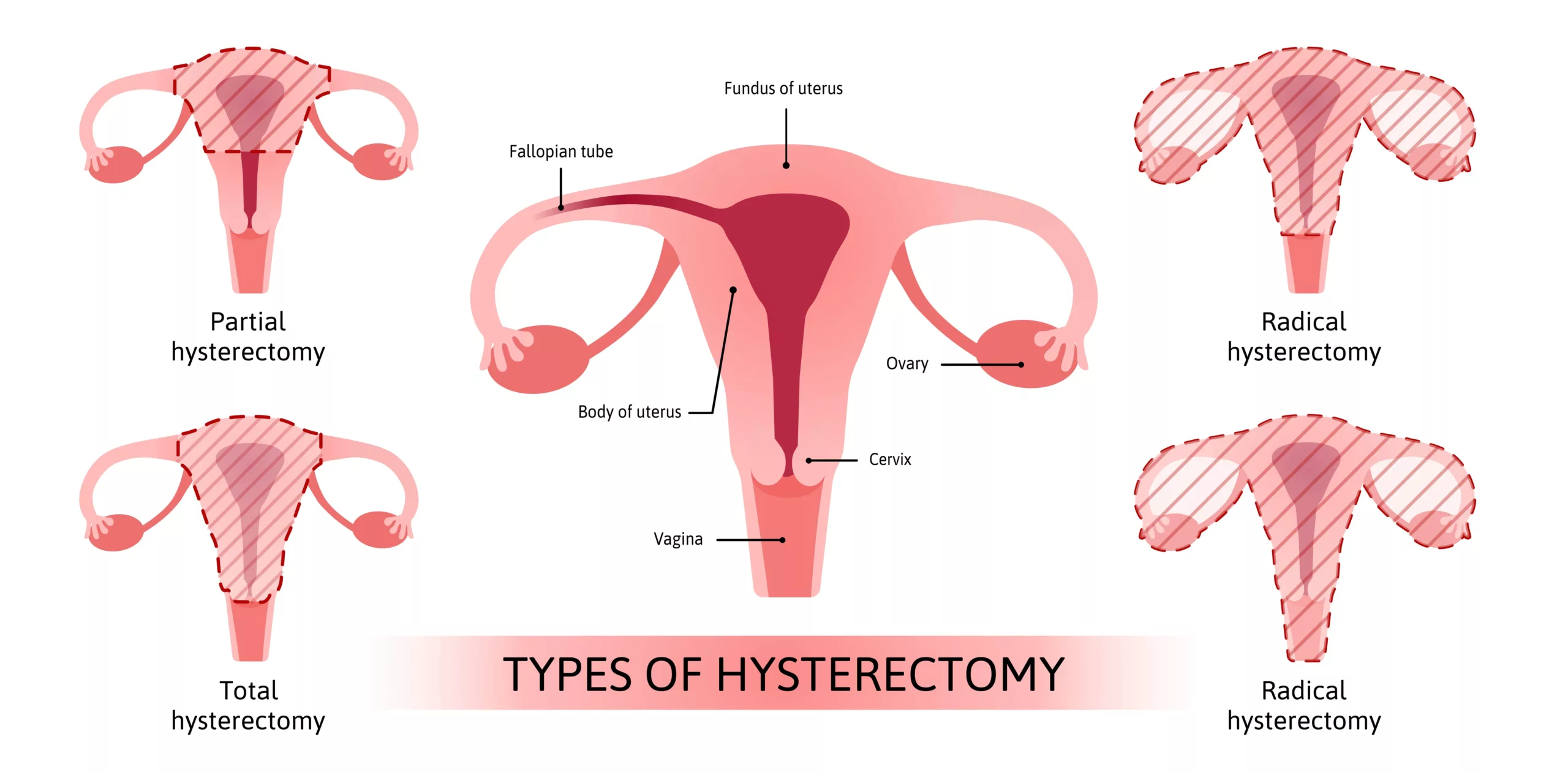
Hysterectomies are one of the most common surgical procedures undergone by women. They refer to the surgical removal of a uterus.1Pillarisetty LS, Mahdy H. Vaginal Hysterectomy. [Updated 2023 Apr 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK554482/ The type of hysterectomy used depends on various factors, including the patient’s medical condition, the reason for the procedure, and the extent of the treatment needed. The options include total hysterectomy (removing the uterus and cervix), subtotal hysterectomy (removing only the uterus), and radical hysterectomy (removing the uterus, cervix, and surrounding tissues). The choice is made based on each patient’s specific needs and circumstances.
What Is a Partial Hysterectomy?
Partial Hysterectomy involves the removal of the uterus but not the cervix. Surgeons commonly prescribe this type of hysterectomy for various conditions like uterine fibroids, cancer treatment, and abnormal bleeding. It’s also known as a subtotal or supracervical hysterectomy.
During a hysterectomy, the surgeon may opt to remove additional organs, such as the fallopian tubes and ovaries. This concurrent removal of the fallopian tubes, known as opportunistic salpingectomy, can significantly reduce a woman’s risk of ovarian cancer.
Following the removal of the uterus and any accompanying organs, regardless of the hysterectomy type, menstrual periods cease entirely. Consequently, the woman loses her ability to conceive or carry a pregnancy to term.
Indications For A Partial Hysterectomy
Doctors prescribe partial hysterectomies after other less invasive treatment modalities have failed. The general indications include:
- Endometriosis: It is a condition where uterine-like tissue grows outside the Uterus.
- Fibroids: These are non-cancerous uterine growths that may cause pain, pressure, and bleeding.
- Ovarian or uterine cancer.
- Abnormal uterine bleeding(Menorrhagia)– Refers to menstrual bleeding occurring for more than seven days. Excessive uterine bleeding can lead to anemia. This can result in fatigue and decreased quality of life.
- Chronic pelvic pain, especially due to prolapse– Prolapse is due to weakening pelvic muscles and ligaments. This may be due to previous vaginal deliveries.
However, women with abnormal pap smears or a diagnosis of reproductive cancer are not good candidates for the procedure. As the cervix is still intact after the procedure, women should still undergo regular cancer screenings(pap smears).
Difference Between a Partial & a Total Hysterectomy
A Partial hysterectomy removes part of the uterus, preserving the cervix. On the other hand, total hysterectomies involve the complete removal of the uterus and cervix. Total hysterectomies are more common than partial hysterectomies.
Advantages Of A Partial Hysterectomy Over Total Hysterectomy
There are many advantages of partial(supracervical) hysterectomies over total hysterectomies. Partial hysterectomies offer quicker recovery, less pain, and minimal scarring. If the surgeon spares the ovaries, there is no need for hormone replacement therapy. Additionally, supracervical hysterectomies reduce vaginal dryness because they preserve the cervical glands. Total hysterectomies have longer recovery time, greater scarring, and are generally more invasive. They are also more likely to lead to vaginal dryness.
Disadvantages Of A Partial Hysterectomy Over Total Hysterectomy
Supracervical(partial) hysterectomies require special instruments that may not be available in every setting. Moreover, the surgeon may even have to switch to a total hysterectomy if the size of the pathology is huge. Lastly, contrary to popular belief, studies have not reported improved sexual function in supracervical hysterectomies when compared to other surgical treatment modalities.2Thakar R, Ayers S, Clarkson P, Stanton S, Manyonda I. Outcomes after total versus subtotal abdominal hysterectomy. N Engl J Med. 2002;347(17):1318-1325. doi:10.1056/NEJMoa013336 Improved surgical outcomes have not been reported for partial vs total hysterectomies.3Lethaby A, Mukhopadhyay A, Naik R. Total versus subtotal hysterectomy for benign gynecological conditions. Cochrane Database Syst Rev. 2012;(4): CD004993. Published 2012 Apr 18. doi:10.1002/14651858.CD004993.pub3
What Are The Surgical Approaches To Partial Hysterectomies?
Various surgical approaches can be employed for a partial hysterectomy, and the choice depends on factors such as the medical condition, cancer stage, uterine size, overall health, and individual considerations.4Partial Hysterectomy. moffitt. Accessed December 19, 2023. https://www.moffitt.org/treatments/surgical-care/partial-hysterectomy-for-gynecological-cancers/ The main approaches to hysterectomy are:
- Abdominal Approach
- Vaginal Approach
- Laparoscopic hysterectomy
Abdominal Hysterectomy involves removal of the uterus through incisions in the lower abdomen. The ovaries and fallopian tubes may be spared during this procedure.
Vaginal approaches are suitable for early-stage cancers and involve the removal of an unenlarged uterus through a vaginal incision.
The laparoscopic approach is minimally invasive. In this approach, surgeons make small incisions in the belly button and abdominal area. They insert a tiny light, a camera (Laproscope), and specialized instruments through these incisions. The surgeon then views the uterus on an external video screen, facilitating its removal.
How Are Partial Hysterectomies Performed?
Before undergoing a partial hysterectomy, patients can expect to undergo preoperative assessments, including blood tests, imaging scans, and discussions about the procedure and recovery process. Additionally, patients may receive instructions regarding dietary restrictions, medication adjustments, and preoperative lifestyle modifications to optimize their health before surgery. Clear communication with healthcare providers and adherence to preoperative guidelines are crucial to ensure a successful outcome and smooth recovery.
Medical staff may administer enemas or laxatives on the day of surgery to empty the bowel. Patients are instructed not to consume food or drink for at least 12 hours before surgery. Bladder catheterization is performed; typically, the catheter is removed a day after surgery.
The Procedure:
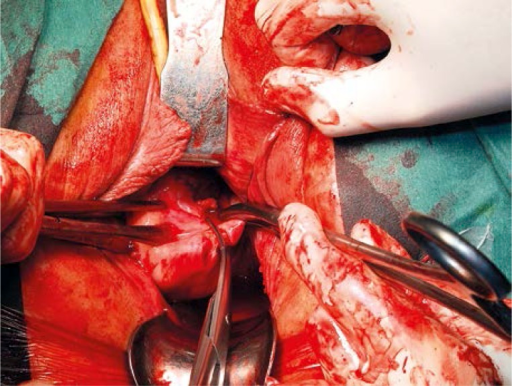
Abdominal Route
In this approach, after general anesthesia, the surgeon makes a 6 to 8-inch incision in the lower abdomen. This is either a vertical incision extending from below the bellybutton to above the pubic bone or a horizontal bikini-line incision, which is an inch above the pubic bone. After developing the visual field, surgeons begin dissecting the ligaments to allow for the removal of the uterus.
Following the procedure, most patients typically remain hospitalized for 2-3 nights, requiring 4-6 weeks of reduced activity during recovery.5NHS Choices. How it’s performed – Hysterectomy. NHS. Published 2019. https://www.nhs.uk/conditions/hysterectomy/what-happens/
Vaginal Route
The surgical team positions the patient in the lithotomy position and administers anesthesia. A solution of 0.9% NaCl and adrenaline is injected into the vaginal portion of the cervix to minimize bleeding. Surgeons then proceed with anterior and posterior colpotomies, which involve making incisions in the vaginal wall. To prevent injury, the patient’s bladder is elevated and dissected.
The surgeon then delivers the uterine body through the anterior colpotomy and guides the cervix into the peritoneal cavity through the posterior colpotomy. Subsequently, supracervical amputation of the uterus is performed. After the uterus is removed, the cervix is returned to its normal position. Finally, continuous suturing is performed to close the wound and colpotomies, and a vaginal pack may be inserted for additional support.6Wilczyński M, Cieślak J, Malinowski A. Supracervical hysterectomy – the vaginal route. Wideochir Inne Tech Maloinwazyjne. 2014;9(2):207-212. doi:10.5114/wiitm.2014.41633
Laparoscopic Route
The patient is first anesthetized before the laparoscopic procedure begins. Surgeons create small incisions in the abdomen, through which they insert instruments and laparoscopic ports. Upon gaining access, the surgical team conducts a thorough examination of the patient’s pelvis and abdomen.
The surgeon focuses on identifying the anatomy of the ureters, assessing the presence of any disease, and evaluating the feasibility of the procedure. After achieving appropriate access, the surgeon dissects the utero-ovarian, round ligament, and broad ligament.
Following this, they carefully separate the vesicouterine peritoneum from the anterior uterus, utilizing cautery as necessary to control bleeding. Subsequently, the surgeon detaches the uterus from the cervix and removes it through one of the incisions.7Jenkins TR. Laparoscopic supracervical hysterectomy. Am J Obstet Gynecol. 2004;191(6):1875-1884. doi:10.1016/j.ajog.2004.06.096 The patient will then be sutured and dressed.
What To Expect After The Procedure?
After the procedure, patients can expect to receive prescriptions for antibiotics and dietary recommendations aimed at facilitating recovery and preventing infections. Also, medical advice typically includes avoiding heavy lifting or strenuous activities for up to six weeks post-surgery. During the initial week following the procedure, healthcare providers advise patients to limit standing to no more than 30 minutes at a time to promote healing and minimize discomfort. These precautions are essential for ensuring a smooth and successful recovery process.
What Is The Recovery Time For Partial Hysterectomies?
Compared to open hysterectomies, patients with supracervical hysterectomies recover quickly. In laparoscopic supracervical hysterectomy, patients may be discharged on the same day. The recovery time is around 2-3 weeks.
Complications Of Partial Hysterectomy
As this is a surgical procedure, there may be post-operative hemorrhage(bleeding), infections, blood clots, and pain. Other complications include damage to nearby structures such as the ureter, bladder, intestine, etc. There may also be fistula formation between the bladder and the vagina. A fistula is an abnormal opening between two structures. Removal will lead to early menopause and symptoms like hot flashes and mood swings.
Is It Possible To Become Pregnant After Partial Or Total Hysterectomy?
Partial hysterectomies lead to infertility. However, there have been cases of partial hysterectomy performed for gestational cancers while preserving fertility. Some of these women later on had live births.8Cheng B, Liu ZX, Zhou W, Qian JH. Fertility-sparing partial hysterectomy for gestational trophoblastic neoplasia: an analysis of 36 cases. J Reprod Med. 2014;59(5-6):274-278.However, it is not possible to become pregnant after a partial or total hysterectomy. Since the uterus is removed, there is no place for a fertilized egg to implant and develop, making pregnancy impossible.9Fader AN, Mansuria S, Guido RS, Wiesenfeld HC. A 14-week abdominal pregnancy after total abdominal hysterectomy. Obstet Gynecol. 2007;109(2 Pt2):519-521. doi:10.1097/01.AOG.0000243774.14606.64
In summary, a partial hysterectomy effectively treats various gynecological conditions while preserving the cervix and, in some cases, the ovaries. Although it does not preserve reproductive function, as the uterus is removed, with proper care and follow-up, this procedure can provide relief and improve the quality of life for many women.
Refrences
- 1Pillarisetty LS, Mahdy H. Vaginal Hysterectomy. [Updated 2023 Apr 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK554482/
- 2Thakar R, Ayers S, Clarkson P, Stanton S, Manyonda I. Outcomes after total versus subtotal abdominal hysterectomy. N Engl J Med. 2002;347(17):1318-1325. doi:10.1056/NEJMoa013336
- 3Lethaby A, Mukhopadhyay A, Naik R. Total versus subtotal hysterectomy for benign gynecological conditions. Cochrane Database Syst Rev. 2012;(4): CD004993. Published 2012 Apr 18. doi:10.1002/14651858.CD004993.pub3
- 4Partial Hysterectomy. moffitt. Accessed December 19, 2023. https://www.moffitt.org/treatments/surgical-care/partial-hysterectomy-for-gynecological-cancers/
- 5NHS Choices. How it’s performed – Hysterectomy. NHS. Published 2019. https://www.nhs.uk/conditions/hysterectomy/what-happens/
- 6Wilczyński M, Cieślak J, Malinowski A. Supracervical hysterectomy – the vaginal route. Wideochir Inne Tech Maloinwazyjne. 2014;9(2):207-212. doi:10.5114/wiitm.2014.41633
- 7Jenkins TR. Laparoscopic supracervical hysterectomy. Am J Obstet Gynecol. 2004;191(6):1875-1884. doi:10.1016/j.ajog.2004.06.096
- 8Cheng B, Liu ZX, Zhou W, Qian JH. Fertility-sparing partial hysterectomy for gestational trophoblastic neoplasia: an analysis of 36 cases. J Reprod Med. 2014;59(5-6):274-278.
- 9Fader AN, Mansuria S, Guido RS, Wiesenfeld HC. A 14-week abdominal pregnancy after total abdominal hysterectomy. Obstet Gynecol. 2007;109(2 Pt2):519-521. doi:10.1097/01.AOG.0000243774.14606.64





