The reproductive apparatus possessed by women is subject to different complications. One health issue frequently associated with the female reproductive system is uterine fibroids, the global prevalence of which is estimated to range between 4.5% and 68.6%. 1Marsh, E. E., Al-Hendy, A., Kappus, D., Galitsky, A., Stewart, E. A., & Kerolous, M. (2018). Burden, prevalence, and treatment of uterine fibroids: a survey of US women. Journal of women’s health, 27(11), 1359-1367. If you are suffering from subserosal fibroids and fear what harm it might do to you, don’t worry; we are here to help!
What are Subserosal Fibroids?
A subserosal fibroid is a benign (non-cancerous) outgrowth that develops on the outer boundary of the womb. It is a type of uterine fibroids. Gynecologists also refer to fibroids as myomas and leiomyomas because these terms aptly define benign and tumorous growths within the muscle cells and smooth muscles. In addition to the linear pattern, myomas can also grow in nonlinear patterns. Furthermore, they can even undergo regression on their own. Subserosal Fibroids tend to be less symptomatic. However, depending on their size and location, they can still lead to pelvic pain, pressure, and heavy menstrual bleeding. Treatment is usually symptomatic and based on the patient’s condition. Surgical interventions might be necessary in some cases.
Types Of Uterine Fibroids
Uterine fibroids can be classified based on their location and attachment. The types are listed below:
Subserosal Fibroids
The uterus comprises multiple layers of soft tissues. A fibroid that forms in the uterus’s outer (subserous) layer is termed a subserosal fibroid. The subserosal layer is a thin outer covering primarily composed of epithelial cells. As these fibroids are located on the outer side, serious consequences from small growths are unlikely to be seen. Generally, subserosal fibroids do not lead to any serious complications. Hence, you don’t need to worry about pregnancy with fibroids.
Submucosal Fibroids
A submucosal fibroid is another variant of the uterine fibroids. It forms in the inner submucosal layer of the uterus. As they involve the inner layer of the uterus, submucosal fibroids are more likely to cause evident symptoms and interfere with fertility.2Gupta, S., Jose, J., & Manyonda, I. (2008). Clinical presentation of fibroids. Best practice & research Clinical obstetrics & gynaecology, 22(4), 615-626.
Intramural Fibroids
Present in the myometrium (muscle layer of the womb), intramural fibroids are the most common type of uterine fibroids. Therefore, they receive the highest medical attention. As they form inside the muscular layer, fibroids can grow into large sizes and stretch the uterus. Intramural and subserosal fibroids behave in a similar pattern.
Cervical Fibroids
Fibroids rarely develop near the vagina. In rare cases, a fibroid can develop at the connection point between the uterus and vagina, i.e., the cervix. Such fibroids are termed cervical fibroids.
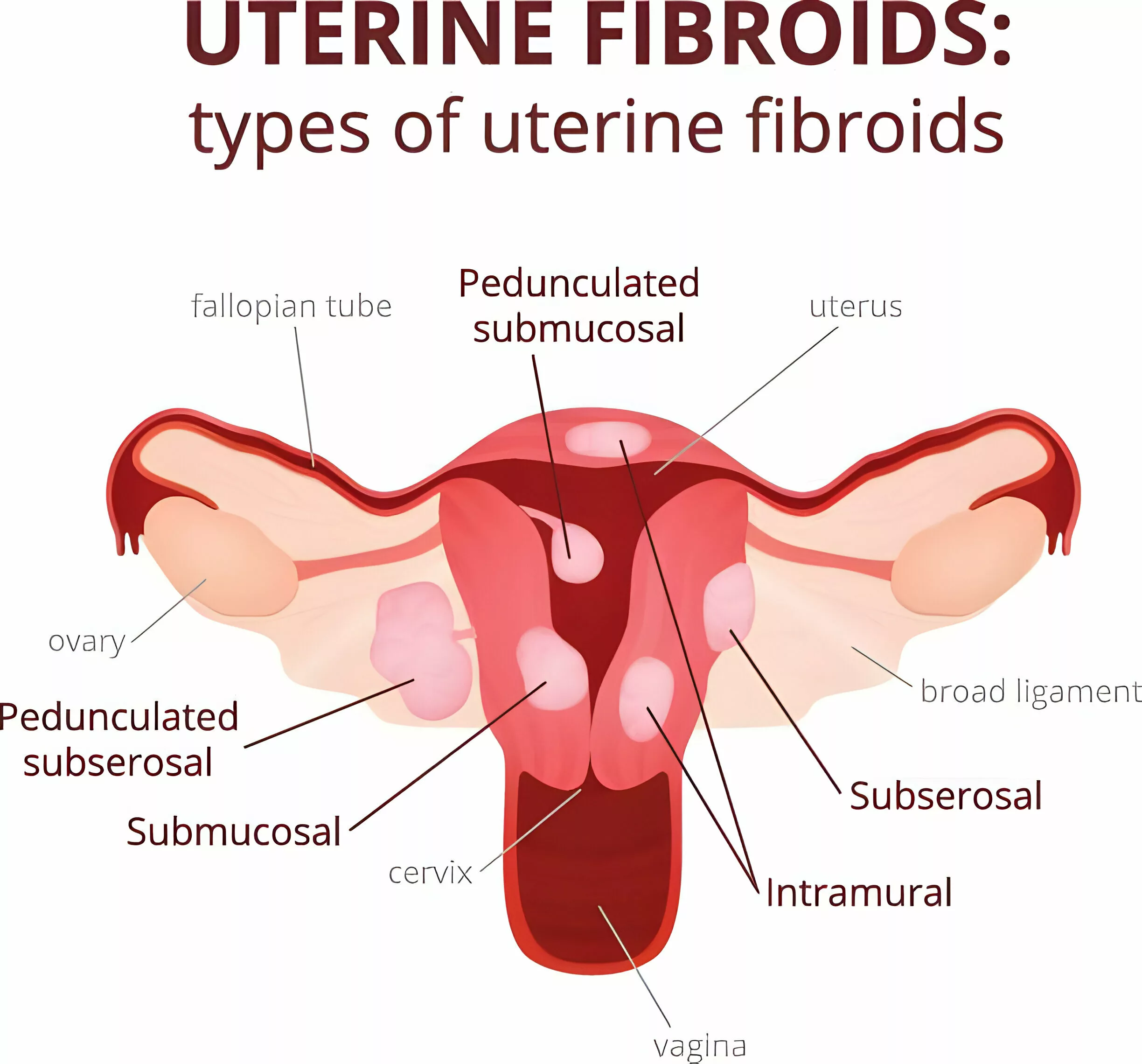
Subserosal Fibroid Types
Based on the attachment to the subserosal layer, a subserosal fibroid can be classified as:
- Non-Pedunculated Fibroid: It attaches directly to the outer side of the uterus.
- Pedunculated Subserosal Fibroid: It attaches to the outside of the uterus via a stem/peduncle. Preoperative diagnosis of a pedunculated fibroid is necessary.3Le, D., Dey, C. B., & Byun, K. (2020). Imaging findings of a torsed pedunculated uterine leiomyoma: A case report. Radiology Case Reports, 15(2), 144-149.
Age Of Onset
Middle-aged women (30 and 40 years) encounter subserosal fibroids more than women of other age groups. The probability of subserosal fibroids increases with age until menopause. However, most fibroids shrink after the onset of menopause.
Symptoms Of Subserosal Fibroids
Subserosal fibroids are asymptomatic in the majority of cases. Patients are unaware that they are suffering from a subserosal fibroid. Small fibroids are mostly silent and do not have any presentation. When present, the symptoms depend on multiple factors, including:
- Number of fibroids
- Size of the fibroid(s)
- Location of the fibroid
Patients report the following symptoms:
Heavy Menstrual Bleeding & Clots
Small subserosal fibroids do not contribute to heavy bleeding. However, a large-sized subserosal fibroid can cause significant menstrual bleeding with blood clots discharge. Experts suggest that the hyper-sized subserosal fibroids exert pressure on the endometrium and promote wall shedding. A uterine fibroid also vascularizes the endometrial layer of the uterus, leading to increased bleeding. While uterine fibroids contribute to abnormal uterine bleeding, period irregularities are rarely seen with subserosal fibroids.
Abdominal Cramping
Several women experience cramping during their periods. Menstrual cramps with fibroids are more pronounced and felt in the lower abdomen. The condition of pain during the menstrual cycle is termed dysmenorrhea. Dysmenorrhea is a symptom present in 30% of patients having uterine myomas.4Khyade, R. L. (2017). A study of menstrual disturbance in cases of fibroid uterus. International Journal of Reproduction, Contraception, Obstetrics and Gynecology, 6(6), 2494-2498. Large-sized subserosal fibroids contribute to pressure on the abdomen, which induces cramping.

Pelvic Pain
Subserosal fibroids rarely cause any symptoms until they become large enough. Cross-sectional surveys reveal that around 64% of women with uterine fibroids experience moderate-to-severe symptoms.5Hervé, F., Katty, A., Isabelle, Q., & Céline, S. (2018). Impact of uterine fibroids on quality of life: a national cross-sectional survey. European Journal of Obstetrics & Gynecology and Reproductive Biology, 229, 32-37. Symptomatic management of large subserosal fibroids targets reductions in bleeding and pelvic pain. In some cases, pelvic pain is accompanied by back pain. Uterine fibroids exert additional weight on the pelvis. This leads to discomfort and pain. Cervical fibroids directly affect a patient’s sex life. Many women report having pain during intercourse. However, subserosal fibroids do not induce pain during sex, nor do they interfere with fertility.
Abdominal Fullness
Many subserosal fibroid patients experience a feeling of abdominal enlargement and report a persistent feeling of tummy fullness. The enlarged masses (fibroids) distend the abdomen, leading to sensations of bloating and fullness. As subserosal fibroids are present on the outer layer of the uterus, the distention of the abdomen is noticeable. Though rare, a supersized fibroid may even lead to intra-abdominal hemorrhage.
Frequent Urination & Constipation
Subserosal fibroids put extra pressure on the bladder and the bowel. The additional weight on the bladder makes you lose control of the sphincters. Therefore, large symptomatic subserosal fibroids present with lower urinary tract symptoms. Similarly, the pressure on your intestines can interfere with normal bowel movements, leading to constipation.
Link Between Subserosal Fibroids & Fertility
The greatest complication associated with uterine fibroids is difficulty in conception. Women of childbearing age report a lack of conception and pregnancy without proper treatment. In the past, clinicians believed that all the fibroid types have some effect on pregnancy rates with and without surgical treatment. However, newer research states that subserosal myomas/fibroids have little to no effect on the fertility of a female. Researchers believe that functional changes induced by fibroids in the myometrium and endometrium lead to fertility issues. As subserosal fibroids are located on the outside of the womb, direct influence on fertility is absent.6Zepiridis, L. I., Grimbizis, G. F., & Tarlatzis, B. C. (2016). Infertility and uterine fibroids. Best Practice & Research Clinical Obstetrics & Gynaecology, 34, 66-73.Therefore, you can get pregnant with a subserosal fibroid, but it’s better to get treatment as soon as possible to avoid complications.
Causes Of Subserosal Fibroids
Doctors are unclear about the definitive cause of a subserosal fibroid. Leading clinicians identify a genetic predisposition in most cases. Based on clinical observation, the following plausible explanations are available for subserosal fibroid development:
Family History
Uterine myomas and leiomyomas run in families. There is a high risk of subserosal fibroids if your mother or grandmother had it.
Hormonal Imbalance
Ovaries are the main reproductive structures that produce hormones like progesterone and estrogen. In cases of hormonal imbalance, estradiol and progesterone can lead to fibroid development. Therefore, ovarian blockage and restoration of hormone levels can lead to sufficient arrest of myoma growth.
Risk Factors for Subserosal Fibroids
There are several factors that can increase your risk of developing uterine fibroids. These factors include:
- Age (30 years plus)
- Ethnicity (Black women)
- Premenopausal state
- Hypertension
- Family history
- Time since the last conception
- Use of food additives
- Soybean milk consumption
- Use of oral/injectable contraceptives
- Smoking
- High Body mass index
So, if you are a black woman of 30 years or more and have a family history of fibroids and high body weight (overweight/obese), you likely will develop subserosal fibroids.
Diagnosis Of Subserosal Fibroids
The vast majority of subserosal fibroids remain asymptomatic. You might discover them during a routine checkup at the gynecologist’s office. An ultrasound reveals the presence of silent subserosal fibroids. The diagnostic protocol usually involves:
History & Physical Examination:
When symptoms are present, the gynecologist takes a complete history of the patient, followed by a physical examination. During a physical exam, subserosal fibroids may be palpable as firm masses in the lower abdomen. These fibroids can sometimes cause pelvic tenderness or pressure, and in some cases, they may be associated with changes in the size or shape of the uterus.
Diagnostic Imaging:
Imaging studies, such as ultrasound or MRI, are often used to confirm the presence of subserosal fibroids and evaluate their size, location, and impact on surrounding structures. Ultrasound is an imaging test involving high-frequency sound waves to visualize structures. Sometimes, gynecologists also advise a transvaginal ultrasound (TVS). On ultrasound, a subserosal fibroid appears as a round and concentric mass of growth present on the wall of the uterus. Small subserosal fibroids are well-demarcated and resemble grapefruits. Often, the subserosal fibroid is attached to the uterus through a stalk (pedunculated fibroid), which is appreciable on the radiograph/ultrasound. This is a unique feature of the subserosal fibroid that makes it distinct from other types. Multiple small fibroids can range from 5 mm to 5 cm in diameter. Or there can be a subserosal fibroid as large as 10 cm or more.
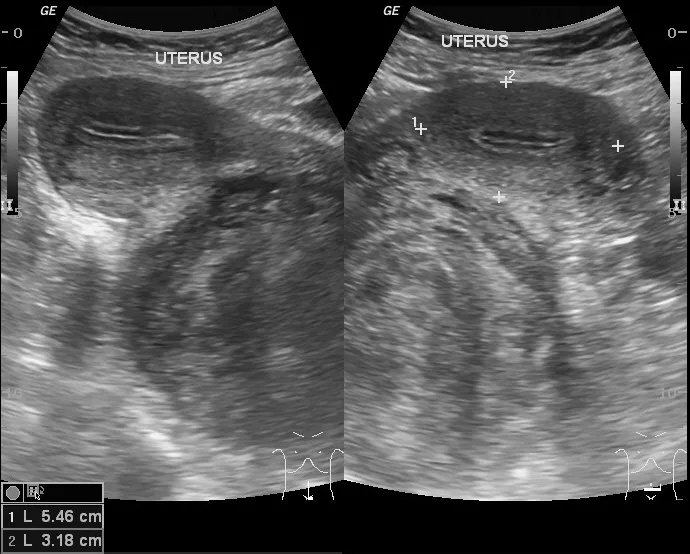
Case courtesy of Maulik S Patel, Radiopaedia.org. From the case rID: 12850
Your doctor may go for a pelvic MRI or a CT scan to get an in-depth picture of the uterus and the ovaries. Your healthcare provider correlates the clinical examination with imaging to reach a diagnosis.
Subserosal Fibroids Treatment
Multiple strategies exist to manage and treat subserosal fibroids. Treatment has two aspects: symptomatic management and regression/elimination of the fibroids. After correlating the findings of the physical examination and ultrasound reports with the patient’s symptoms, the doctor decides which treatment modality is best.
Medicines:
Pharmacological management is effective for most small to moderate-sized subserosal myomas. There are medicines for symptomatic management and remission of the fibroids.
Symptomatic Management
Gynecologists generally prescribe over-the-counter painkillers for pelvic/back pain. While NSAIDs (Ibuprofen/Naproxen) provide pain relief, antispasmodic drugs (mebeverine, etc.) reduce abdominal cramping. Your doctor might advise you to take a birth control pill to decrease menstrual bleeding. Progestin (hormone)–releasing intrauterine devices (IUDs) may also be placed to decrease blood loss.
Gonadotropin-releasing Hormone Agonists (GnRH) Agonists
GnRH agonist drugs (such as leuprolide acetate) shrink subserosal fibroids by blocking the production of FSH (follicle-stimulating hormone) and luteinizing hormone (LH). This blockage eventually stops menstruation (by dropping progesterone and estrogen levels in the blood) and thus shrinks fibroids. GnRH agonists have proven to be effective in shrinking fibroids.7Ciebiera, M., Madueke-Laveaux, O. S., Feduniw, S., Ulin, M., Spaczyński, R., Zgliczyńska, M., … & Al-Hendy, A. (2023). GnRH agonists and antagonists in therapy of symptomatic uterine fibroids–current roles and future perspectives. Expert Opinion on Pharmacotherapy, 24(16), 1799-1809.
Minimally Invasive Procedures:
The next step for small-to-moderate subserosal fibroid treatment includes multiple minimally invasive procedures:
Uterine Fibroid Embolization (UFE)
The surgeon cuts off the blood supply to the fibroid by injecting small particles into the uterine artery. It reduces pedunculated subserosal fibroid size with minimal adverse effects.
Radiofrequency Ablation
A radiofrequency device emitting high-energy radio waves is placed within the fibroid, generating heat that destroys fibroids. A similar myolysis (Acessa) procedure shrinks fibroids by laser or heat, while cryo-myolysis works by freezing the fibroids.
Magnetic Resonance Guided Focused Ultrasound (MRgFUS)
The patient is placed in an MRI machine, and high-intensity ultrasound waves are directed at the subserosal fibroids to destroy them by heat. It offers immediate symptomatic relief and quick recovery.
Surgical Treatment:
Surgery is reserved for large-sized fibroids that do not respond to conventional therapies.
Myomectomy
In this procedure, the surgeon removes fibroids from the uterus. It can be done with the conventional open method (large incision) or via a few small incisions, smart surgical tools, and a camera (laparoscopic myomectomy). However, a recurrence of fibroids can occur in this surgery.
Hysterectomy
In severe unresolvable cases, the surgeon opts to remove parts of the uterus (subtotal) or the whole uterus (total hysterectomy). You will lose your fertility after a hysterectomy. Thus, hysterectomy is only reserved for patients with complicated subserosal fibroids that decrease the quality of life. Some patients prefer to try home remedies or complementary medicine to heal fibroids. Acupuncture, yoga, and massage therapy have some positive effects, but you should consult your doctor before opting for them.
How To Prevent Subserosal Fibroids?
Women in the risk factor group can prevent fibroids by taking care of their vitamin D levels. Research suggests a link between low serum vitamin D levels and the occurrence of subserosal fibroids. Some studies even suggest that vitamin D supplementation leads to a reduction in the size of leiomyomas.8Hajhashemi, M., Ansari, M., Haghollahi, F., & Eslami, B. (2019). The effect of vitamin D supplementation on the size of uterine leiomyoma in women with vitamin D deficiency. Caspian journal of internal medicine, 10(2), 125. Ladies at a higher risk must have routine gynecological checkups to prevent undiagnosed subserosal fibroids. This is important because most small-to-moderate subserosal fibroids go undiagnosed until they become humongous.
Final Word
In conclusion, subserosal fibroids, commonly found in women between 30 and 40 years old, typically remain asymptomatic but can cause symptoms such as heavy menstrual bleeding, abdominal enlargement, and pelvic discomfort when they grow large. Treatment options range from over-the-counter painkillers to minimally invasive procedures like uterine fibroid embolization (UFE), endometrial ablation, or MRgFUS. In severe cases, surgical interventions such as myomectomy or hysterectomy may be necessary to alleviate symptoms and improve quality of life.
Refrences
- 1Marsh, E. E., Al-Hendy, A., Kappus, D., Galitsky, A., Stewart, E. A., & Kerolous, M. (2018). Burden, prevalence, and treatment of uterine fibroids: a survey of US women. Journal of women’s health, 27(11), 1359-1367.
- 2Gupta, S., Jose, J., & Manyonda, I. (2008). Clinical presentation of fibroids. Best practice & research Clinical obstetrics & gynaecology, 22(4), 615-626.
- 3Le, D., Dey, C. B., & Byun, K. (2020). Imaging findings of a torsed pedunculated uterine leiomyoma: A case report. Radiology Case Reports, 15(2), 144-149.
- 4Khyade, R. L. (2017). A study of menstrual disturbance in cases of fibroid uterus. International Journal of Reproduction, Contraception, Obstetrics and Gynecology, 6(6), 2494-2498.
- 5Hervé, F., Katty, A., Isabelle, Q., & Céline, S. (2018). Impact of uterine fibroids on quality of life: a national cross-sectional survey. European Journal of Obstetrics & Gynecology and Reproductive Biology, 229, 32-37.
- 6Zepiridis, L. I., Grimbizis, G. F., & Tarlatzis, B. C. (2016). Infertility and uterine fibroids. Best Practice & Research Clinical Obstetrics & Gynaecology, 34, 66-73.
- 7Ciebiera, M., Madueke-Laveaux, O. S., Feduniw, S., Ulin, M., Spaczyński, R., Zgliczyńska, M., … & Al-Hendy, A. (2023). GnRH agonists and antagonists in therapy of symptomatic uterine fibroids–current roles and future perspectives. Expert Opinion on Pharmacotherapy, 24(16), 1799-1809.
- 8Hajhashemi, M., Ansari, M., Haghollahi, F., & Eslami, B. (2019). The effect of vitamin D supplementation on the size of uterine leiomyoma in women with vitamin D deficiency. Caspian journal of internal medicine, 10(2), 125.