What is Tetralogy of Fallot?
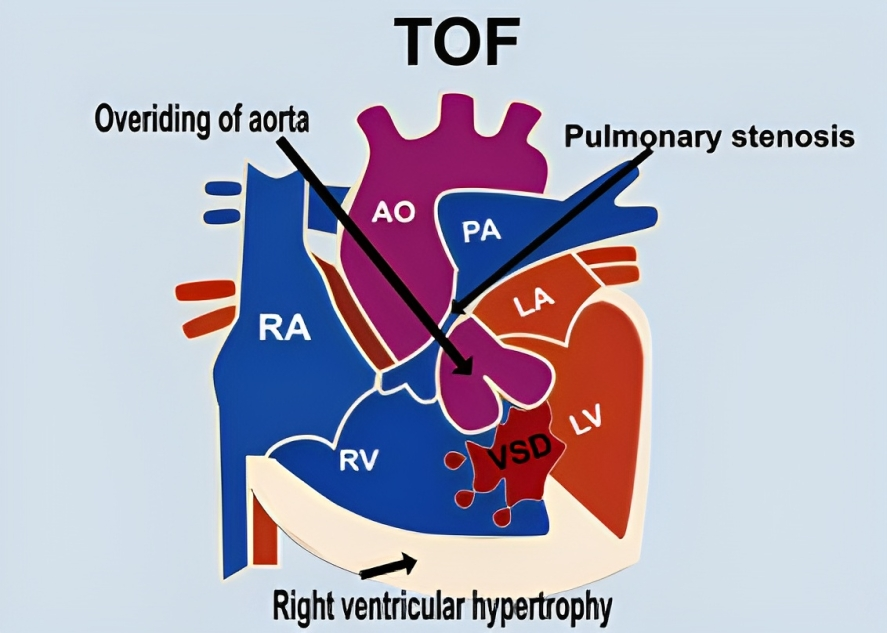
Tetralogy of Fallot is the most common congenital cyanotic heart disease (also known as blue baby disease). It is characterized by four cardiac abnormalities, including Right ventricular hypertrophy, ventricular septal defect (VSD), overriding of the aorta, and right ventricle outflow obstruction. The combination of these anomalies, particularly the septal defect, results in a direct shunting of blood from the right ventricle to the aorta (right-to-left shunt). It is the most common cause of cyanosis in infants due to inadequate blood supply to the lungs for oxygenation.
Children with early diagnosis and treatment of tetralogy of Fallot enjoy better and long-term survival results than others. The mortality rate increases by 50% if it remains untreated.
Tetralogy of Fallot accounts for only 7-10% of all cyanotic heart diseases, with 1-2 cases per 1000-3000 births. It affects males and females equally and is more common in younger ones than adults.1Bhimji, S., MD PhD. (n.d.). Tetralogy of Fallot (TOF) in Adults Treatment & Management: Approach considerations, Medical treatment, Surgical treatment. https://emedicine.medscape.com/article/2035949-treatment#d9?form=fpf
Background
The tetralogy of Fallot was first described by the Danish anatomist Dane Neils Stenson; therefore, it was also named Stein-Fallot tetralogy. In 1777, a Dutch physician, Eduard, Reported a case of a 16-month-old child called “Blue Boy.” Initially, this child was considered to have asthma, but his autopsy revealed a congenitally malformed heart.
Classical Anatomy
Your normal heart consists of four chambers: right atrium, right ventricle, left atrium, and left ventricle. Normally, your blood comes back from your body to your heart via the superior and inferior vena cava into the right atrium. From the right atrium, blood pumps down into the right ventricle through the tricuspid valves. The ventricle contracts and pumps blood toward the pulmonary arteries (carrying deoxygenated blood), and from the pulmonary arteries, it reaches the lungs, where oxygenation occurs.
From the lungs, blood travels toward the left atrium via pulmonary veins (carrying deoxygenated blood). The right atrium pumps blood toward the right ventricle via the mitral valve (bicuspid valve). The ventricle contracts and pumps blood toward the aorta, from where the blood is distributed to the whole body.
Four Cardinal pathological features characterize the classical anatomy of the Tetralogy of Fallot.2Diaz-Frias, J. (2022, January 18). Tetralogy of Fallot. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK513288/ These are:
1- Ventricular Septal Defect (VSD):
It is a clinical condition with a significant defect in the membranous part of the septum (differentiating the ventricles). Due to this defect, there is a large gap between both ventricles, allowing blood to enter from the right ventricle to the left ventricle (right to left shunt).
2- Right Ventricular Outflow Obstruction:
Pulmonary outflow obstruction at the level of the right ventricle is the cardinal feature of the tetralogy of Fallot. Obstruction of blood flow from the right ventricle causes hypertrophy of the right ventricle, which is also a key feature of this disease. If non-resistant blood flows from the right ventricle to the left ventricle, the pressure of the right ventricle increases. This pressure pumps blood from the right to the left ventricle (right to left shunt) and bypasses the pulmonary veins. It leads to hypoxemia due to inadequate oxygenation of the blood.
Right ventricular outflow obstruction becomes more severe when the collateral blood supply is also affected (closed patent ductus arteriosus), resulting in more hypoxemia (lower blood oxygen level). The outflow obstruction can occur on different sites above the level of the pulmonary valve (10%), at the level of the pulmonary valve (10%), and in combination (30%). However, the complete obstruction of the right ventricular outflow can also occur; this is called pulmonary atresia.
3- Overriding of the Aorta:
It is also a pathological condition in which the aorta is present above the ventricular septal defect. Overriding of the aorta drives deoxygenated blood from the right ventricle into the aorta, which circulates into the body. Normally, the aorta arises from the left ventricle, but in 25 % of the cases, it arises from the right ventricle, called the double outlet ventricle.
4- Right Ventricular Hypertrophy:
Right ventricular hypertrophy occurs due to right ventricular outflow obstruction, which increases the right ventricle pressure and leads to hypertrophy of the right ventricle.
Anatomical Variants of the Tetralogy of Fallot
There are some variants of tetralogy of Fallot depending upon the degree of cyanosis. These variants are:
Pink Fallot (Left-Right Shunt):
In this subtype of TOF, the affected child has normal oxygen saturation with no or minimum ventricular outflow obstruction. In this condition, the child is cyanotic and healthy.3Megha and Sakthivel V. “A case of pink tetralogy of Fallot.” International Journal of Contemporary Advanced Research, vol. 7, no. 1, 2018. DOI: http://dx.doi.org/10.24327/ijcar.2018.12981.2301
Blue Fallot (Right to Left Shunt) (15%):
In this subtype, the affected child is cyanotic and has a low level of oxygen saturation. It is the more severe form of TOF in which there is complete ventricular outflow tract obstruction (pulmonary atresia).
Tetralogy of Fallot with Absent Pulmonary Valves (6 % of the TOF):
In this subtype, the child is cyanotic but with an open right ventricular outflow obstruction. This type of TOF can cause respiratory complications due to the absence of a pulmonary valve, which will lead to a pulmonary aneurysm. This pulmonary aneurysm distally puts pressure on the trachea and bronchi, resulting in breathing difficulty.
How Does Tetralogy of Fallot Occur?
The development of the heart starts at the 20th day of gestation. Tetralogy of Fallot occurs when a septum called bulbar septum develops. Bulbar separates the ascending aorta from the pulmonary artery and finally fuses with the interventricular septum. The Right ventricular outflow obstruction is most commonly subvalvular (infundibular) but can occur at any place: above the valve, below the valve, or mixed.
The infundibular part of the right ventricular outflow obstruction is dynamic and changes according to the stress level. In stress, subvalvular obstruction increases, driving a right-to-left shunt, resulting in profound hypoxemia (low oxygen in the blood), characterized by the cyanotic spell. In the presence of subvalvular obstruction, systemic vascular resistance decreases, increasing the right-to-left shunting and worsening the disease.
Pulmonary resistance is more common in infants than in adults. If pulmonary resistance increases, right ventricular outflow tract obstruction increases, resulting in a greater right-to-left shunt.
Causes & Risk Factors of Tetralogy of Fallot
Tetralogy of Fallot is a multifactorial disease. Some genetic studies reported that polymorphism of methylenetetrahydrofolate reductase (MTHR) may be involved in causing TOF. Polymorphism of gene VEGF is associated with an increased risk for TOF, while polymorphism of 936C>t is associated with a decreased risk for TOF.4Tetralogy of Fallot – Symptoms, diagnosis, and treatment | BMJ Best Practice. (n.d.). https://bestpractice.bmj.com/topics/en-gb/701
In addition, the tetralogy of Fallot is also associated with the CATCH22 characterized by:
- Cardiac defects
- Abnormal facies
- Thymic hypoplasia
- Cleft palate
- Hypocalcemia
- Deletion of chromosome 22q11
Risk Factors:
Some prenatal factors make a child more prone to have TOF.5Wilson, R. D., Ross, O., & Griksaitis, M. (2019). Tetralogy of Fallot. BJA Education, 19(11), 362–369. https://doi.org/10.1016/j.bjae.2019.07.003 These factors are:
- Maternal diabetes
- Rubella infection
- Medicine-induced (prenatal intake of retinoic acid)
- Smoking
- Genetic abnormalities (trisomy 13, 18, 21)
- Phenylketonuria
- Old age
- Alcohol use
What are the Symptoms of Tetralogy of Fallot?
The clinical presentation of TOF depends upon the severity of the disease. Neonates most commonly present with cyanosis soon after birth or later when the right ventricular outflow obstruction worsens. Symptoms of tetralogy of Fallot are:6Tetralogy of Fallot – Symptoms, diagnosis, and treatment | BMJ Best Practice. (n.d.). https://bestpractice.bmj.com/topics/en-gb/701
- Cyanosis (which can be gradual in onset and increases as the disease progresses)
- Low oxygen levels, even after oxygen therapy
- Presence of pan systolic and ejection systolic murmur
- Cyanotic spell: These spells most commonly occur during the morning or after crying
- Arrhythmias
Additionally, some other symptoms that are also associated with the TOF are:
- Fatigue
- Poor feeding
- Agitation
- Breathing difficulty
- Exercise intolerance
- Clubbing
- Heart failure
How to Diagnose Tetralogy of Fallot?
TOF should be diagnosed early to overcome its severity and complications. A complete history, physical examination, laboratory investigation, and imaging techniques are required to diagnose the TOF.
History:
In a detailed history, your doctor will ask multiple questions related to the disease, including:
- History of smoking, alcoholism, or maternal diabetes
- Have you had any infection before your delivery?
- Family history
- Socioeconomic status
Physical Examination:
In a physical examination, your doctor will inspect your chest to see if there is any abnormality. There is a bulging of the left anterior hemithorax due to right ventricular hypertrophy. However, on auscultation of the chest, there is a single first heart sound with a loud second heart sound. The frequency of murmur depends upon the degree of obstruction (the greater the block, the more the murmur), which is described as a harsh ejection systolic murmur. If there is a regurgitation of murmur, a systolic click can also be auscultated along the left eternal border. Pulse is usually regular.
Laboratory Investigations:
Some laboratory investigations that help diagnose TOF are:
- Complete blood count (CBC): The CBC of this patient shows markedly elevated red blood cell count depending on the level of oxygen in the blood
- Coagulation profile
- Arterial blood gasses (ABGs) to check oxygen saturation and lactate levels to check the severity of the disease
- White blood count to check for infections
- Blood sugar level to check for hypoglycemia
ECG:
Electrocardiography is the most common baseline investigation that helps rule out the other causes and functionality of the heart. ECG in these patients shows:
- Tall R wave in V1 showing Right ventricular hypertrophy (enlarged right ventricle) with right bundle branch block
- QRS Interval to check for arrhythmia
- Atrial fibrillation and atrial tachycardia
- Tall P wave (pulmonale) sign of right atrial enlargement
Cardiac Catheterization:
Cardiac catheterization is not usually required but can be advised when echocardiography cannot define the heart structure. It tells about the size, anatomy, and pressure inside the heart. In TOF, the findings of cardiac catheterization are:
- Increase pressure in the right ventricle
- Right ventricular hypertrophy
- Pulmonary hypertension
Imaging Investigations:
Imaging investigations, which include X-rays, echocardiography, and MRI, help your doctor visualize the internal structure of the heart and its anatomy.
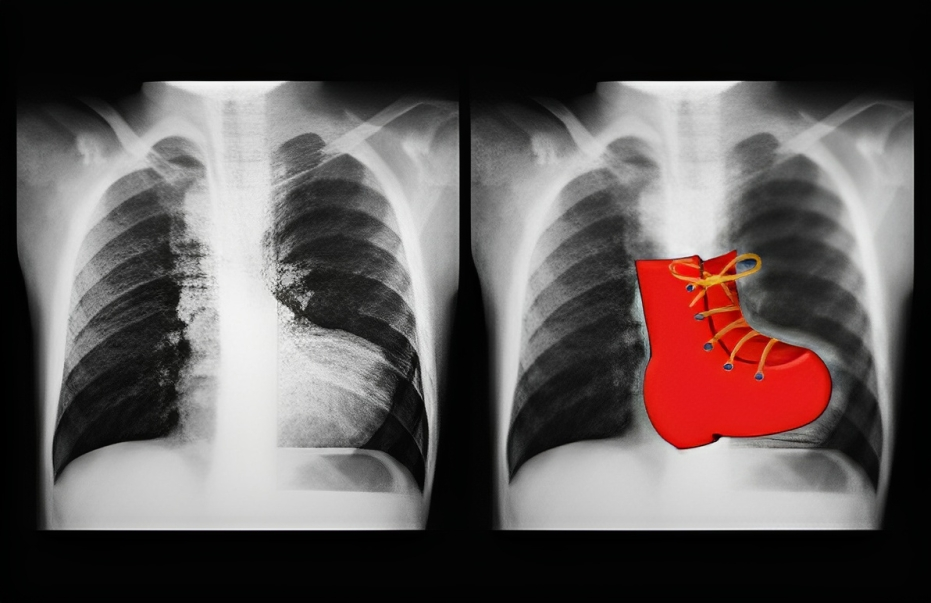
X-ray
It is one of the most basic first-line investigations. X-ray of a patient with TOF sometimes shows a normal heart appearance. However, the Cardinal feature of TOF in X-rays is a boot-shaped heart with reduced pulmonary vasculature. In 25% of the cases, the aortic arch is on the right side.
Echocardiography
Echocardiography is the investigation of choice for Tetralogy of fallot. It can reveal the internal structure of the heart, valves, and any defects in the heart.
Magnetic Resonance Imaging (MRI)
MRI is considered the gold standard investigation for tetralogy of Fallot. It gives the heart’s three-dimensional structure and also helps assess the function of the right ventricle, the size of the heart, and the pulmonary valve. MRI helps to assess the following things :
- The velocity of pulmonary regurgitation
- Size of the right ventricle
- Degree of right ventricular outflow tract obstruction
- Presence of ventricular septal defect
- The pressure gradient inside the head chambers
How to Treat Tetralogy of Fallot?
Neonates (Newborn babies) with TOF present with severe hypoxemia need urgent medical and surgical intervention to overcome the disease. Patients with severe right ventricular outflow obstruction need prostaglandin therapy until a definite surgical procedure is undertaken. However, in the case of dynamic right ventricular outflow obstruction, beta blockers are used to treat spells.
Treatment of Tet spell:
It is the most severe condition in which a neonate presents with a deteriorating situation and hemodynamic instability and needs emergency resuscitation by following the ABC (airway, breathing, and circulation) protocol. Spelling only occurs in children who have not undergone surgical repair and have closed patent ductus arteriosus. These are considered as high-risk patients. Some factors trigger the spelling episodes. These are:
- Exercise
- Anxiety and depression
- Feeding and dedication
- Crying
- Low oxygen level
- Acidosis
- Drugs that activate your sympathetic systems
- Hot baths
- During induction of anesthesia
It is important to avoid such risk factors even during surgery (induction of anesthesia).7Kannan B. R. (2008). Tetralogy of Fallot. Annals of pediatric cardiology, 1(2), 135–138. https://doi.org/10.4103/0974-2069.43880
Management of Hypercyanotic Spell:
Management of hyperchaotic spells is necessary and life-saving. It includes the following steps:
- Avoid any precipitating factors
- Calm the child
- Ask him to sit in knee-to-chest position
- High-flow oxygen therapy to maintain oxygen saturation
- Analgesia to treat pain (morphine and ketamine)
- Reduce PaCo2
- Beta-blockers (propranolol)
- Intravenous bicarbonate to avoid acidosis
- Fluid bolus to improve right ventricle filling
- Avoid giving beta-agonists (dopamine) because their drugs worsen the condition
- Ventilator support can also be required if oxygen Saturation is not going to normal
- Bacterial prophylaxis is necessary to avoid bacterial endocarditis
- Phlebotomy

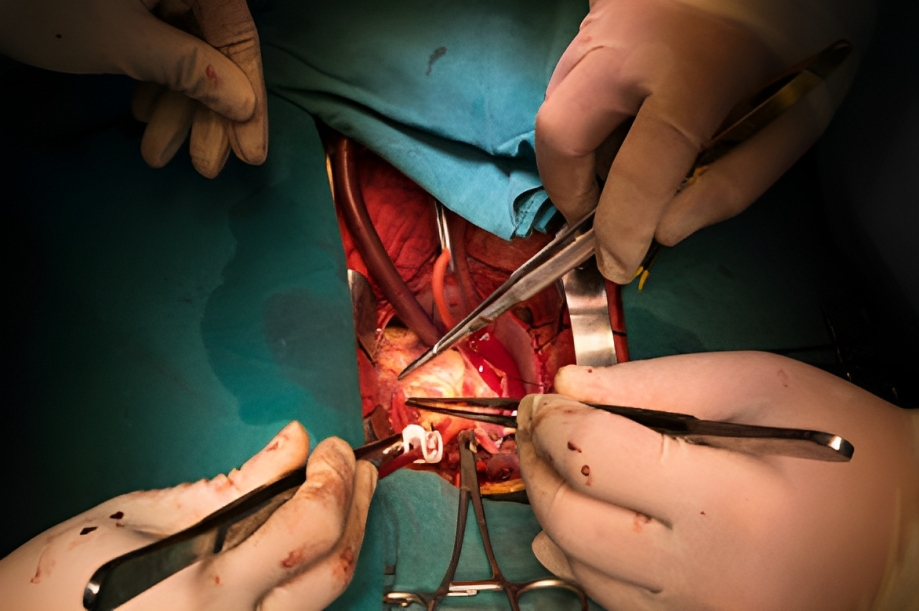
Surgical Intervention:
Complete surgical repair is the definitive treatment of tetralogy of Fallot. However, emergency surgeries can also be done to save the life of the patients. Surgical procedures that are used to treat TOF are:
Cardiac Catheter Intervention:
The surgeons recommend this surgery to patients who are not candidates for complete surgical repair. In this procedure, the surgeon inserts a catheter into the heart, which helps improve pulmonary blood flow. Another form of this procedure is pulmonary Volvomy. This procedure also allows for the stenting of patent ductus arteriosus (PDA).
Palliative Surgery (Shunting):
This surgical procedure is uncommon as most people choose complete surgical repair in one rather than a staged procedure. However, this surgical procedure is suitable for patients who are unfit for complete surgical repair. It included a Blalock-Taussig shunt,
which is a temporary surgical procedure in which the surgeon anastomoses the right subclavian artery with the pulmonary artery to improve pulmonary blood flow.
Corrective Surgery:
It is the most definite procedure for treating the tetralogy of Fallot.8Bedair, R., & Iriart, X. (2019). EDUCATIONAL SERIES IN CONGENITAL HEART DISEASE: Tetralogy of Fallot: diagnosis to long-term follow-up. Echo research and practice, 6(1), R9–R23. https://doi.org/10.1530/ERP-18-0049 This surgery involves the following interventions:
- Closure of ventricular septal defect
- Relief of the right ventricular outflow tract obstruction (through resection of obstructive muscle or using a transannular patch to widen the pulmonary valve or artery)
- Possible repair or widening of the pulmonary artery
What is the Prognosis of Tetralogy of Fallot?
Neonates with a more severe form of TOF present with deep cyanosis soon after birth, which can cause death of the patient. Infants who survive the first year of life have a better prognosis due to the formation of collateral vessels. The complete surgical repair is required in the second decade of life. Without surgical correction, the survival rate is decreased. Complete surgical repair before school age (6 years of age) has a good Prognosis, but sudden death can occur due to arrhythmias.
Complications of Tetralogy of Fallot
Several complications can occur due to Tetralogy of Fallot.9Diaz-Frias, J., & Guillaume, M. (2022, January 18). Tetralogy of Fallot. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK513288/ These are:
- Cerebral thrombosis
- Brain abscess
- Bacterial endocarditis
- Polycythemia
- Depression
- Anemia
Conclusion
To conclude, Tetralogy of Fallot is a congenital heart defect characterized by four cardinal features—newborns with TOF present with cyanosis and tet spells in the emergency department. Surgical interventions to correct this defect are critical as they improve a patient’s prognosis by 50%. If your newborn has cyanosis (skin turning blue), immediately consult your doctor for further evaluation and treatment. Delays in treatment can be fatal.
Refrences
- 1Bhimji, S., MD PhD. (n.d.). Tetralogy of Fallot (TOF) in Adults Treatment & Management: Approach considerations, Medical treatment, Surgical treatment. https://emedicine.medscape.com/article/2035949-treatment#d9?form=fpf
- 2Diaz-Frias, J. (2022, January 18). Tetralogy of Fallot. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK513288/
- 3Megha and Sakthivel V. “A case of pink tetralogy of Fallot.” International Journal of Contemporary Advanced Research, vol. 7, no. 1, 2018. DOI: http://dx.doi.org/10.24327/ijcar.2018.12981.2301
- 4Tetralogy of Fallot – Symptoms, diagnosis, and treatment | BMJ Best Practice. (n.d.). https://bestpractice.bmj.com/topics/en-gb/701
- 5Wilson, R. D., Ross, O., & Griksaitis, M. (2019). Tetralogy of Fallot. BJA Education, 19(11), 362–369. https://doi.org/10.1016/j.bjae.2019.07.003
- 6Tetralogy of Fallot – Symptoms, diagnosis, and treatment | BMJ Best Practice. (n.d.). https://bestpractice.bmj.com/topics/en-gb/701
- 7Kannan B. R. (2008). Tetralogy of Fallot. Annals of pediatric cardiology, 1(2), 135–138. https://doi.org/10.4103/0974-2069.43880
- 8Bedair, R., & Iriart, X. (2019). EDUCATIONAL SERIES IN CONGENITAL HEART DISEASE: Tetralogy of Fallot: diagnosis to long-term follow-up. Echo research and practice, 6(1), R9–R23. https://doi.org/10.1530/ERP-18-0049
- 9Diaz-Frias, J., & Guillaume, M. (2022, January 18). Tetralogy of Fallot. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK513288/