Esophageal Manometry is a procedure for evaluating the pressure and motility of the esophagus. It uses a probe and sensors to detect pressure and movement in the esophagus. It is the gold standard for diagnosing esophageal motility disorders like achalasia, gastroesophageal reflux disease, and hypo- or hypercontractile esophagus.
What Is Esophageal Manometry?
Esophageal Manometry is a procedure in which your doctor evaluates the pressure and movements of the esophagus to diagnose the motility disorders of your esophagus. The doctor passes a tube from your nose to the esophagus; it has probes and pressure sensors along with it. The probes sense the pressure and contractions in your esophagus as you swallow water, and the software converts these measurements into pressure values and graphs later. It was performed for the first time in 1950.
Indications Of Esophageal Manometry
There are the following indications of esophageal manometry:
- Dysphagia (Difficulty in swallowing)
- Odynophagia (Painful Swallowing)
- Gastroesophageal reflux disease (GERD)
- Non-cardiac chest pain
- Work up for the diagnosis of any pathology of the esophagus
- For diagnosis of motility disorders of the esophagus
- Regurgitation of food
- Achalasia
- Hoarseness of voice
- Nutcracker esophagus
- Esophageal spasm
- Evaluation of the patient before any surgery like anti-reflux or esophageal surgery
- Choking or coughing on food intake
- Evaluation of symptoms like burping, bloating, and chest burning
- Evaluation of esophageal function in patients with lupus, scleroderma, systemic lupus erythematosus (SLE), Parkinson’s disease, or stroke.
How To Prepare A Patient For Esophageal Manometry?
Preparation of a patient for esophageal manometry involves the following steps:
History
Before esophageal manometry, your doctor may ask the following history questions:
- Do you have symptoms like regurgitation, chest pain, or heartburn, and since when have you developed these symptoms? What is the frequency of these symptoms?
- Do you have difficulty swallowing solids and liquids or discomfort while swallowing food?
- Do you have recent weight loss gastroesophageal reflux disease (GERD) or acid brash?
- Do you have a history of previous surgery? Are you taking any medication?
- Your doctor may ask about the history of voice changes, smoking, alcohol intake, and food habits.
Examination
Your doctor performs your complete medical and physical examination before doing esophageal manometry. Your doctor may thoroughly assess your nutritional status. They might also check your weight and body mass index before the procedure.
Laboratory Investigations
Laboratory investigations before esophageal manometry include the following:
- Complete blood count
- Urine analysis
- Lipid profile
- Echocardiography
- Lung function tests
- Kidney function tests
- Infection screening
Informed Consent
Your doctors will counsel you about the complete procedure of esophageal manometry. After telling you about the steps of the procedure and the associated risks, they will ask you to sign a consent form as proof.
What Precautions Should You Follow Before Esophageal Manometry?
Your doctor will counsel you about the Dos and Don’ts before the surgery, as well as the diet and medication you need to take.
- Tell your doctor all the relevant history correctly.
- Your doctor will ask you to fast for at least 6 hours before the procedure, so don’t eat or drink a whole meal before your procedure.
- Avoid belching or burping 24 before the procedure.
- If you need to drink water, only take a small sip.
- Do not take meals or drinks.
- The doctors take precautions to minimize the perforation risk and ensure infection control.
- Avoid smoking or alcohol 24 hours before the surgery.
- Avoid medicines like nitrates, opioids, calcium channel blockers, or antidepressants.
Step-by-Step Procedure Of Esophageal Manometry
Preparation & Positioning
Your doctor asks you to arrive at the hospital on the day of the test, after consent, they ask you to remove any dentures.
Then, they apply topical anesthetic like lidocaine in the nose and throat to reduce discomfort during the procedure.
They position you comfortably, usually sitting upright or lying with your head elevated.
During the procedure, they apply vitals monitors such as a pulse oximeter, BP apparatus, and electrocardiography (ECG).
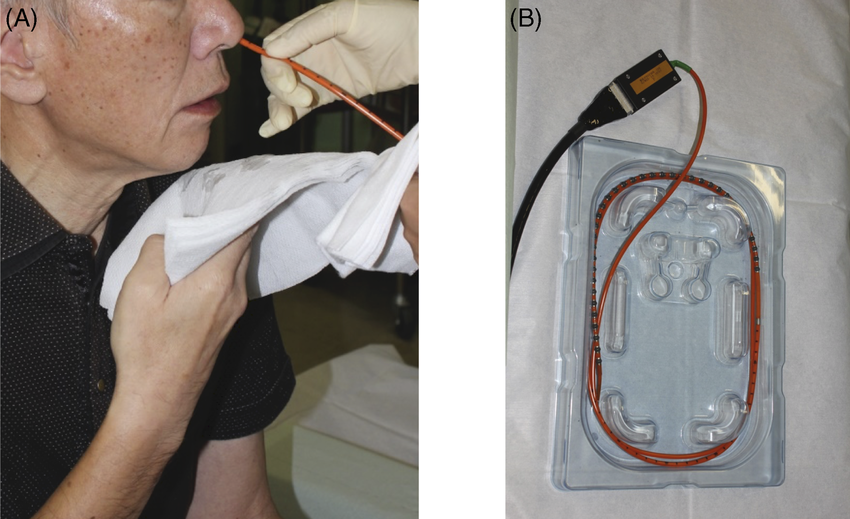
Insertion Of Catheter
Your doctor first lubricates the catheter, then inserts it through your nose or mouth and further guides it into the esophagus with the help of videofluoroscopy and positions it in the esophagus almost 3-5 centimeters above the lower esophageal sphincter.
Calibration
After inserting the catheter, your doctor will calibrate the manometry system and take a baseline reading to take it as a reference point.
Wet Swallows
They ask you to take five to ten milliliters of water and measure the esophageal pressure.
They repeat wet swallows after every ten minutes and take almost ten readings.
Dry Swallows
After wet swallows, they ask you to swallow without drinking water and take a reading. They repeat dry swallows for three to five minutes.
Pressure Measurements
Your doctor will measure the pressure of your lower esophageal sphincter and motility pattern while performing the dry and wet swallows.
Now, automated software will evaluate the data, and the doctor will receive information related to the moments and pressure in your esophagus and its sphincters, including Integrated relaxation pressure (IRP), contractile deceleration point (CDP), and the distal contractile integer (DCI).
Complications Of Esophageal Manometry
Esophageal manometry is generally a safe procedure having fewer complications, but following compilations of esophageal manometry may occur:
Esophageal Injury
During the insertion of the catheter inside the esophagus, an esophageal injury may occur. Tube insertion in patients having achalasia can perforate the esophagus even if an inexperienced person performs it.
Gagging Or Coughing
Tube insertion can activate your gag or cough reflex, cause vomiting, and hinder the procedure.
Infection
Infection may occur during esophageal manometry if the instruments are not sterilized or they do not follow aseptic protocol.
Complications Of Topical Anaesthesia
This process is performed under topical Anaesthesia, and the complications of topical anaesthesia, like skin reaction, allergy, abscess, nerve damage or systemic toxicity, may occur during the procedure.
Esophageal Spasm:
Esophageal problems like esophageal spasms can occur during esophageal manometry.
Aspiration Pneumonia:
The patient may aspirate the esophageal contents through the airway to the lungs, and aspiration pneumonia may occur.
Bleeding:
In esophageal manometry, there is a risk of bleeding from the mouth, nose, and throat. Moreover, If perforation of the esophagus occurs, there is a risk of bleeding from the esophagus.
Chest Pain & Heartburn:
Chest pain, discomfort or heartburn can occur during esophageal manometry.
What Safety Measures Should Be Adopted After Esophageal Manometry?
After esophageal manometry, your doctor ensures the following safety measures:
- Observation and monitoring of the patient for thirty minutes after the procedure
- Vitals monitoring that includes pulse, blood pressure, and oxygen saturation monitoring
- Analgesics for pain relief
- Monitoring for bleeding from your nose or throat and any discharge
- Wound care and antibiotics for infection control
- Swallow carefully and avoid heavy meals
- Proper follow-up for interpretation of results and further management of diagnosed pathology
How Do Doctors Interpret The Results Of Esophageal Manometry?
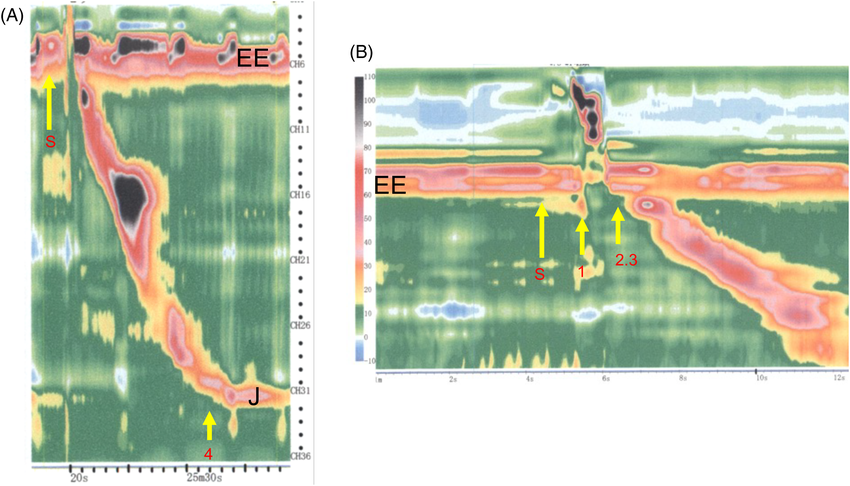
Doctors classify the results of esophageal manometry results in groups according to the Chicago classification.
Group l Chicago Classification:
Group one Chicago classification is incomplete lower esophageal sphincter relaxation that represents achalasia and obstruction of the esophagogastric junction.
Achalasia
Achalasia means failure of peristalsis and absence of relaxation of the lower esophageal sphincter. Moreover, there is difficulty in swallowing, and there is regurgitation of food. In manometry results, a rise in integrated relaxation pressure (IRP) represents achalasia. Integrated relaxation pressure represents the esophagogastric junction relaxation, and its normal value is less than 15 millimeters of mercury. The reason behind the increase in integrated relaxation pressure is failed peristalsis and failure of relaxation of the lower esophageal sphincter, which results in the accumulation of food and a rise in the integrated relaxation pressure.
Obstruction Of Esophagogastric Junction
If you have high integrated relaxation pressure, failure of relaxation of your lower esophageal sphincter along with weak peristalsis, and you don’t have achalasia, then you have obstruction of your esophagogastric junction.
Group II Chicago Classification:
The second group in the Chicago classification represents major problems in peristalsis, such as Jackhammer esophagus, esophageal spasm, and absent peristalsis of the esophagus.
A distal contractility integer (DCI) less than 450 millimeters of mercury indicates weak peristalsis, while a value greater than eight thousand millimeters of mercury indicates hypercontractility.
Esophageal Spasm
Your doctor diagnoses esophageal spasm if you have distal latency of less than 4.5 seconds.
Jackhammer Oesophagus
If your doctor measures the distal contractile integer of more than 8000 millimeters of mercury, it is a Hypercontractile or Jackhammer esophagus.
Absent Contractility
If you have absent contractility, your distal contractility integer will be less than a hundred millimeters of mercury. However, integrated relaxation pressure will be normal.
Group lII Chicago Classification:
Group three Chicago classification represents major peristalsis problems, including infective and fragmented peristalsis.
Ineffective Peristalsis
Ineffective peristalsis causes more than fifty percent of swallows to go infective. Moreover, the distal contractility integer is also less than a hundred millimeters of mercury.
Fragmented Peristalsis
In fragmented peristalsis, there is a gap between peristaltic waves, and your doctor observes ineffective motility.
Nutcracker Oesophagus
In the nutcracker esophagus, the distal contractility integer lies between eight thousand to fifteen hundred millimeters of Mercury.
Group IV Chicago Classification:
Group four of the Chicago classification represents the normal esophagus. In this category, the integrated relaxation pressure is normal (15 millimeters of mercury); moreover, distal latency is also normal ( between 450 and 8000 millimeters of mercury). Your doctor usually observes such manometry findings in patients with Gastroesophageal reflux disease when they go for a workup before surgery. More than fifty percent of their effective swallows are normal.
What Is Esophageal Manometry With Impedance?
Esophageal manometry with impedance is a combined test for assessing esophageal pressures, contractility, and motor functions. It includes esophageal manometry for measuring pressure and muscle contractions in the esophagus and the impedance for measuring the flow of liquids, gases, and solids through the esophagus. It helps in diagnosing conditions like achalasia, spasms, dysphagia, gastroesophageal reflux disease, and other motility disorders. In this procedure, your doctor inserts a probe with a sensor into the esophagus, and the sensor detects the flow of liquids along with the esophageal pressure and motility. The measurements are plotted on a graph that helps in assessing the function of the esophagus.
What Is High-Resolution Manometry?
Nowadays, doctors prefer High-Resolution Manometry (HRM) over conventional Manometry as it provides more details. It is the gold standard for the investigation of many diseases. In this process, your doctor inserts a catheter with probes in your esophagus that transmits intraluminal data. Then, the software converts this data to dynamic esophageal pressure topography plots. After placing the probe, the doctor takes a baseline measurement, then performs ten wet swallows and compares the results in the end.
Esophageal Manometry Vs. Barium Swallow
| Esophageal Manometry | Barium Swallow | |
| Definition | Esophageal manometry is the measurement of pressure and muscle contractions in the esophagus to diagnose disorders of esophagus like gastroesophageal reflux disease, achalasia and dysphagia. | Barium Swallow is used to access the anatomy, structure, and function of your esophagus, upper esophageal sphincter, and stomach. |
| Procedure | In esophageal manometry, your doctor passes a probe with sensors from your nose to the esophagus, which senses its movement and pressure. | In a Barium swallow, your doctor gives you a barium mixture to drink. The mixture coats the mucosa of the esophagus, and your doctor takes X-rays to visualize the anatomy of the esophagus and check its function. |
| Purpose | Manometry focuses on the muscle contractions and pressure in the esophagus.
It is more sensitive to motility disorders. |
Barium swallow focuses on the anatomy and structural integrity of the esophagus.
It is more sensitive for the detection of structural appearance. |
Difference Between Endoscopy & Esophageal Manometry
Endoscopy and Esophageal Manometry are two different procedures for testing the function of the gastrointestinal tract. Endoscopy is a technique to visualize the inside of your gastrointestinal tract, while esophageal manometry focuses on evaluating the pressure and movements of your esophageal muscles. In endoscopy, your doctor uses a soft, flexible tube along with a camera that helps visualize the gastrointestinal tract mucosal lining and detect lesions in the gastrointestinal tract. Doctors also perform endoscopy to take samples for biopsy. Endoscopy is helpful for diagnosis of Gastroesophageal reflux disease, cancer, ulcers, and inflammation.
Conclusion
Esophageal manometry is a procedure to diagnose motility disorders of your esophagus. It measures the pressure and contractility patterns of your esophagus with the help of a probe. Its indications include dysphagia, gastroesophageal reflux disease, chest pain, choking, and difficulty in swallowing food. The results of these tests help in the diagnosis of various esophageal disorders like achalasia, esophageal spasm, jackhammer esophagus, and nutcracker esophagus.





