Addisonian crisis, or acute adrenal crisis, is a rare and potentially fatal condition where the adrenal glands don’t produce enough cortisol during stressful situations. This leads to symptoms like weakness, vomiting, diarrhea, dizziness, low blood pressure, and fainting. It occurs in people with Addison’s disease and requires immediate medical attention to prevent death. Treatment focuses on identifying the underlying adrenal insufficiency and resolving symptoms with IV fluids and glucocorticoids.1Rathbun, K. M., & Singhal, M. (2023). Addisonian Crisis. In StatPearls. StatPearls Publishing.
What is the Addisonian Crisis?
Addisonian crisis can occur when your adrenal glands that sit above each kidney don’t produce enough hormone called cortisol hormone for bodily function. Cortisol hormones play a role in regulating blood pressure, maintaining blood sugar levels and electrolytes, managing immune and bone health, and managing stress levels. People with Addison’s disease or damaged adrenal glands are unable to produce enough cortisol. Low cortisol levels can cause your body to show symptoms. You may not know you have Addison’s disease or adrenal insufficiency until you experience an Addisonian crisis. It can be triggered by physical stress, such as infection, surgery, or trauma, and requires urgent medical attention to prevent severe complications or death.
Addisonian crisis is a life-threatening event; if it is not managed timely, it can cause death.
What causes the Addisonian crisis?
The Addisonian crisis is an endocrine emergency that occurs due to acute adrenal insufficiency in the production of cortisol hormone, triggered by external or internal factors. Without early intervention, you may experience worsening health, potentially resulting in fatal conditions.2Elshimy, G., Chippa, V., Kaur, J., & Jeong, J. M. (2023). Adrenal Crisis. In StatPearls. StatPearls Publishing.
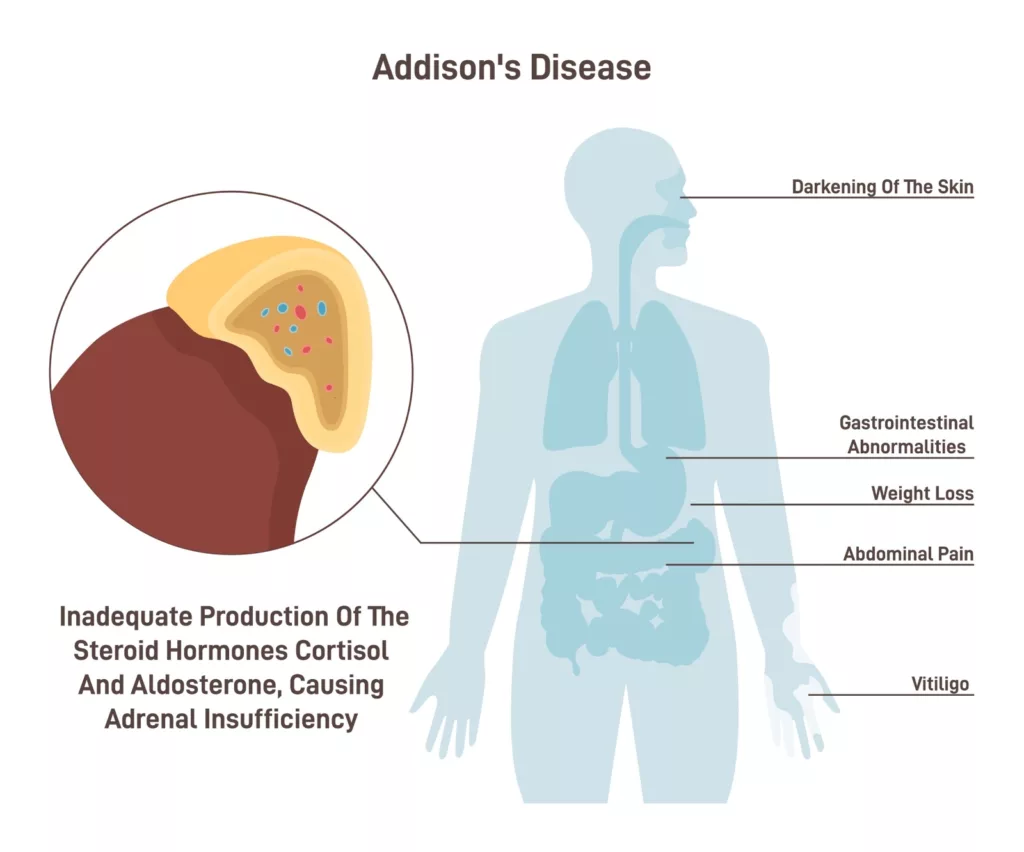
Adrenal glands are located above each kidney and play a crucial role in stress response. Adrenal insufficiency occurs when there is an absence or deficiency of adrenal hormones, mainly cortisol and aldosterone. Cortisol is responsible for glucose metabolism and the anti-inflammatory response, whereas aldosterone is responsible for maintaining body fluid and electrolyte balance. When the release of these hormones is suppressed or absent, there is a risk of developing an Addisonian crisis.
The Addisonian crisis occurs if you have adrenal insufficiency, either primary or secondary.
- Primary Adrenal Insufficiency (Addison’s Disease): This occurs due to damage or destruction of the adrenal glands, commonly caused by autoimmune reactions, infections (e.g., tuberculosis), adrenal hemorrhage, or surgical removal of the adrenal glands.
- Secondary Adrenal Insufficiency: This results from pituitary or hypothalamic dysfunction, which leads to decreased ACTH (adrenocorticotropic hormone) production, impairing cortisol synthesis. It can also occur due to abrupt withdrawal of long-term glucocorticoid therapy.
Stressful events, such as infections, trauma, or surgery, often precipitate an Addisonian crisis, as the body cannot mount an adequate hormonal response to these stressors.3Feeney, C., Buell, K. G., Avari, P., Buckley, A., Meeran, K., & Rees, D. A. (2018). Addisonian crisis: assessment and management. British journal of hospital medicine (London, England: 2005), 79(3), C34–C37. https://doi.org/10.12968/hmed.2018.79.3.C34
Symptoms of Acute Adrenal Crisis:
The prominent clinical features of Addisonian crisis are hypotension and hypovolemia, but the condition may also present with non-specific symptoms, including:4Dineen, R., Thompson, C. J., & Sherlock, M. (2019). Adrenal crisis: prevention and management in adult patients. Therapeutic advances in endocrinology and metabolism, 10, 2042018819848218. https://doi.org/10.1177/2042018819848218
- Lethargy (tiredness)
- Dizziness
- Loss of appetite
- Nausea
- Vomiting
- Abdominal pain
- Fever, chills
- Extremely Low blood pressure
- Low blood sugar level
- Altered mental state (confusion)
- Loss of consciousness
- Increased heart rate
- Hyperpigmentation of skin
Triggers for the Addisonian Crisis
Addisonian crisis can be triggered by factors including;
- A traumatic event that may lead to physical shock (accident)
- Extreme Dehydration
- Infections, including gastrointestinal infection
- Long-term use of steroids or abrupt stopping of steroids
- Emotional trauma
- Low blood sugar level
- Severe allergic reactions
- Thyrotoxicosis
- Strenuous physical activity
How is Addisionian Crisis Diagnosed?
The diagnosis of Addisonian crisis begins with a thorough assessment of medical history and symptoms. A detailed history helps identify signs of adrenal insufficiency, such as fatigue, dizziness, vomiting, and hypotension, particularly during stress or illness.5National Institute of Diabetes and Digestive and Kidney Diseases. (n.d.). Adrenal Insufficiency and Addison’s Disease: Diagnosis. Retrieved from [https://www.niddk.nih.gov/health-information/endocrine-diseases/adrenal-insufficiency-addisons-disease/diagnosis](https://www.niddk.nih.gov/health-information/endocrine-diseases/adrenal-insufficiency-addisons-disease/diagnosis)
Laboratory Tests
Several tests are critical for confirming the diagnosis:
- Adrenocorticotropic Hormone (ACTH) Test: This test evaluates the adrenal glands’ ability to respond to ACTH. A low cortisol level despite ACTH stimulation indicates adrenal insufficiency.
- Serum Cortisol Test: Correctly identifies cortisol deficiency; however, it’s more accurate if combined with an ACTH stimulation test.
- Serum Potassium and Sodium Tests: These tests are essential to detect electrolyte imbalances. Hyperkalemia (high potassium) and hyponatremia (low sodium) are common in adrenal crisis.
- Fasting Blood Glucose Test: Checks for hypoglycemia, a frequent feature of Addisonian crisis.
In addition, plasma renin activity is often measured to assess aldosterone function, as aldosterone deficiency is a component of primary adrenal insufficiency.
Imaging Studies
- CT Scan: Used to evaluate the adrenal glands for damage, such as atrophy, hemorrhage, or tumors.
- MRI: Assesses pituitary or hypothalamic abnormalities in cases of secondary adrenal insufficiency.
Treatment
Treatment for Addisonian crisis requires immediate intervention to prevent life-threatening complications. Delaying treatment can result in severe outcomes, including shock or death. Diagnosis should not delay the start of therapy, and an endocrinologist should be involved in managing the condition.
Intravenous (IV) glucocorticoid is the primary treatment. The first line for glucocorticoid replacement is a 100 mg bolus of hydrocortisone. If hydrocortisone is not available, dexamethasone is an alternative option. Oral glucocorticoids should not be administered because the patient is often too ill to eat or drink due to nausea and vomiting.
Continuous infusion of hydrocortisone is more effective than intermittent boluses, as it maintains cortisol levels within the therapeutic range. In addition to glucocorticoid therapy, intravenous rehydration is crucial. Over the first 12 to 24 hours, give two to three liters of normal saline or 5% dextrose in normal saline. This approach also helps treat hypoglycemia (low blood sugar levels).
Electrolyte imbalances, particularly hyperkalemia (high potassium levels) and hyponatremia (low sodium levels) are common in Addisonian crisis. IV fluids help address these imbalances. In severe hyperkalemia, additional interventions, such as calcium gluconate or insulin with glucose, may be necessary.
Once the patient shows signs of recovery from the adrenal crisis, gradually decreasing the steroid dose is recommended.6Wass, J. A., & Arlt, W. (2012). How to avoid precipitating an acute adrenal crisis. BMJ (Clinical research ed.), 345, e6333. https://doi.org/10.1136/bmj.e6333
Prognosis of the Addisonian Crisis
Prompt identification and immediate treatment of an Addisonian crisis lead to a good prognosis and recovery. However, individuals who are critically ill and have multiple comorbidities, such as diabetes, severe thyroid issues, and other health problems, may face higher risks of mortality and disability.
Complications of the Addisonian Crisis
If left untreated, an Addisonian crisis can lead to several severe complications, including;
- Cardiac arrhythmias: Abnormal heart rhythms due to electrolyte imbalances
- Cardiac arrest
- Hypotension: Low blood pressure may cause fainting
- Hypoglycemic shock: Extremely low blood sugar levels, potentially leading to coma
Prevention from Addisonian Crisis
People with Addison’s disease and their families should be educated on identifying signs of extreme stress that could trigger an adrenal crisis. In some cases, patients with Addison’s disease are advised to use emergency hydrocortisone injections or increase their oral steroid dosage during stressful situations.
Addisonian crisis vs. Addison’s disease
Addison’s disease, also known as primary adrenal insufficiency, is a chronic condition in which the adrenal glands fail to produce enough glucocorticoids (like cortisol) and mineralocorticoids (like aldosterone). It is most often caused by autoimmune adrenalitis but can also result from infections, tumors, or other factors. The diagnosis is made through blood tests showing low cortisol levels and elevated adrenocorticotropic hormone (ACTH). Treatment generally involves lifelong hormone replacement therapy with glucocorticoids and mineralocorticoids.7Michels, A., & Michels, N. (2014). Addison disease: early detection and treatment principles. American Family Physician, 89(7), 563–568.
An Addisonian crisis, on the other hand, is an acute, life-threatening event triggered by a significant stressor such as infection, surgery, or trauma. This crisis occurs when the body’s already insufficient adrenal glands can’t meet the heightened demand for cortisol, leading to symptoms like severe hypotension, hypoglycemia, and altered mental status. Immediate treatment, including intravenous glucocorticoids and fluid replacement, is critical to prevent fatal outcomes. Effective management of Addison’s disease can help prevent the onset of an Addisonian crisis.8Barthel, A., Benker, G., Berens, K., Diederich, S., Manfras, B., Gruber, M., Kanczkowski, W., Kline, G., Kamvissi-Lorenz, V., Hahner, S., Beuschlein, F., Brennand, A., Boehm, B. O., Torpy, D. J., & Bornstein, S. R. (2019). An Update on Addison’s Disease. Experimental and clinical endocrinology & diabetes: official journal, German Society of Endocrinology [and] German Diabetes Association, 127(2-03), 165–175. https://doi.org/10.1055/a-0804-27159Betterle, C., & Morlin, L. (2011). Autoimmune Addison’s disease. Endocrine development, 20, 161–172. https://doi.org/10.1159/000321239
Conclusion
An Addisonian crisis, also known as acute adrenal insufficiency, is a severe and potentially life-threatening condition that demands immediate diagnosis and treatment to reduce mortality. The primary risk factor for an Addisonian crisis is the presence of primary adrenal insufficiency or Addison’s disease. However, it can also occur in individuals with either diagnosed or undiagnosed Addison’s disease. Symptoms are nonspecific and may include low blood pressure, low blood sugar levels, nausea, vomiting, dizziness, and fainting. Treatment typically involves fluid and glucocorticoid replacement therapy. Educating patients and their families about identifying triggers and preventing future crises is essential for effective management.
Refrences
- 1Rathbun, K. M., & Singhal, M. (2023). Addisonian Crisis. In StatPearls. StatPearls Publishing.
- 2Elshimy, G., Chippa, V., Kaur, J., & Jeong, J. M. (2023). Adrenal Crisis. In StatPearls. StatPearls Publishing.
- 3Feeney, C., Buell, K. G., Avari, P., Buckley, A., Meeran, K., & Rees, D. A. (2018). Addisonian crisis: assessment and management. British journal of hospital medicine (London, England: 2005), 79(3), C34–C37. https://doi.org/10.12968/hmed.2018.79.3.C34
- 4Dineen, R., Thompson, C. J., & Sherlock, M. (2019). Adrenal crisis: prevention and management in adult patients. Therapeutic advances in endocrinology and metabolism, 10, 2042018819848218. https://doi.org/10.1177/2042018819848218
- 5National Institute of Diabetes and Digestive and Kidney Diseases. (n.d.). Adrenal Insufficiency and Addison’s Disease: Diagnosis. Retrieved from [https://www.niddk.nih.gov/health-information/endocrine-diseases/adrenal-insufficiency-addisons-disease/diagnosis](https://www.niddk.nih.gov/health-information/endocrine-diseases/adrenal-insufficiency-addisons-disease/diagnosis)
- 6Wass, J. A., & Arlt, W. (2012). How to avoid precipitating an acute adrenal crisis. BMJ (Clinical research ed.), 345, e6333. https://doi.org/10.1136/bmj.e6333
- 7Michels, A., & Michels, N. (2014). Addison disease: early detection and treatment principles. American Family Physician, 89(7), 563–568.
- 8Barthel, A., Benker, G., Berens, K., Diederich, S., Manfras, B., Gruber, M., Kanczkowski, W., Kline, G., Kamvissi-Lorenz, V., Hahner, S., Beuschlein, F., Brennand, A., Boehm, B. O., Torpy, D. J., & Bornstein, S. R. (2019). An Update on Addison’s Disease. Experimental and clinical endocrinology & diabetes: official journal, German Society of Endocrinology [and] German Diabetes Association, 127(2-03), 165–175. https://doi.org/10.1055/a-0804-2715
- 9Betterle, C., & Morlin, L. (2011). Autoimmune Addison’s disease. Endocrine development, 20, 161–172. https://doi.org/10.1159/000321239

