Palmar hyperhidrosis is a condition of excessive sweating in the palms of the hands and soles of the feet. Therefore, the layman’s term for this disease is sweaty palms. The condition arises due to overactivation of the sweat glands in the skin. Reports suggest that palmar hyperhidrosis affects only 3% of the world’s population. It equally affects men and women; however, there is a general misconception of women having a predominance.1Romero, F. R., Haddad, G. R., Miot, H. A., & Cataneo, D. C. (2016). Palmar hyperhidrosis: clinical, pathophysiological, diagnostic, and therapeutic aspects. Anais brasileiros de dermatologia, 91, 716-725.
Episodes of excessive sweating are notable even during early childhood. Thus, pediatric palmar hyperhidrosis may be severe enough to interfere with daily physical activities and school performance in adolescents and children. Etiologically, palmar hyperhidrosis can be either primary hyperhidrosis or secondary hyperhidrosis.
Primary palmar hyperhidrosis (also known as focal hyperhidrosis) arises from abnormalities in the eccrine sweat glands. It mostly develops during childhood/adolescence (known as pediatric palmar hyperhidrosis) and persists throughout life. On the other hand, secondary palmar hyperhidrosis develops secondary to some underlying medical conditions such as diabetes, hyperthyroidism, drug abuse, medicine usage, etc.
Hyperpalmar hidrosis may not seem like a significant health concern, but the disorder can lead to serious reductions in quality of life. This is partly because most patients do not seek treatment for the disorder. Thus, proper diagnosis and timely treatment are essential for physical and social well-being.
Acute Vs. Chronic Palmar Hyperhidrosis
Palmar hyperhidrosis (PH), which is part of hyperhidrosis (HH), can be acute or chronic. Acute palmar hyperhidrosis has a sudden onset but lasts only a short time. It typically develops due to an external trigger like stress or drug usage. The cause of acute palmar hyperhidrosis is the activation of the nervous supply (postganglionic nerves) of the eccrine gland.
On the contrary, chronic palmar hyperhidrosis stays in the body for a long time. Therefore, clinicians refer to the chronic type as the persistent/recurrent type. This very type is the result of an underlying comorbidity such as diabetes, thyroid issues, gene mutations, etc.
Palmar Hyperhidrosis Symptoms
Sweating is the body’s mechanism for responding to the increasing external temperature. Multiple receptors, the brain, and the sweat glands work together to thermoregulate the body. Increased outside heat or amped-up internal heat (due to hectic activity) is lost by releasing sweat from glands. But, in the case of palmar hyperhidrosis, sweating ensues even when no stimulus exists.
- Patients experience sweating in the palms of their hands or soles of their feet without any cause.
- Most patients report symmetrical and bilateral symptoms, i.e., A specific area on both sides of the body is involved (palms or soles).
- The palms are cold.
- The palms may change color and appear pale or blue. Pediatric patients usually have pink or white skin appearance during excessive sweating.
- The skin may become scaly and appear cracked in severe, chronic cases.
- Children often have trouble holding a pen/pencil as they continually try to keep the school papers/notebooks dry.
- In some cases, the onset of sweating is linked to emotional stress. However, in other cases, no such link is seen.
- A greater intensity of sweating is seen on the finger and palms region. But the posterior part of the hand is spared and there is less sweating.
- In severe cases, the sweat droplets combine to cover the entire hand and start to drip.
- Several patients also report swelling of the fingers during a hyperhidrosis episode.
- Bacterial/yeast infection of the recurrent sweaty skin leads to bad odor and consequent social embarrassment.
- Profuse sweating tends to affect electronic equipment and ruins clothes.
- Palmar hyperhidrosis has a grave psychosocial impact and leads to significant embarrassment and shame in the sufferers.2Laje, P. (2022). Palmar Hyperhidrosis. In Fundamentals of Pediatric Surgery (pp. 415-420). Cham: Springer International Publishing.
Palmar Hyperhidrosis Causes
Sweaty palms are the outcome of a wide array of issues:
Emotional Disturbance
The most common trigger for acute palmar hyperhidrosis is stress. Other emotional feelings, such as embarrassment, fear, and anxiety, also contribute to excessive perspiration. Thus, palmar HH is frequently seen in anxiety and psychosocial disorder patients.3Hsu, V. M., Shah, V. V., Aldahan, A. S., Mlacker, S., Samarkandy, S., & Nouri, K. (2017). Hyperhidrosis and stress. Stress and Skin Disorders: Basic and Clinical Aspects, 137-148. This abnormal release of sweat is attributed to the quick release of acetylcholine in the blood. Acetylcholine overexcites the postganglionic nerves of the gland, thereby inducing sweating. Many individuals notice transient palmar sweating when fainting, i.e., vasovagal syncope.
Neurological Disorder
Patients suffering from neurological disorders tend to develop secondary palmar hyperhidrosis. Sweating abnormalities like palmar hyperhidrosis are present in 5.5-12.9% of Parkinson’s disease (PD) patients.4Leta, V., van Wamelen, D. J., Rukavina, K., Jaakkola, E., Sportelli, C., Wan, Y. M., … & Chaudhuri, K. R. (2019). Sweating and other thermoregulatory abnormalities in Parkinson’s disease: A review. Annals of Movement Disorders, 2(2), 39-47.Individuals in the later stage of disease have a higher prevalence of hyperhidrosis. Other neurological abnormalities that can lead to hyperhidrosis include hypothalamic hyperhidrosis (overactive thermoregulation), vasovagal syndrome, spinal cord injury, and stroke.
Family History
Primary palmar hyperhidrosis has a genetic predisposition and runs within the families. Researchers identify alterations in gene loci on chromosomes 2, 14 and 16. Thus, many believe that the disease is polygenically inherited (inherited via multiple genes).5Henning, M. A., Pedersen, O. B., & Jemec, G. B. (2019). Genetic disposition to primary hyperhidrosis: a review of the literature. Archives of dermatological research, 311(10), 735-740.
Hormonal Imbalance
Certain endocrine disorders promote overproduction of the neurotransmitter acetylcholine, leading to eccrine gland overactivation.6Almohideb, M., Aljihani, M., Bukhari, M., Algethami, B., Asiri, O., & Alnamlah, A. (2021). The Impact of Hyperhidrosis on Patients’ Quality of Life and Daily Activities. International Journal of Pharmaceutical Research And Allied Sciences, 10(2-2021), 77-83. Underlying comorbidities that induce hormone dysregulation and consequent secondary palmar hyperhidrosis include:
- Diabetes
- Hyperthyroidism (overactive thyroid deranges thermoregulation and promotes excessive sweating throughout the body)7Misra, M. (2021). Excessive Sweating and Heat Intolerance. Endocrine Conditions in Pediatrics: A Practical Guide, 139-141.
- Hypopituitarism
- Acromegaly
- Pregnancy
- Menopause
Medicines
A variety of drugs can trigger excessive palm sweating. The list of medicines that can induce palmar hyperhidrosis includes:8Romero, F. R., Haddad, G. R., Miot, H. A., & Cataneo, D. C. (2016). Palmar hyperhidrosis: clinical, pathophysiological, diagnostic, and therapeutic aspects. Anais brasileiros de dermatologia, 91, 716-725.
- NSAIDs (naproxen, celecoxib, etc.)
- Opioids
- Doxepin
- Amitriptyline
- Insulin
- Venlafaxine
- Fluoxetine
Drug Abuse
Many drug addicts suffer from persistent sweaty palms. Substance abuse and alcoholism lead to vasodilation (widening of the blood vessels) in the skin. Blood vessel dilation paired with increased heart rate amps up sweating.
Topical Products
Skin products can rarely cause hyperhidrosis. However, newer formulations may contribute to unexplained, excessive sweating of the palms. Per a case report, a 41-year-old female reported “reactive hyperhidrosis” after applying moisturizers and hand sanitizers. She reported severe palm sweating after using a hand sanitizer containing 62% ethyl alcohol.9Oulee, A., Mendoza, R., & Nguyen, E. (2024). Reactive Hyperhidrosis Induced by Topical Products. The Journal of Clinical and Aesthetic Dermatology, 17(1), 6.

Tumors/Neoplasms
Sometimes, benign growths can stimulate sweating of the palms and the armpits. Hodgkin’s disease, central nervous system tumors, and breast cancers can cause sweaty palms.10Jabłonowska, O., Woźniacka, A., & Dziankowska-Bartkowiak, B. (2020). Hyperhidrosis: causes and treatment options. Dermatology Review/Przegląd Dermatologiczny, 107(3), 246-256.
Infections
Serious infections such as Tuberculosis and septicemia. TB patients often report nocturnal (night-time) sweating due to dysregulation of the hormone cortisol.11Luies, L., & Du Preez, I. (2020). The echo of pulmonary tuberculosis: mechanisms of clinical symptoms and other disease-induced systemic complications. Clinical microbiology reviews, 33(4), 10-1128.Transient sweating of the palms may also occur in feverish conditions.
Palmar hyperhidrosis can be an unwanted gift from the surgeon. Though rare, cardiac surgery may also cause excessive palm sweating.
Why Do Only My Palms Sweat Excessively And Not Other Body Parts?
The eccrine glands in palms and soles are responsible for sweat production in hands and feet, respectively. The postganglionic sympathetic neurons innervate the eccrine sweat glands. In the case of hands and feet, the neurotransmitter that stimulates sweat production is acetylcholine. However, the groin, chest, and armpit sweat glands are apocrine sweat glands. Norepinephrine activates these glands, not acetylcholine. Therefore, any acetylcholine imbalance leads to profuse sweating only in the hands and feet.
Palmar Hyperhidrosis Diagnosis
Your doctor will start with a complete history of sweating, including drug history (to rule out drug-induced hyperhidrosis) and family history of hyperhidrosis (if present).
The physician also inquires about the duration and pattern of sweating. Most patients report at least one episode of excessive sweating during a week, so the frequency of sweating is also an important question. He might also inquire about associated symptoms such as fever, appetite/weight loss, or hormone imbalances.
Palmar Hyperhidrosis Diagnostic Criteria
An individual is diagnosed as PH if he/she suffers from excessive sweating for 6 months or more, with no apparent cause, and fulfills any two of the following characteristics:12Haider, A., & Solish, N. (2005). Focal hyperhidrosis: diagnosis and management. Cmaj, 172(1), 69-75.
- Symmetrical sweating on both hands (bilateral)
- Has a family history (of HH)
- At least one episode of sweating/week
- The age of onset is greater than 25 years
- No sweating during sleep
- Sweating impairs daily activities
Diagnostic Tests
Majorly there are two diagnostic tests done to diagnose palmar hyperhidrosis:
Iodine-Starch (Minor) Test:
An alcoholic solution of iodine (2%) is applied to the palm and dried. Cornstarch is sprinkled over the affected area. In a positive result, the iodine-starch solution turns dark blue.
Paper Test:
This involves placing specialized paper on the palms to absorb sweat off the surface. The weight of the sweaty paper is measured to calculate the amount of sweat accumulated. A modified iodine-paper technique also exists which helps determine the number of sweat glands involved in the disease. 13Gagnon, D., Ganio, M. S., Lucas, R. A., Pearson, J., Crandall, C. G., & Kenny, G. P. (2012). Modified iodine-paper technique for the standardized determination of sweat gland activation. Journal of Applied Physiology, 112(8), 1419-1425.Differential diagnosis of palmar hyperhidrosis includes sleep hyperhidrosis. In this very condition, patients experience episodes of moderate-to-diffuse sweating during sleep.
Palmar Hyperhidrosis Treatment
Sweaty palms do not pose any physical health concerns, but they can hamper daily activities and psychological health. The main aim of treatment strategies is to improve the patient’s quality of life.
Non-Surgical Treatment
Most healthcare providers prefer alleviating symptoms with non-surgical treatment (especially topical) therapy. The different types of modalities include:
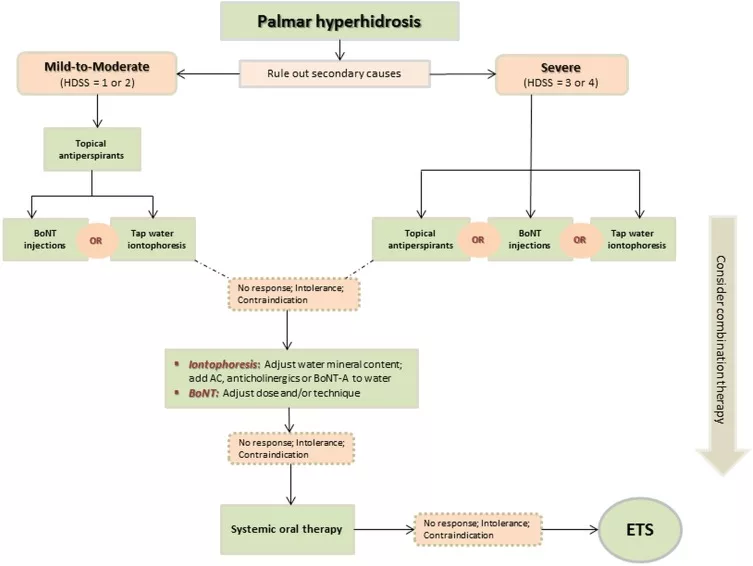
Antiperspirants
Astringents or antiperspirant solutions are the first line of treatment in the management of mild-to-moderate palmar hyperhidrosis. The most commonly prescribed palmar hyperhidrosis antiperspirants contain aluminum chloride (in the form of an aqueous solution of 20-30%). These solutions work by blocking the sweat glands. In a study, topical application of an antiperspirant (containing aluminum chloride) significantly reduced sweat production in plantar hyperhidrosis.14Streker, M., Reuther, T., Hagen, L., & Kerscher, M. (2012). Hyperhidrosis plantaris–a randomized, half‐side trial for efficacy and safety of an antiperspirant containing different concentrations of aluminium chloride. JDDG: Journal der Deutschen Dermatologischen Gesellschaft, 10(2), 115-119.Doctors advise applying astringents during the night for a couple of times a week.
Iontophoresis
This treatment type involves delivering different medications to the skin using mild electrical currents. Iontophoresis is a renowned way of alleviating persistently excessive sweating, especially in the palms and armpits.
Research suggests iontophoresis to be a safe and effective treatment modality for palmar hyperhidrosis.15Kim, D. H., Kim, T. H., Lee, S. H., & Lee, A. Y. (2017). Treatment of palmar hyperhidrosis with tap water iontophoresis: a randomized, sham-controlled, single-blind, and parallel-designed clinical trial. Annals of Dermatology, 29(6), 728.
Iontophoresis using tap water leads to greater improvements in the Hyperhidrosis Disease Severity Scale (HDSS) than the topical application of aluminum chloride hexahydrate in plantopalmar hyperhidrosis patients. Iontophoresis is also relatively inexpensive.16Rahim, M., Ahmed, N., Khan, K. N., Memon, S., Naveed, T., Shah, S. A., … & Ali, U. (2022). Comparison of the efficacy of tap water iontophoresis versus aluminum chloride hexahydrate in the treatment of palmoplantar hyperhidrosis. Cureus, 14(12).
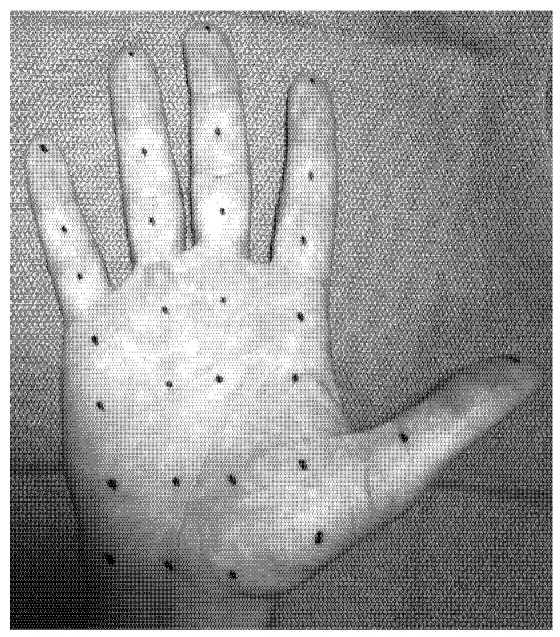
Botulinum Toxin (Botox)
Botox has numerous applications in the cosmetic field. However, an injection of the botulinum toxin can also help relegate your palm sweating. Once inside the body, it blocks the release of acetylcholine, thereby halting the activation of eccrine sweat glans. It is a safe and effective treatment for palmar hyperhidrosis.17Campanati, A., Gregoriou, S., Consales, V., Rizzetto, G., Bobyr, I., Diotallevi, F., … & Offidani, A. (2020). Combined treatment of palmar hyperhidrosis with botulinum toxin type A and oxybutynin chloride: results of a clinical, multicenter, prospective study. Dermatologic therapy, 33(6), e14039.
Anticholinergic Drugs
Anticholinergics are medicines that compete with the acetylcholine at the receptors, thereby blocking the neurotransmitter’s binding and action. Anticholinergic medicines are good at alleviating perspiration but there are multiple adverse effects (dry mouth, constipation, postural hypotension). Therefore, oral anticholinergics for PH are rarely prescribed.18Cruddas, L., & Baker, D. M. (2017). Treatment of primary hyperhidrosis with oral anticholinergic medications: a systematic review. Journal of the European Academy of Dermatology and Venereology, 31(6), 952-963.However, topical anticholinergics are being tested and have shown promising results so far.19Wong, N. S., Adlam, T. M., Potts, G. A., & Farshchian, M. (2022). Hyperhidrosis: a review of recent advances in treatment with topical anticholinergics. Dermatology and therapy, 12(12), 2705-2714.Common anticholinergic drugs include:
- Oxybutynin
- Benztropine
- Propantheline
- Glycopyrrolate
Psychotherapy And Behavioral Therapy
Your doctor may advise psychotherapy if the hyperhidrosis is secondary to stress and anxiety. Behavioral therapies like CBT help control emotions and aid in coping with the disease.
Other non-surgical treatment options that may be work for PH patients include:
- Microwave therapy
- High-Intensity Focused Ultrasound (HIFU) therapy
- Fractional radiofrequency via micro-needling
Surgical Options
Thoracic Sympathectomy
Video-assisted thoracoscopic sympathectomy (VATS) or Endothoracic sympathectomy (ETS) is a minimally-invasive surgical procedure in which the surgeon removes (cuts and clips) the abnormal part of the nerve innervating the sweat glands. Patients report improvements in quality of life after thoracic sympathectomy.20Wei, Y., Xu, Z. Q. D., & Li, H. (2020). Quality of life after thoracic sympathectomy for palmar hyperhidrosis: a meta-analysis. General Thoracic and Cardiovascular Surgery, 68, 746-753.
Final Words
Sweaty palms (or palmar hyperhidrosis) can develop due to neuronal issues (primary PH) or secondary to underlying comorbidities like hyperthyroidism, diabetes, drug abuse, etc. Excessive perspiration leads to embarrassment and issues in carrying out daily chores. Treatment aims at reducing the production/action of the overactive neurotransmitter acetylcholine. Topical antiperspirants work for most patients. Non-surgical treatment modalities include iontophoresis, Botox, and psychotherapy (in case of stress-induced hyperhidrosis). Thoracic sympathectomy is the only surgical option reserved for advanced patients. The surgical removal of the faulty nerve leads to significant improvements in quality of life.
Refrences
- 1Romero, F. R., Haddad, G. R., Miot, H. A., & Cataneo, D. C. (2016). Palmar hyperhidrosis: clinical, pathophysiological, diagnostic, and therapeutic aspects. Anais brasileiros de dermatologia, 91, 716-725.
- 2Laje, P. (2022). Palmar Hyperhidrosis. In Fundamentals of Pediatric Surgery (pp. 415-420). Cham: Springer International Publishing.
- 3Hsu, V. M., Shah, V. V., Aldahan, A. S., Mlacker, S., Samarkandy, S., & Nouri, K. (2017). Hyperhidrosis and stress. Stress and Skin Disorders: Basic and Clinical Aspects, 137-148.
- 4Leta, V., van Wamelen, D. J., Rukavina, K., Jaakkola, E., Sportelli, C., Wan, Y. M., … & Chaudhuri, K. R. (2019). Sweating and other thermoregulatory abnormalities in Parkinson’s disease: A review. Annals of Movement Disorders, 2(2), 39-47.
- 5Henning, M. A., Pedersen, O. B., & Jemec, G. B. (2019). Genetic disposition to primary hyperhidrosis: a review of the literature. Archives of dermatological research, 311(10), 735-740.
- 6Almohideb, M., Aljihani, M., Bukhari, M., Algethami, B., Asiri, O., & Alnamlah, A. (2021). The Impact of Hyperhidrosis on Patients’ Quality of Life and Daily Activities. International Journal of Pharmaceutical Research And Allied Sciences, 10(2-2021), 77-83.
- 7Misra, M. (2021). Excessive Sweating and Heat Intolerance. Endocrine Conditions in Pediatrics: A Practical Guide, 139-141.
- 8Romero, F. R., Haddad, G. R., Miot, H. A., & Cataneo, D. C. (2016). Palmar hyperhidrosis: clinical, pathophysiological, diagnostic, and therapeutic aspects. Anais brasileiros de dermatologia, 91, 716-725.
- 9Oulee, A., Mendoza, R., & Nguyen, E. (2024). Reactive Hyperhidrosis Induced by Topical Products. The Journal of Clinical and Aesthetic Dermatology, 17(1), 6.
- 10Jabłonowska, O., Woźniacka, A., & Dziankowska-Bartkowiak, B. (2020). Hyperhidrosis: causes and treatment options. Dermatology Review/Przegląd Dermatologiczny, 107(3), 246-256.
- 11Luies, L., & Du Preez, I. (2020). The echo of pulmonary tuberculosis: mechanisms of clinical symptoms and other disease-induced systemic complications. Clinical microbiology reviews, 33(4), 10-1128.
- 12Haider, A., & Solish, N. (2005). Focal hyperhidrosis: diagnosis and management. Cmaj, 172(1), 69-75.
- 13Gagnon, D., Ganio, M. S., Lucas, R. A., Pearson, J., Crandall, C. G., & Kenny, G. P. (2012). Modified iodine-paper technique for the standardized determination of sweat gland activation. Journal of Applied Physiology, 112(8), 1419-1425.
- 14Streker, M., Reuther, T., Hagen, L., & Kerscher, M. (2012). Hyperhidrosis plantaris–a randomized, half‐side trial for efficacy and safety of an antiperspirant containing different concentrations of aluminium chloride. JDDG: Journal der Deutschen Dermatologischen Gesellschaft, 10(2), 115-119.
- 15Kim, D. H., Kim, T. H., Lee, S. H., & Lee, A. Y. (2017). Treatment of palmar hyperhidrosis with tap water iontophoresis: a randomized, sham-controlled, single-blind, and parallel-designed clinical trial. Annals of Dermatology, 29(6), 728.
- 16Rahim, M., Ahmed, N., Khan, K. N., Memon, S., Naveed, T., Shah, S. A., … & Ali, U. (2022). Comparison of the efficacy of tap water iontophoresis versus aluminum chloride hexahydrate in the treatment of palmoplantar hyperhidrosis. Cureus, 14(12).
- 17Campanati, A., Gregoriou, S., Consales, V., Rizzetto, G., Bobyr, I., Diotallevi, F., … & Offidani, A. (2020). Combined treatment of palmar hyperhidrosis with botulinum toxin type A and oxybutynin chloride: results of a clinical, multicenter, prospective study. Dermatologic therapy, 33(6), e14039.
- 18Cruddas, L., & Baker, D. M. (2017). Treatment of primary hyperhidrosis with oral anticholinergic medications: a systematic review. Journal of the European Academy of Dermatology and Venereology, 31(6), 952-963.
- 19Wong, N. S., Adlam, T. M., Potts, G. A., & Farshchian, M. (2022). Hyperhidrosis: a review of recent advances in treatment with topical anticholinergics. Dermatology and therapy, 12(12), 2705-2714.
- 20Wei, Y., Xu, Z. Q. D., & Li, H. (2020). Quality of life after thoracic sympathectomy for palmar hyperhidrosis: a meta-analysis. General Thoracic and Cardiovascular Surgery, 68, 746-753.

