. O. (n.d.). Undescended testicle surgery (Orchiopexy). Children’s Hospital of Philadelphia. https://www.chop.edu/treatments/surgery-undescended-testicles-orchiopex
Why is Orchiopexy Performed?
Orchiopexy is suitable in patients with undescended testes because if it remains untreated it causes infertility, cancer of the testicles, and testicular torsion. Seminoma is one of the most common testicular tumors that is caused by undescended testes.
Recovery time after Orchiopexy
Orcheopexy is not a major operation. It is a less invasive procedure with minimal hospital stay. Most of the child recover to their normal activities within 2-5 days after the procedure.
What are the Complications of Orchiopexy?
There are some complications that can occur during the procedure these are:
- Bleeding
- Infection can occur in both testes after bilateral orchiopexy, resulting in loss of the testes. Therefore, to avoid this complication, if the patient has bilateral undescended testes, then your doctor will perform a staged procedure. In this procedure, each testicle is treated separately with a gap of several months.
- Scarring or keloid formation
- Testicular atrophy
- ligation or revascularization of Vas deferens during the dissection
- Reascend of the testes (testes come out of the scrotum)
What is Normal after the Surgery?
Some signs are normal after the surgery, these are:
- Mild scrotal swelling that subsides gradually
- You can feel pain that may be relieved by taking medication and subside after some time
- Mild to moderate fever after the surgery
When to Consult your doctor after Orchiopexy?
Immediately call your doctor when you see the following problem in your child:
- A continuous high-grade fever not settling after taking medication
- Continues pain
- Persistent nausea and vomiting
- Bleeding from the surgical site
- Increase in scrotal swelling
- Change of color of the testes
Conclusion
To conclude, orchiopexy is a surgical procedure to descend the undescended testis to their normal position. Doctors usually advise this procedure when testes fail to descend in the scrotal sac after 8 months of life to prevent infertility. If your child has testicular pain or undescended testes, consult your doctor for evaluation, diagnosis, and management.
Refrences
- 1Leslie, S. W., Sajjad, H., & Villanueva, C. A. (2023, June 5). Cryptorchidism. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK470270/
- 2Prevalence and natural history of cryptorchidism. (1993, July 1). PubMed. https://pubmed.ncbi.nlm.nih.gov/8100060/
- 3Tseng, C. S., Chiang, I. N., Hong, C. H., Lu, Y. C., Hong, J. H., Chang, H. C., Huang, K. H., & Pu, Y. S. (2017). Advantage of early orchiopexy for undescended testis: Analysis of testicular growth percentage ratio in patients with unilateral undescended testicle. Scientific reports, 7(1), 17476. https://doi.org/10.1038/s41598-017-17825-w
- 4
Mohammad Alnoaiji, M. S., Alrashidi, T. N., Ghmaird, A. S., Alsalem, S. S., Alanazi, M. S., Albazei, A. I., Alenzi, M. O., Aljuhani, M. A., Alotaibi, R. S., Alanazi, S. A., Althomali, A. M., Almohammadi, A. M., & Alshahrani, E. H. (2019). Age at Surgery and Outcomes of Undescended Testes at King Salman Armed Forces Hospital, Tabuk, Saudi Arabia. Cureus, 11(12), e6413. https://doi.org/10.7759/cureus.6413 - 5Orchiopexy for testicle torsion: Before your surgery. (n.d.). https://myhealth.alberta.ca/Health/aftercareinformation/pages/conditions.aspx?hwid=abk8820
- 6Taran, I., & Elder, J. S. (2006). Results of orchiopexy for the undescended testis. World journal of urology, 24(3), 231–239. https://doi.org/10.1007/s00345-006-0056-4
- 7Elseth, A. (2023, August 8). Orchiopexy. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK560904/
- 8Philadelphia, C. H. O. (n.d.). Undescended testicle surgery (Orchiopexy). Children’s Hospital of Philadelphia. https://www.chop.edu/treatments/surgery-undescended-testicles-orchiopex





