Postural hypotension or orthostatic hypotension (OH) is a condition in which patients feel dizzy (or faint) when standing up from a sitting or supine position. This is attributed to a sudden drop in blood pressure, which induces syncope (fainting). Orthostatic means standing up, while hypotension means low blood pressure. Mostly, the condition develops transiently due to dehydration. However, it may present chronically due to some underlying serious health condition (like CNS lesion or cardiac dysfunction, etc.). The condition has a high risk of morbidity and mortality due to its association with frequent falls in senile patients. As per reports, 25% of patients visiting the ER for syncope are diagnosed with postural hypotension.1Palma, J. A., & Kaufmann, H. (2020). Management of orthostatic hypotension. CONTINUUM: Lifelong Learning in Neurology, 26(1), 154-177
OH incidence increases with age. The condition is pretty common in older adults, with a prevalence of over 22% in the older population.2Saedon, N. I. Z., Pin Tan, M., & Frith, J. (2020). The prevalence of orthostatic hypotension: a systematic review and meta-analysis. The Journals of Gerontology: Series A, 75(1), 117-122. Usually, doctors advise lifestyle changes and certain medications for orthostatic hypotension.
Orthostatic Hypotension Symptoms

Blurred Vision:
The transient drop in blood pressure can cause blurring or even loss of vision. Patients often report having a black out or a white out. Skin pallor and a loss of consciousness, though rarely, can accompany the vision loss.3Stewart, J. M., & Clarke, D. (2011). “He’s Dizzy when he Stands Up.” An Introduction to Initial orthostatic Hypotension. The Journal of pediatrics, 158(3), 499.
Nausea:
Several patients report being nauseous from the sudden BP drop. Generally, mental fogginess and heart palpitations are felt with nausea.4Wahba, A., Shibao, C. A., Muldowney, J. A., Peltier, A., Habermann, R., & Biaggioni, I. (2022). Management of orthostatic hypotension in the hospitalized patient: a narrative review. The American journal of medicine, 135(1), 24-31.
Headache:
Individuals with frequent episodes of hypotension may also experience mild to moderate headaches. Orthostatic headache is a type of headache that worsens on standing up and may be seen in children with orthostatic hypotension (due to postural tachycardia syndrome).5Go, S., Yamanaka, G., Kasuga, A., Kanou, K., Takamatsu, T., Takeshita, M., … & Kawashima, H. (2020). Orthostatic headache in children, including postural tachycardia syndrome and orthostatic hypotension: a near-infrared spectroscopy study. Journal of Clinical Medicine, 9(12), 4125.
Fatigue:
The cause of fatigue in OH patients is unclear, but it is reported by the vast majority. Many claim to have brain fog with fatigue and orthostatic syncope. The feelings of tiredness and fatigue negatively impact the patient’s quality of life.6Wu, R. E., Khan, F. M., Hockin, B. C., Lobban, T. C., Sanatani, S., & Claydon, V. E. (2022). Faintly tired: a systematic review of fatigue in patients with orthostatic syncope. Clinical Autonomic Research, 32(3), 185-203.
Palpitations:
The rapid fall in blood pressure can induce heart palpitations (a pounding heart). There have been cases where patients experienced loss of consciousness, fatigue, and palpitations following an episode of OH. 7Fedorowski, A., Ricci, F., Hamrefors, V., Sandau, K. E., Hwan Chung, T., Muldowney, J. A., … & Olshansky, B. (2022). Orthostatic hypotension: management of a complex, but common, medical problem. Circulation: Arrhythmia and Electrophysiology, 15(3), e010573. You may also feel short of breath during an episode of postural hypotension.
Muscle Pain:
Patients often experience a unique type of pain with OH, called the “coat hanger pain”. Experienced in the back of the neck and shoulders, the pain is so-called because its location in the body resembles a coat-hanger. Individuals complain of feeling a “charley horse,” i.e., sharp pain and muscle tightness in the region. According to a study by Khurrana and colleagues, coat hanger pain is present in about 60% of orthostatic hypotension patients.8Khurana, R. K. (2012). Coat-hanger ache in orthostatic hypotension. Cephalalgia, 32(10), 731-737. You may also experience lower back pain and associated muscle weakness.
Orthostatic Hypotension Causes
Based on the underlying causes, clinicians classify it as neurogenic and non-neurogenic.
Neurogenic Orthostatic Hypotension:
In the neurogenic subtype, there is inadequate regulation of blood pressure in response to changes in posture (when standing). Generally, nervous disorders are responsible for postural hypotension in young patients. Multiple nervous disorders can cause a neurogenic type of disease:
Autonomic Nervous System Dysfunction
Dysfunction of the sympathetic nervous system leads to improper coordination and consequent syncope/dizziness on standing. In the vast majority of cases, impairment of the baroreflex-mediated vasoconstriction of the skeletal muscles and splanchnic circulation leads to hypotension.9Freeman, R., Abuzinadah, A. R., Gibbons, C., Jones, P., Miglis, M. G., & Sinn, D. I. (2018). Orthostatic hypotension: JACC state-of-the-art review. Journal of the American College of Cardiology, 72(11), 1294-1309. Baroreceptors are specialized stretch receptors that detect blood pressure in the vessels. When these receptors dysfunction, there is a failure of the nervous system (mainly the sympathetic nervous system).
Parkinson’s Disease
Conditions like neurogenic orthostatic hypotension (nOH) and Parkinson’s disease co-exist in geriatric patients. Nervous deficits in older individuals can cause orthostatic syncope. The co-existence of nOH and Parkinson’s multiplies the risk of falls, serious injuries, and fractures in old patients.
Moreover, nOH in the elderly with neurodegenerative disorders is easily missed. Therefore, healthcare providers are advised to focus on approaches to recognize and prevent nOH.10LeWitt, P. A., Kymes, S., & Hauser, R. A. (2019). Parkinson disease and orthostatic hypotension in the elderly: recognition and management of risk factors for falls. Aging and disease, 11(3), 679. Other neurodegenerative diseases associated with nOH include Lewy body dementia, multiple system atrophy, etc.
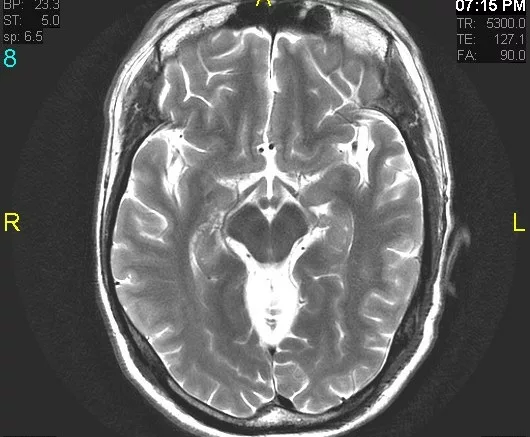
CNS Lesions & Neuropathies
Damage and lesions to the brain (central nervous system) can also cause malfunctioning of the autonomic system. Brainstem lesions, spinal cord lesions, and multiple system atrophy are causative factors for postural hypotension. Neuropathies caused by diabetes, auto-immune disorders, vitamin B12 deficiency, and kidney failure can also contribute to nOH.
Non-Neurogenic Orthostatic Hypotension:
The non-neurogenic type is usually the outcome of low blood volume, i.e., hypovolemia, and poor heart performance. It is commonly seen in older individuals. The following abnormalities are frequently associated with non-neurogenic orthostatic hypotension:
Dehydration
Acute orthostatic hypotension in senile individuals is mostly due to underlying dehydration. Therefore, fluid replacement therapy is administered to correct the condition.11Gupta, V., & Lipsitz, L. A. (2007). Orthostatic hypotension in the elderly: diagnosis and treatment. The American journal of medicine, 120(10), 841-847.
Anemia
OH with anemia requires special attention as it may be associated with grave consequences. There is limited evidence of anemia causing OH. However, experts believe that anemia can go alongside postural hypotension.
Hyperglycemia
Higher than normal blood glucose is seen in diabetics. Persistently raised glycemic levels tend to cause cardiac autonomic neuropathy (which ultimately leads to autonomic system dysfunction). It has been seen that, over time, patients develop episodes of severe glycemic dysregulation, which can eventually lead to orthostatic hypotension.12Pop-Busui, R. (2010). Cardiac autonomic neuropathy in diabetes: a clinical perspective. Diabetes care, 33(2), 434.
Hemorrhage
Studies have revealed a high prevalence of OH in patients suffering from hemorrhagic stroke during the acute stage. The condition disrupts the body’s normal compensatory mechanism (to regulate blood pressure) and contributes to hypovolemia. Therefore, doctors advise keeping stroke patients under monitoring until surgery is done.13Tam, P. K., Ramamurthy, G., Rawat, L., Huang, S., & Lim, J. H. (2024). Prevalence and Outcomes of Orthostatic Hypotension in Hemorrhagic Stroke Patients During Hospitalization. Neurology International, 16(6), 1878-1886.
Heart Defects
Different types of cardiovascular pathologies alter the heart’s ability to adequately pump blood (and respond to the physiological changes) on standing. In a normal individual, the heart compensates for the pooling of blood in the extremities, which occurs on standing. But in individuals with cardiac defects like atherosclerosis, heart failure, vessel stiffening, and arrhythmias, there is inadequate compensation and a sudden drop in blood pressure on standing.
Adrenal Insufficiency
Your adrenal glands produce hormones to regulate blood volume, blood pressure, and vascular tone. Insufficiency of the adrenal gland leads to aldosterone (mineralocorticoid) deficiency and cortisol (glucocorticoid) deficiency. Aldosterone hormone helps regulate blood volume, while cortisol plays a role in maintaining vascular tone. Therefore, adrenal insufficiency (mainly due to aldosterone deficiency) leads to orthostatic hypotension.
Medications
Several classes of medicinal drugs can impair the body’s ability to maintain blood pressure during posture changes. Antihypertensive medicines that alter the volume of blood (diuretics), change vessel tone (calcium channel blockers, nitrates), and lower the blood pressure (beta-blockers, ACE inhibitors) can cause hypotension.14Rivasi, G., Rafanelli, M., Mossello, E., Brignole, M., & Ungar, A. (2020). Drug-related orthostatic hypotension: beyond anti-hypertensive medications. Drugs & aging, 37, 725-738. Research shows that there is an increased risk of OH with prolonged usage of antipsychotic and antidepressant drugs (tricyclics).15Bhanu, C., Nimmons, D., Petersen, I., Orlu, M., Davis, D., Hussain, H., … & Walters, K. (2021). Drug-induced orthostatic hypotension: a systematic review and meta-analysis of randomised controlled trials. PLoS Medicine, 18(11), e1003821.
Orthostatic Hypotension Diagnosis
Doctors categorize the condition as orthostatic hypotension if there is a blood pressure drop of more than 20mm Hg of systolic blood pressure (SBP) or a diastolic BP drop of 10mm Hg within 3 minutes of standing.
Healthcare providers run multiple tests to diagnose orthostatic hypotension, including:
Tilt Table Test:
The patient lies flat on a tilt table while his/her vitals (mainly blood pressure) are monitored. The patient stays in the supine position for about 5 minutes. Then, the table is tilted so the patient is at a 60-degree angle. Health professionals diagnose the condition as OH if the SBP drops by at least 20mm Hg or the DBP drops by 10mm Hg in 3 minutes.

Doctors conduct several other tests to diagnose the underlying cause of the orthostatic syncope. Blood tests help diagnose comorbidities like anemia. An electrocardiogram (ECG) and an echocardiogram (echo) help check the heartbeat rhythm and pumping effectiveness, respectively. Nowadays, portable ECG devices (Holter monitors) can be used to measure heart rhythms. An exercise stress test may also be advised to measure the changes in heart rate during physical exertion.
Differential Diagnosis:
Orthostatic Hypotension Vs Postural Tachycardia Syndrome (POTS)
Both conditions are characterized by changes in the body on standing. However, in OH patients experience dizziness and fainting (due to blood pressure drop) on posture change, while POTS patients notice an increase in heart rate (rise of 30 bpm or more in 10 minutes of standing). In POTS, there is dizziness similar to OH, but there is no drop in blood pressure.
Types Of Body Responses
Clinicians have noted different types of bodily responses in orthostatic hypotension patients:

- Classic response: OH occurs within 3 minutes of standing.
- Delayed response: OH occurs after 3 minutes.
- Initial response: It lasts for less than 15 seconds after changes in posture.
- Delayed blood pressure recovery response: Blood pressure drop returns to the original value at a time longer than 15 seconds.
Most patients have classic orthostatic hypotension. Therefore, clinical literature only refers to the classic type as OH.
Orthostatic Hypotension Treatment
The treatment plan for orthostatic hypotension varies according to the underlying condition causing it. Mostly, OH develops secondary to some health issue; doctors aim to diagnose and fix the issue causing it.
Lifestyle Changes:
Simple steps can help improve the condition. For example, ample hydration is an important step in treatment because a number of cases arise due to dehydration. Individuals on bed rest should change posture (sit up) regularly to avoid OH. Wearing elastic stockings on the legs can alter the blood supply to the peripheries (on standing) and minimize the chances of postural hypotension. Some experts believe that abdominal compressions are more effective than lower extremity compressions.
Changing the dosage of medicines (antihypertensives and antidepressants) can also help reduce the risk of OH. Limiting alcohol intake can help. Strengthening muscles with exercise is also a good step.
Medicines:
Very rarely, health providers advise medications for orthostatic hypotension. When given, the main aim of these drugs is to increase the blood volume and/or pressure. The first line of treatment is to give fludrocortisone (expands intravascular volume) and midodrine hydrochloride (raises BP by constricting blood vessels). However, fludrocortisone is limited due to serious side effects (like heart failure, renal fibrosis, etc.) on prolonged usage.
Another pressor agent (like midodrine) used for OH management is droxidopa. It is safer than midodrine. However, midodrine is specifically indicated in cases of autonomic dysfunction. Other drugs used for treatment include erythropoiesis-stimulating agents, desmopressin (a diabetes insipidus drug), and octreotide. Pyridostigmine (an acetylcholinesterase inhibitor) is beneficial when used in combination with midodrine or atomoxetine.
Doctors treat the underlying issues like anemia, uncontrolled diabetes, cardiac problems, and adrenal insufficiency to correct orthostatic hypotension.
Final Word
Orthostatic hypotension is a condition in which the patient faints (or feels dizzy) on standing up. This happens due to a sudden drop in blood pressure (at least 20mm Hg in 3 minutes). The condition is frequent in older adults and occurs due to neurogenic and non-neurogenic causes. Autonomic nervous system failure and neurodegenerative disorders are major causes of neurogenic OH. Anemia, dehydration, cardiac defects, diabetes, adrenal insufficiency, and prolonged use of certain drugs (antidepressants, antihypertensives, etc.) contribute to non-neurogenic OH.
Symptoms are more pronounced in the morning, and most patients report vision blurriness, headaches, fatigue, and coat-hanger muscle pain during an episode of orthostatic syncope. A tilt table test helps diagnose the condition along with ECGs, echocardiograms, and exercise stress tests. Doctors usually treat the condition with hydration, lifestyle changes (compression stockings, limiting alcohol, etc.), medicine dose adjustment (of antihypertensives, etc.), and rarely with medicines. When prescribed, commonly used drugs include fludrocortisone, midodrine, droxidopa, and pyridostigmine.
Refrences
- 1Palma, J. A., & Kaufmann, H. (2020). Management of orthostatic hypotension. CONTINUUM: Lifelong Learning in Neurology, 26(1), 154-177
- 2Saedon, N. I. Z., Pin Tan, M., & Frith, J. (2020). The prevalence of orthostatic hypotension: a systematic review and meta-analysis. The Journals of Gerontology: Series A, 75(1), 117-122.
- 3Stewart, J. M., & Clarke, D. (2011). “He’s Dizzy when he Stands Up.” An Introduction to Initial orthostatic Hypotension. The Journal of pediatrics, 158(3), 499.
- 4Wahba, A., Shibao, C. A., Muldowney, J. A., Peltier, A., Habermann, R., & Biaggioni, I. (2022). Management of orthostatic hypotension in the hospitalized patient: a narrative review. The American journal of medicine, 135(1), 24-31.
- 5Go, S., Yamanaka, G., Kasuga, A., Kanou, K., Takamatsu, T., Takeshita, M., … & Kawashima, H. (2020). Orthostatic headache in children, including postural tachycardia syndrome and orthostatic hypotension: a near-infrared spectroscopy study. Journal of Clinical Medicine, 9(12), 4125.
- 6Wu, R. E., Khan, F. M., Hockin, B. C., Lobban, T. C., Sanatani, S., & Claydon, V. E. (2022). Faintly tired: a systematic review of fatigue in patients with orthostatic syncope. Clinical Autonomic Research, 32(3), 185-203.
- 7Fedorowski, A., Ricci, F., Hamrefors, V., Sandau, K. E., Hwan Chung, T., Muldowney, J. A., … & Olshansky, B. (2022). Orthostatic hypotension: management of a complex, but common, medical problem. Circulation: Arrhythmia and Electrophysiology, 15(3), e010573.
- 8Khurana, R. K. (2012). Coat-hanger ache in orthostatic hypotension. Cephalalgia, 32(10), 731-737.
- 9Freeman, R., Abuzinadah, A. R., Gibbons, C., Jones, P., Miglis, M. G., & Sinn, D. I. (2018). Orthostatic hypotension: JACC state-of-the-art review. Journal of the American College of Cardiology, 72(11), 1294-1309.
- 10LeWitt, P. A., Kymes, S., & Hauser, R. A. (2019). Parkinson disease and orthostatic hypotension in the elderly: recognition and management of risk factors for falls. Aging and disease, 11(3), 679.
- 11Gupta, V., & Lipsitz, L. A. (2007). Orthostatic hypotension in the elderly: diagnosis and treatment. The American journal of medicine, 120(10), 841-847.
- 12Pop-Busui, R. (2010). Cardiac autonomic neuropathy in diabetes: a clinical perspective. Diabetes care, 33(2), 434.
- 13Tam, P. K., Ramamurthy, G., Rawat, L., Huang, S., & Lim, J. H. (2024). Prevalence and Outcomes of Orthostatic Hypotension in Hemorrhagic Stroke Patients During Hospitalization. Neurology International, 16(6), 1878-1886.
- 14Rivasi, G., Rafanelli, M., Mossello, E., Brignole, M., & Ungar, A. (2020). Drug-related orthostatic hypotension: beyond anti-hypertensive medications. Drugs & aging, 37, 725-738.
- 15Bhanu, C., Nimmons, D., Petersen, I., Orlu, M., Davis, D., Hussain, H., … & Walters, K. (2021). Drug-induced orthostatic hypotension: a systematic review and meta-analysis of randomised controlled trials. PLoS Medicine, 18(11), e1003821.

