
Port-wine stain is a non-cancerous condition some babies are born with. It is named so because it looks like wine was splashed on the skin. The condition develops because of the congenital malformation of blood vessels under the skin. Port wine stains can be found on any part of the body. The stains get darker with time and do not go on their own. One of the best port wine stain treatments is the pulsed dye laser. Although it doesn’t remove the stain permanently, it practically makes it fade away and appear less bumpy.
What is Port-Wine Stain?
Port wine stain, or nevus flammeus, is a birthmark found anywhere on the body, especially on the face, neck, arms, or legs. Around 25 million people worldwide have port wine stain birthmarks. According to research, every 3 in 1000 babies are born with port wine stains.1Liu, L., Li, X., Zhao, Q., Yang, L., & Jiang, X. (2022). Pathogenesis of Port-Wine Stains: Directions for Future Therapies. International journal of molecular sciences, 23(20), 12139. https://doi.org/10.3390/ijms232012139
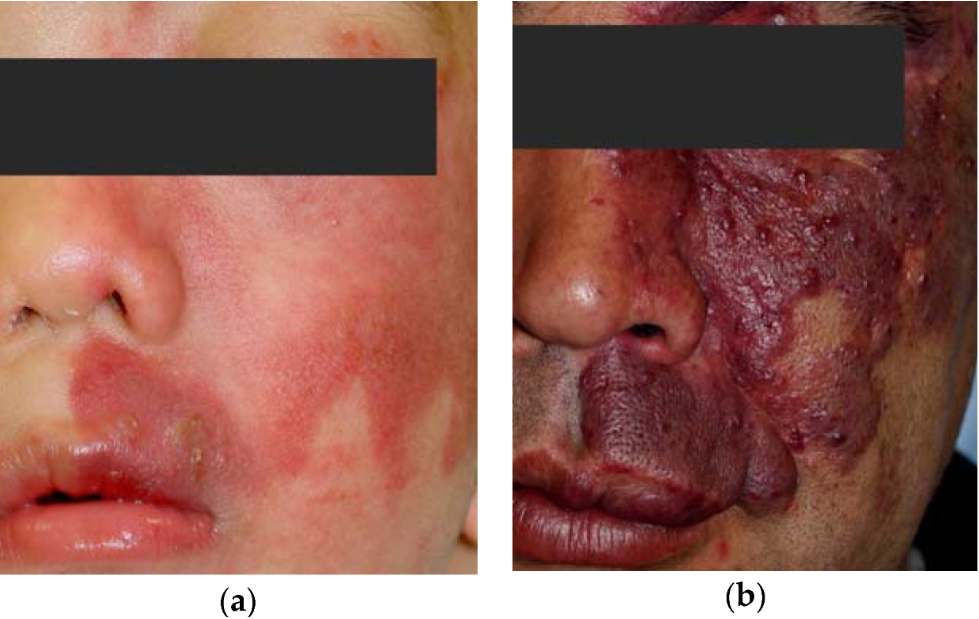
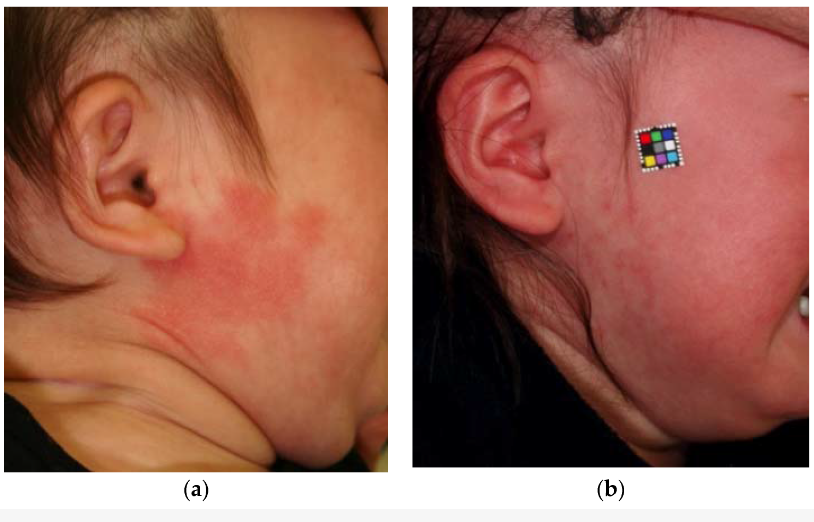
It starts as a flat pinkish stain on the body. Over time, it gets darker and turns reddish-purple. Besides affecting appearance, these birthmark stains can also cause problems with sight, speech, and hearing.2Heiser, A., Jowett, N., Occhiogrosso, J., Tessler, O., & Tan, O. T. (2020). Societal-Perceived Health Utility of Hypertrophic Facial Port-Wine Stain and Laser Treatment. Facial plastic surgery & aesthetic medicine, 22(5), 327–335. Advanced online publication. https://doi.org/10.1089/fpsam.2020.0059
Appearance of Port-Wine Stain
A port wine stain manifests as a pink, red, or purplish discoloration on the skin, exhibiting clearly defined borders. While these birthmarks can emerge on any part of the body, they are most commonly found on the face, neck, and scalp.
Port wine stains are typically present as smooth patches in children. As the child matures, the birthmark expands in size, maintaining proportional growth. Over time, these stains may become thicker and darker, acquiring a pebbly texture beneath the skin. Additionally, they may be more prone to bleeding after an injury, posing challenges in terms of control.
Port-Wine Stain Causes – Why Does It Happen?
There are several hypotheses when it comes to port wine stain causes. The most accepted hypothesis is the one explaining embryological defects.3Shajil C, M Das J. Nevus Flammeus. [Updated 2023 Nov 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK563254/
Normally, we have three layers of the skin: epidermis, dermis, and hypodermis. Blood vessels are present throughout the second or deeper layer – the dermis. These vessels provide oxygen and nutrients to the skin.
In the case of a port wine stain, these vessels are not properly formed during infancy.4Updyke, K. M., & Khachemoune, A. (2017). Port-Wine Stains: A Focused Review on Their Management. Journal of drugs in dermatology: JDD, 16(11), 1145–1151. They get bigger and wider, letting more blood flow through them. Resultantly, the skin of that area looks red or purple.
It’s not because of anything the parents did or didn’t do during pregnancy. In fact, there have been cases when there were no genetic mutations, and still, various family members had PWS.
Difference Between Port-Wine Stain and Other Vascular Birthmarks
Birthmarks usually come under two categories: vascular and non-vascular or pigmented.
Since vascular birthmarks involve blood vessels, they appear pink, red, or purplish. On the other hand, non-vascular pigmented birthmarks are more dark brown, black, blue, or gray.
Let’s explore the differences between port wine stain and other vascular birthmarks.
Port-Wine Stain Vs. Stork Bite
Port wine stains are rare compared to stork bites, which appear in around 44% of babies.5Leung, A. K., Barankin, B., & Hon, K. L. (2014). Persistent salmon patch on the forehead and glabellum in a Chinese adult. Case reports in medicine, 2014, 139174. https://doi.org/10.1155/2014/139174 PWSs become nodular and darker over time, while stork bites remain flat and get darker when the baby cries and strains while defecating or holding breath.
Common sites of port wine stains are the face, neck, and limbs, while stork bites are typically found on the glabella, forehead, and eyelids. The stork bite lesions on the forehead or eyelids are called “angel’s kisses.”
Stork bites, also called “Salmon patches,” are usually symmetrical and often fade over time. They are rarely found after six years of age.6Leung, A. K., Barankin, B., & Hon, K. L. (2014). Persistent salmon patch on the forehead and glabellum in a Chinese adult. Case reports in medicine, 2014, 139174. https://doi.org/10.1155/2014/139174. On the other side, port-wine stains persist throughout life and can be associated with certain syndromes7Wanitphakdeedecha, R., Ng, J. N. C., Yan, C., Manuskiatti, W., Sudhipongpracha, T., & Jantarakolica, T. (2021). Quality of Life and Psychological Effects of Port-Wine Stain: A Review of Literature. Clinical, cosmetic and investigational dermatology, 14, 681–690. https://doi.org/10.2147/CCID.S315804
Port-Wine Stain vs Hemangioma
PWS and hemangiomas are very distinct and can be differentiated easily.
A hemangioma usually appears as a raised, red, or pinkish growth on the skin. It has a smooth, shiny surface with a lumpy texture. It often grows quickly during a baby’s first six months. Unlike port wine stains, many small hemangiomas can shrink on their own.
Sometimes, hemangiomas cause problems with eating, breathing, vision, or a child’s development. In such cases, immediate medical help is needed.
Is Port-Wine Stain Removal Possible?
Yes, it is possible to get rid of the port wine stain. Usually, port wine stain treatment is not required because it is a benign condition. However, treatment is done in the following cases:
- Bleeding from the stained area
- Thick bumpy stain
- Facial disfigurement
- To boost self-esteem
Although the stain doesn’t get removed completely, laser treatment makes it lighter, helping to boost confidence and self-esteem.

Port-Wine Stain Treatment Options
Early consultation with a doctor is beneficial for infants with unique birthmarks, although treatment typically begins during their later years.
There are two choices for treating this birthmark: Laser and cosmetic camouflage.
Laser Treatment for Port-Wine Stain:
Laser treatment, specifically with a pulsed dye laser, is the preferred method for reducing the appearance of a port wine stain. It can also help with the ‘cobblestone effect’ that may occur later in life.
How does Laser Treatment Work?
Different types of lasers, such as argon, YAG, or pulsed dye, can be used. However, the pulsed dye laser is the most preferred type for port wine stain treatment.
A pulsed dye laser uses a focused beam of light that targets the red color in the blood vessels of the port wine stain. This process, known as selective photothermolysis, treats a specific tissue area within the blood vessels using light that generates heat.8Brightman, L. A., Geronemus, R. G., & Reddy, K. K. (2015). Laser treatment of port-wine stains. Clinical, cosmetic and investigational dermatology, 8, 27–33. https://doi.org/10.2147/CCID.S53118
How long does Laser Treatment for Birthmarks take?
It’s recommended to undergo four to six treatments over a few years to achieve the best results.
The duration of each treatment depends on whether the child receives it under general or local anesthesia and the characteristics of their birthmark.
What is the Procedure for Laser Treatment for PWS?
Step 1: The initial step for laser treatment is a ‘Patch test’ to see how well the birthmark responds to the laser.
A local anesthetic cream is used to numb the area. A test patch containing a few laser dots is applied to the birthmark. It may cause discomfort, similar to being flicked with a rubber band.
Step 2: Once the test patch shows a successful result, regular treatment sessions with more laser dots can begin.
Children may require local or general anesthesia based on the size and location of the birthmark.
Step 3: The child’s skin may appear bruised and sore after each laser session. It’s important to care for their skin between appointments.
Cosmetic Camouflage:
Some people cannot afford laser treatment, so they opt for cosmetic camouflage. This is not a treatment but rather a technique for hiding port wine stains using special water-resistant makeup.
As the name “camouflage” indicates, the technique doesn’t remove the stain but rather covers it up. When applied on the face, it’s best to remove it nightly with cleansing cream; on the body, it can be left for three or four days.
A port wine stain can get dry, so remember to moisturize it. If the skin is bruised, clean it gently with soap and water, then apply pressure with a clean bandage.
Port-Wine Stain Complications
Here are some Port Wine Stain complications that can affect its prognosis:
Sturge-Weber Syndrome:
Sturge-Weber syndrome, a rare condition occurring in 1 in 20,000 to 50,000 births, involves a similar stain on the face.9Shirley, M. D., Tang, H., Gallione, C. J., Baugher, J. D., Frelin, L. P., Cohen, B., North, P. E., Marchuk, D. A., Comi, A. M., & Pevsner, J. (2013). Sturge-Weber syndrome and port-wine stains caused by somatic mutation in GNAQ. The New England journal of medicine, 368(21), 1971–1979. https://doi.org/10.1056/NEJMoa1213507
It is caused by an abnormality in the blood vessels of the face area supplied by the ophthalmic branch of the fifth cranial nerve (trigeminal nerve).
If a baby has a port-wine stain on the face, there’s a 6% chance of having Sturge-Weber syndrome, increasing to 26% if the stain is on a specific nerve area.10Ch’ng, S., & Tan, S. T. (2008). Facial port-wine stains – clinical stratification and risks of neuro-ocular involvement. Journal of plastic, reconstructive & aesthetic surgery: JPRAS, 61(8), 889–893. https://doi.org/10.1016/j.bjps.2007.05.011
Glaucoma:
There is a higher chance of glaucoma in patients who have PWS stains near the regions supplied by the ophthalmic branch of the trigeminal nerve.11Wu, Y., Yu, R. J., Chen, D., Xu, L., Li, M., Zhu, L., Guo, C. Y., & Guo, W. Y. (2017). Glaucoma in Patients with Eyes Close to Areas Affected by Port-wine Stain has Lateral and Gender Predilection. Chinese Medical Journal, 130(24), 2922–2926. https://doi.org/10.4103/0366-6999.220319
Skin Changes:
Over time, port wine stain becomes nodular, and the skin becomes a bit bumpy over that area.
Bleeding:
In certain cases, port wine stains bleed when touched.
Cosmetic Concerns:
The most common complication is facial disfigurement. It causes various emotional or psychological effects, especially if the birthmark is on a visible area like the face.
Self-Esteem Issues:
Not only medical but also psychological complications come with PWS.
Children or adults with port wine stains have low self-esteem, particularly if they face social stigma, teasing, or bullying in their surroundings.
How do you help a child with a Port-Wine Stain?
A port wine stain might make your child feel awkward, especially if it’s on their face. People often stare and say insensitive things.
Studies have shown that children born with a larger port wine stain often have negative experiences during their childhood.12Fournier, H., Calcagni, N., Morice-Picard, F., & Quintard, B. (2023). Psychosocial implications of rare genetic skin diseases affecting appearance on daily life experiences, emotional state, self-perception and quality of life in adults: a systematic review. Orphanet journal of rare diseases, 18(1), 39. https://doi.org/10.1186/s13023-023-02629-1 They may develop coping mechanisms like avoiding gatherings, splashing taunts, or dark humor.
Parents should help their children by:
- Talking openly about the birthmark using simple words.
- Telling the kid that PWS is a special mark that makes them unique.
- Help the child to learn camouflage to make up for the stain.
- Educate those around the child about the birthmark and foster understanding and acceptance.
- Teaching the child how to respond to questions about the stain.
To sum it up, PWS is a birthmark that can be present on any part of the body. It is a benign condition and usually causes no harm. Normally, there’s no need for the port wine stain treatment. However, laser treatment can be considered if the stain affects a child’s confidence or leads to potential complications.
Refrences
- 1Liu, L., Li, X., Zhao, Q., Yang, L., & Jiang, X. (2022). Pathogenesis of Port-Wine Stains: Directions for Future Therapies. International journal of molecular sciences, 23(20), 12139. https://doi.org/10.3390/ijms232012139
- 2Heiser, A., Jowett, N., Occhiogrosso, J., Tessler, O., & Tan, O. T. (2020). Societal-Perceived Health Utility of Hypertrophic Facial Port-Wine Stain and Laser Treatment. Facial plastic surgery & aesthetic medicine, 22(5), 327–335. Advanced online publication. https://doi.org/10.1089/fpsam.2020.0059
- 3Shajil C, M Das J. Nevus Flammeus. [Updated 2023 Nov 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK563254/
- 4Updyke, K. M., & Khachemoune, A. (2017). Port-Wine Stains: A Focused Review on Their Management. Journal of drugs in dermatology: JDD, 16(11), 1145–1151.
- 5Leung, A. K., Barankin, B., & Hon, K. L. (2014). Persistent salmon patch on the forehead and glabellum in a Chinese adult. Case reports in medicine, 2014, 139174. https://doi.org/10.1155/2014/139174
- 6Leung, A. K., Barankin, B., & Hon, K. L. (2014). Persistent salmon patch on the forehead and glabellum in a Chinese adult. Case reports in medicine, 2014, 139174. https://doi.org/10.1155/2014/139174
- 7Wanitphakdeedecha, R., Ng, J. N. C., Yan, C., Manuskiatti, W., Sudhipongpracha, T., & Jantarakolica, T. (2021). Quality of Life and Psychological Effects of Port-Wine Stain: A Review of Literature. Clinical, cosmetic and investigational dermatology, 14, 681–690. https://doi.org/10.2147/CCID.S315804
- 8Brightman, L. A., Geronemus, R. G., & Reddy, K. K. (2015). Laser treatment of port-wine stains. Clinical, cosmetic and investigational dermatology, 8, 27–33. https://doi.org/10.2147/CCID.S53118
- 9Shirley, M. D., Tang, H., Gallione, C. J., Baugher, J. D., Frelin, L. P., Cohen, B., North, P. E., Marchuk, D. A., Comi, A. M., & Pevsner, J. (2013). Sturge-Weber syndrome and port-wine stains caused by somatic mutation in GNAQ. The New England journal of medicine, 368(21), 1971–1979. https://doi.org/10.1056/NEJMoa1213507
- 10Ch’ng, S., & Tan, S. T. (2008). Facial port-wine stains – clinical stratification and risks of neuro-ocular involvement. Journal of plastic, reconstructive & aesthetic surgery: JPRAS, 61(8), 889–893. https://doi.org/10.1016/j.bjps.2007.05.011
- 11Wu, Y., Yu, R. J., Chen, D., Xu, L., Li, M., Zhu, L., Guo, C. Y., & Guo, W. Y. (2017). Glaucoma in Patients with Eyes Close to Areas Affected by Port-wine Stain has Lateral and Gender Predilection. Chinese Medical Journal, 130(24), 2922–2926. https://doi.org/10.4103/0366-6999.220319
- 12Fournier, H., Calcagni, N., Morice-Picard, F., & Quintard, B. (2023). Psychosocial implications of rare genetic skin diseases affecting appearance on daily life experiences, emotional state, self-perception and quality of life in adults: a systematic review. Orphanet journal of rare diseases, 18(1), 39. https://doi.org/10.1186/s13023-023-02629-1




