Lennox Gastaut Syndrome is an epileptic disorder that occurs in infants and children. This condition is also called childhood encephalopathy. Infants or children with Lennox gastaut syndrome experience recurrent epileptic attacks and manifest characteristic EEG patterns associated with learning, cognitive, and behavioral impairment. This syndrome has a high rate of mortality in infants and children.
What is Lennox Gastaut Syndrome?
Lennox gastaut syndrome is a rare disorder that most commonly affects children between the age of 3-4 years. It was first described by Dr.Henri Gastaut in Marseille, France, in 1966, and its characteristic EEG patterns were described by Dr.William. G. Lennox from the United States of America (USA). As these scientists described the features of this syndrome, this syndrome was named after these two scientists.
Patients with this syndrome have epilepsy since their childhood that remains throughout their lives. This is the most severe form of epilepsy. It can occur in sleep and wakefulness. Moreover, it can impact the psychomotor system, giving rise to abnormal behavior and cognitive impairment. Abnormal behavior can lead to agitation, psychosis, and autism. Key features of LGS include early onset of seizures, multiple types of seizures, developmental delay, and a characteristic EEG pattern.
LGS is a rare form of epilepsy that accounts for only 2-5% of all childhood epilepsy. This syndrome’s overall incidence and prevalence is about 1-2% per 100,000 people worldwide. Notably, this syndrome more commonly targets males than females. The onset of LGS is between 3-5 years of age.1Lennox-Gastaut syndrome: MedlinePlus Genetics. (n.d.). https://medlineplus.gov/genetics/condition/lennox-gastaut-syndrome/#causes
What are the Causes of Lennox Gastaut Syndrome?
There are multiple causes of Lennox gastaut syndrome. It can be symptomatic or idiopathic. Some genetic causes are not well understood.
Symptomatic LGS:
It is the most common form of LGS and constitutes 75% of LGS cases. In symptomatic LGS, the underlying pathology is known and can be diagnosed. The causes include:
- Brain injury or trauma that can occur before or after birth
- Hypoxic brain injury
- Tuberous sclerosis
- Metabolic abnormalities
- Brain malformation
- West syndrome
- Infantile spasm
- Brain tumors
- Infection (bacterial or viral meningitis and encephalitis)
- Stroke
- Genetic disorders
Children having secondary LGS show a worse prognosis than others.
Idiopathic:
In idiopathic causes, the exact cause of the LGS remains unknown. The child has normal brain imaging and has no history of brain injury before the onset of LGS. However, some genetic changes contribute to this syndrome. These changes include mutations in GABRB3, ALG13, SCN1A, and CHD2.2Camfield P. R. (2011). Definition and natural history of Lennox-Gastaut syndrome. Epilepsia, 52 Suppl 5, 3–9. https://doi.org/10.1111/j.1528-1167.2011.03177.x
What type of seizures does my child have in Lennox Gastaut Syndrome?
Lennox gastaut syndrome is associated with multiple types of seizures. These seizures are recurrent and occur for a short period, but they can occur for a longer period (status epilepticus). Types of seizures involved in LGS are:
Tonic-Clonic Seizures:
In tonic-clonic seizures, the whole body of your child is involved. In this type of seizure, muscles become stiff like a rod (increased tone), and uncontrolled bodily movement and fits occur.
Tonic Seizures:
In tonic seizures, only the tone of the muscles increases without any body movement. Tonic seizures can occur during sleep and also when your child is awake.
Atonic Seizures:
In this type, the tone of the muscles decreases and leads to frequent falls called drop attacks.
Absence Seizures:
In the absence seizures, there is a sudden loss of awareness of your child. In these seizures, the patient experiences multiple staring spells. These seizures remain for a few seconds to a few minutes.
Myoclonic Seizures:
Myoclonic seizures involve only muscles. These are characterized by uncontrolled muscle movements. These contractions can occur in one or both limbs.
Status Epilepticus:
It is an emergency in which the patient experiences continuous epileptic episodes (episodes of fits) that remain for hours.3Lennox-Gastaut Syndrome. (n.d.). National Institute of Neurological Disorders and Stroke. https://www.ninds.nih.gov/health-information/disorders/lennox-gastaut-syndrome#:~:text=Lennox%2DGastaut%20syndrome%20is%20a,seizures%20that%20vary%20among%20individuals.

What are the Stages of Seizures?
Seizures usually begin with three stages. These are:
Aura or Prodrome Stage (Pre-Seizure):
It is a pre-epileptic stage that occurs more often when your child feels unpleasant. It is characterized by odd behavior and changes in mood and senses. Your child may hear voices or see things that do not exist in reality.
Seizures:
In this stage, your child experiences seizures depending upon the type.
Post-Seizures:
This stage occurs when the seizures end and your child gains full consciousness.
Symptoms of Lennox Gastaut Syndrome:
The symptoms of LGS vary from person to person depending upon the cause, severity of the disease, and type of seizure. Symptoms of LGS according to the type include 4National Organization for Rare Disorders. (2023, November 20). Lennox-Gastaut syndrome – Symptoms, causes, treatment | NORD. https://rarediseases.org/rare-diseases/lennox-gastaut-syndrome/
Tonic seizures:
Symptoms of a tonic seizure include:
- Increase muscle tone (stiffness) in one or both limbs, including the trunk
- Falling
Atonic Seizures:
- Decrease or loss of muscle that is sudden in onset
- Going limp and falling attacks
- Drooping of the eyelid
- Loss of consciousness for short duration
- Head nodding and jerking movement
Absence Seizures:
- Sudden loss of awareness
- Frequent starring of eyes
Myoclonic Seizures:
- Involuntary muscle contractions
- Muscle spasm
Other Symptoms:
Some other symptoms are also associated with the LGS. These are5Cherian, K. A., MD. (n.d.). Lennox-Gastaut Syndrome Treatment & Management: Approach considerations, antiepileptic therapy, Corpus callostomy. https://emedicine.medscape.com/article/1176735-treatment?form=fpf#d9
- Odd behavior
- Dizziness
- Developmental delay
- Intellectual abnormalities that worsen with time because of resistant treatment
- Cognitive impairment
- Urinary incontinence
How to Diagnose Lennox Gastaut Syndrome?
Children under eight years of age having recurrent and uncontrolled seizures that are resistant to medications come under suspicion of LGS. Early diagnosis is necessary because it can cause irreversible brain damage if it remains undiagnosed. The evaluation of the patient with LGS depends upon the history, clinical examination, characteristic EEC pattern, laboratory investigations, and imaging.

History:
The clinical history of the patient helps to diagnose the disease. In history, your doctor will ask some questions. These include:
Prenatal History
In prenatal history, your doctor may ask questions to the mother regarding his/her before the birth. These questions include the following points:
- Any infection during pregnancy?
- Drug history during pregnancy?
- Any prenatal ultrasound records?
- Any history of falls during pregnancy?
Birth History
- History of trauma during birth
- Any history of delayed crying?
- Was any congenital anomaly present at the time of delivery?
- Is your baby full-term or premature?
Postnatal History
Postnatal history includes a history of trauma, infections, brain tumors, metabolic disorders, behavioral abnormalities, intellectual abnormalities, and seizures. He will ask you about the onset and duration of these seizures.
Your doctor may also ask about the history of gestational diabetes, eclampsia, pre-eclampsia, and past medical history.
Physical Examination:
In a physical examination, your doctor will examine your child. Moreover, he will examine your child’s mood and behavior.
Neurological Examination:
In a neurological examination, your doctor will examine your child’s mental status. Patients with LGS show deficits in higher cognitive function and intellectual disabilities during neurological examination.
Laboratory Investigations:
Laboratory investigations are also required to rule out the other causes of seizures. These investigations include:
- Complete blood count (CBC) to check hemoglobin level
- White blood cell count to check infection
- Serum electrolytes
- Random blood glucose level
- Serum calcium level
- Lactic acid level
- Complete urine examination
- Cerebrospinal fluid examination
- Serum ammonia level
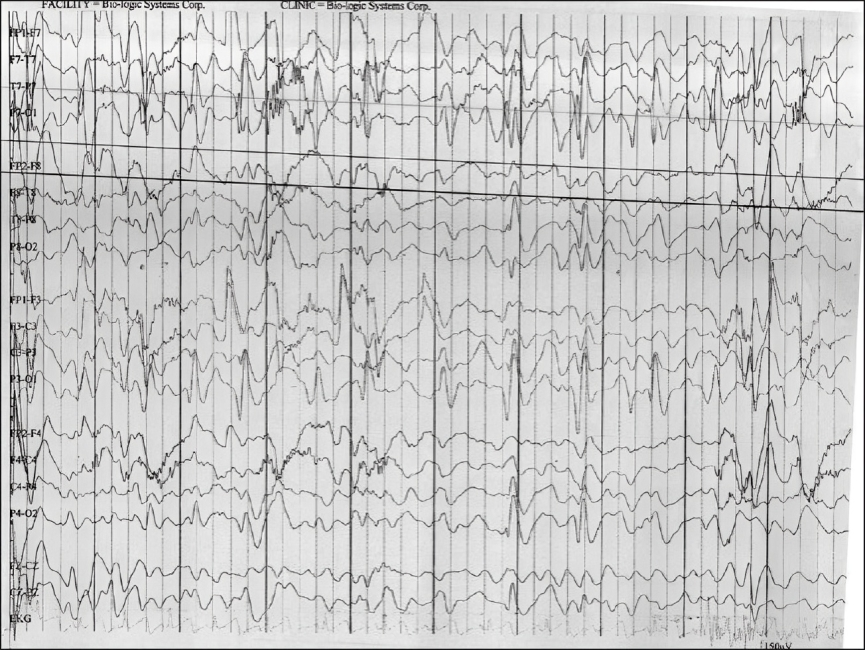
Electroencephalogram (EEG):
EEG (sleep and awake) is a diagnostic test in which a doctor records your child’s brain impulses. People with LGS show characteristic EEG patterns (Spike wave pattern).
Characteristic of EEG:
The EEG of a patient with Lennox gastaut syndrome has special characteristics that are:
- Constant or transient slow background
- Slow spike-wave pattern during sleep
- Polyspikes and slow-wave patterns during sleep (Non-REM)
- Decreased spike-wave pattern during REM sleep
Imaging:
Neuroimaging will help your doctor see the internal structure of your Child’s brain. Imaging includes MRI, CT scan, and PET scan. MRI is the preferred imaging study in patients with LGS rather than a CT scan. It is usually advised in patients with suspicion of brain injury and hematoma resulting from falls.6Cherian, K. A., MD. (n.d.). Lennox-Gastaut Syndrome Treatment & Management: Approach considerations, antiepileptic therapy, Corpus callostomy. https://emedicine.medscape.com/article/1176735-treatment?form=fpf#d9

How to Treat Lennox Gastaut Syndrome?
The main goal of the treatment of LGS is to control seizures. Seizures are controlled by medical management, dietary management, and surgical management. However, early diagnosis and treatment are necessary to prevent irreversible brain damage.
Medical Management :
The goal of medical management is to control recurrent bouts of seizures. Multiple medications are used to treat seizures depending upon the type of seizures and recurrence. Controls of tonic and atonic seizures are first taken under consideration because these seizures cause multiple falls that can cause brain injury. The medicines that are used for seizure control are:
Lamotrigine
This antiepileptic medication Is a drug of choice to treat generalized tonic-clonic seizures. It also helps to improve the mood and behavior of the affected child. According to FDA recommendations, this drug is used in patients older than two years.
Valproate
It can treat multiple seizures. It is used in combination with other antiepileptic drugs to treat different types of seizures and is also used as a monotherapy to treat seizures.
Felbamate
This drug treats tonic and atonic seizures. This drug is used in resistant cases when all the drugs are failed to treat seizures. Moreover, it cannot be used in routine practice due to severe side effects.
Topiramate
This drug is used to treat tonic-clonic seizures. It is also used in children with an age greater than two years.
Cannabidiol Oral Solution
This Oral solution usually treats drop attacks (atonic seizures). It is also recommended for children > 2 years.
Rufinamide
This drug treats tonic and atonic seizures and is used in patients with ages greater than four years. This drug does not interfere with other types of seizures.
Clobazam
It belongs to the family of benzodiazepines and is used as an adjunctive drug to treat seizures.
Some other medications are used to treat seizures but are not common. These medications are ethosuximide, clonazepam, leveiacteum, and zonisamide.
Medicines that worsen seizures in LGS:
Some medications can worsen the seizure types in LGS. However, these medicines are not used to treat LGS. These medicines include:
- Phenytoin
- Carbamazepine
- Phenobarbitol
- Gabapentin
- Lacosamide
Dietary Management:
LGS is sometimes refractory to medicines. Some dietary modifications decrease the seizures. The diet plan for LGS includes:
- A diet with a low glycemic index
- Keto diet
- Atkins diet
A ketogenic diet contains higher fat levels than protein and carbohydrates (non-ketogenic). The ratio of ketogenic and non-ketogenic diets is about 4:1. Patients taking ketogenic diets show promising effects, including seizure control and behavioral and cognitive improvement. The result of the ketogenic diet depends upon the compliance of the patient.
Surgical Management:
Surgery is the last step to treat LGS when medical management and dietary protocols fail to treat seizures. However, the surgical management of LGS includes the following approaches:
Vagus Nerve Stimulation
During this surgery, a surgeon implants a device in your child’s brain to send signals through the vagus nerve. According to studies, vagus nerve stimulation shows a 50 % decrease in seizure frequency with a follow-up period of 5 years.
Corpus Callosotomy
Corpus callosotomy is effective in treating drop attacks but not for all types of seizures. Therefore, it is a palliative surgical approach, which is not curative.
Focal Cortical Resection
In rare cases when the cause of seizures is brain tumors, hematoma, or any other structural lesions. In focal cortical resection, the affected part is resected to improve the seizure.7Amrutkar, C. V. (2023, July 31). Lennox Gastaut Syndrome. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK532965/
Follow-up:
A regular follow-up is necessary to check the efficacy of ongoing treatment and the ongoing side effects.
Life Expectancy of Lennox Gastaut Syndrome
The overall prognosis of the patient with Lennox gastaut syndrome remains poor. Sudden death can occur due to brain damage or frequent falls that cause injury to your child’s brain. However, if the child has a positive history of infantile syndrome or West syndrome, then the prognosis becomes worse.
Moreover, people with idiopathic LGS show less severe symptoms and a better prognosis than others. The mortality rate is 3-7 percent in 5-7 years of follow-up.
How can I prevent brain injuries in my child having LGS?
Brain damage occurs when your child experiences an episode of seizures. Medical treatment can stop these fits to reduce brain damage. Moreover, wearing helmets and face guards can help your child from traumatic brain and face injuries. Unfortunately, if an injury has occurred, it is irreversible.8Al-Banji, M. H., Zahr, D. K., & Jan, M. M. (2015). Lennox-Gastaut syndrome. Management update. Neurosciences (Riyadh, Saudi Arabia), 20(3), 207–212. https://doi.org/10.17712/nsj.2015.3.20140677
Is Lennox gastaut syndrome Progressive?
People with LGS experience multiple episodes of seizures of different types daily that change with age. There is a progressive deterioration of the brain’s cognitive, behavioral, and intellectual functions with time. Therefore, most patients with LGS are unable to live and work independently.
Conclusion
To conclude, Lennox gastaut syndrome is a childhood disease in which an infant or child suffers from recurrent episodes of epilepsy. It manifests as seizures, dizziness, urinary incontinence, developmental delay, and intellectual abnormalities. Medical management controls recurrent bouts of seizures. If medical treatment fails, surgical treatment is suitable. Lennox gastaut syndrome has a poor prognosis.
Refrences
- 1Lennox-Gastaut syndrome: MedlinePlus Genetics. (n.d.). https://medlineplus.gov/genetics/condition/lennox-gastaut-syndrome/#causes
- 2Camfield P. R. (2011). Definition and natural history of Lennox-Gastaut syndrome. Epilepsia, 52 Suppl 5, 3–9. https://doi.org/10.1111/j.1528-1167.2011.03177.x
- 3Lennox-Gastaut Syndrome. (n.d.). National Institute of Neurological Disorders and Stroke. https://www.ninds.nih.gov/health-information/disorders/lennox-gastaut-syndrome#:~:text=Lennox%2DGastaut%20syndrome%20is%20a,seizures%20that%20vary%20among%20individuals.
- 4National Organization for Rare Disorders. (2023, November 20). Lennox-Gastaut syndrome – Symptoms, causes, treatment | NORD. https://rarediseases.org/rare-diseases/lennox-gastaut-syndrome/
- 5Cherian, K. A., MD. (n.d.). Lennox-Gastaut Syndrome Treatment & Management: Approach considerations, antiepileptic therapy, Corpus callostomy. https://emedicine.medscape.com/article/1176735-treatment?form=fpf#d9
- 6Cherian, K. A., MD. (n.d.). Lennox-Gastaut Syndrome Treatment & Management: Approach considerations, antiepileptic therapy, Corpus callostomy. https://emedicine.medscape.com/article/1176735-treatment?form=fpf#d9
- 7Amrutkar, C. V. (2023, July 31). Lennox Gastaut Syndrome. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK532965/
- 8Al-Banji, M. H., Zahr, D. K., & Jan, M. M. (2015). Lennox-Gastaut syndrome. Management update. Neurosciences (Riyadh, Saudi Arabia), 20(3), 207–212. https://doi.org/10.17712/nsj.2015.3.20140677

