Impacted wisdom teeth are third molars that do not have enough space to emerge or develop properly in the mouth. The surgical procedure for the removal of impacted wisdom teeth, especially in the lower jaw, is the most common intervention in the dental clinic.1McArdle LW, Renton T. The effects of NICE guidelines on the management of third molar teeth. Br Dent J. 2012;213:E8. doi: 10.1038/sj.bdj.2012.780 Patients between the ages of 18-25 are more likely to present with problems associated with impacted wisdom teeth, however, older patients may also experience symptoms and require treatment before the age of 70.2Renton T, Wilson NH. Problems with erupting wisdom teeth: signs, symptoms, and management. Br J Gen Pract. 2016 Aug;66(649):e606-8. doi: 10.3399/bjgp16X686509. PMID: 27481985; PMCID: PMC4979926.
Human dentition consists of various types of teeth, of which molars are responsible for chewing food. Our ancestors had more than four molars in each jaw, which gradually decreased due to the decrease in changing dietary habits. Over time, the agricultural and industrial revolutions contributed to changes in jaw size, resulting in smaller jaws that could no longer accommodate additional molars. In most cases, the lack of space leads to the third molar aka the wisdom teeth remaining unerupted and entrapped within their eruption site.3Richardson M.E. The etiology and prediction of mandibular third molar impaction. Angle Orthod. 1977;47:165–172. doi: 10.1043/0003-3219(1977)047<0165:TEAPOM>2.0.CO2.
Does everyone have Wisdom Teeth Impaction?
The prevalence of impacted wisdom teeth is affected by race, region, and local factors such as oral function. It is generally agreed that more than half of the global population exhibits one or more wisdom tooth abnormalities, which include bone-impacted wisdom teeth. When present, wisdom teeth in the lower jaw are at a greater risk of one of the many kinds of impaction than the upper jaw.4Pinto, A. C., Francisco, H., Marques, D., Martins, J. N. R., & Caramês, J. (2024). Worldwide Prevalence and Demographic Predictors of Impacted Third Molars—Systematic Review with Meta-Analysis. Journal of Clinical Medicine, 13(24), 7533. https://doi.org/10.3390/jcm13247533
There is also an increasing incidence of wisdom tooth agenesis, which implies a total lack of third molar formation. Hence, not everyone will have wisdom teeth.5Jung, H., & Cho, H. (2013). Prevalence of missing and impacted third molars in adults aged 25 years and above. Imaging Science in Dentistry, 43(4), 219. https://doi.org/10.5624/isd.2013.43.4.219
Impacted vs Erupted Wisdom Teeth
Before moving on to impactions, it is important to understand the differences between impacted and erupted third molars. Erupted third molars are those that have the proper space and alignment for emerging into their functional spot. Such wisdom teeth are completely visible and are similar in form and alignment to their neighboring molars. In contrast, impacted wisdom teeth are the ones that may or may not have erupted into the oral cavity but end up being misaligned due to a lack of proper space between the second molar and the jaw bone. Such teeth do not attain a functional position and are a cause of patient discomfort. You can see a partial bony or soft tissue impaction when only a part of the tooth is visible in the mouth.
Types of Wisdom Teeth Impaction
Classification based on the type of Tissue:
Soft Tissue Impaction:
When the wisdom tooth has erupted through the bone but has not emerged from the overlying soft tissue, i.e. the gum, it is referred to as a soft tissue impaction. The management of such cases is very straightforward and only requires relief from the overlying gum to allow eruption.
Bony Impaction:
When the wisdom teeth fail to erupt through the part of the jaw bone where it is formed, they are called Bone-impacted wisdom teeth. This type of impaction can further be classified as:
- Partially bony impacted wisdom teeth: In this scenario, the third molar has only partially erupted from its bony confines and is entrapped between the bone and the overlying soft tissue. Such cases are often symptomatic and may cause a lot of discomfort to the patient.
- Completely bone-impacted wisdom teeth: As the term implies, the third molar is housed in an abnormal position within the jaw bone and may present as a pathology later in life. Complete bony impaction can also remain asymptomatic.
Classification based on Alignment:
Mesial Impaction:
When the impacted wisdom tooth is directed towards the second molar, it is said to be a mesial impaction. This is the most common type of impacted wisdom teeth.
Distal Impaction:
If the impacted wisdom tooth is such that its crown is directed towards the back of the mouth, it is classified as distal impaction.
Vertical Impaction:
When the tooth itself is in the proper direction, with the root and crown in line with the long axis of the adjacent molar, it is referred to as a vertical impaction. Many soft tissue impactions are vertical.
Horizontal Impaction:
Horizontally impacted wisdom teeth are the ones with the crown almost at a right angle to the long axis of the neighboring molar and the root facing the end of the mouth.
Tell-tale signs of Impacted Wisdom Teeth
The symptoms of the impacted wisdom teeth range from mild discomfort to clear swelling of the face, depending on whether or not an infectious process has begun. Following are some of the most common manifestations of the condition:
- Constant pain and tenderness at the end of the mouth
- Inability to open the jaw to the fullest
- Routine cheek bites
- Crowding of teeth in the affected jaw
- Referred pain to the ear
- Swelling over the cheek and area at the angle of the jaw
- Toothache accompanied by fevers and chills
- Bad mouth odor
- Spitting out of pus often
- Strange taste in the mouth
Diagnosis of Impacted Wisdom Teeth
Clinical Examination
An important thing to bear in mind is the fact that many impacted wisdom teeth may present asymptomatically. This doesn’t imply that they can be retained as they are potentially frequent sites of pathologies later in life. Symptomatic cases will present with the classical features of inflammation and infection, i.e. pain, tenderness, pus discharge, oral and facial swellings, and even fever. Probing to exclude periodontal disease, vital pulp therapies such as cold and hot tests, percussion tests, and other routine dental tests are carried out on the adjacent teeth to pinpoint the exact tooth. Diagnosing bone-impacted wisdom teeth based on clinical examination is not appropriate, however, partially bony-impacted wisdom teeth can be assessed clinically. The confirmation of a diagnosis will always require imaging together with the assessment of the alignment of the impacted teeth and their relation to neighboring structures.
Radiography
Panoramic radiographs are preferred to other 2D imaging as they give a clearer view of the relationship between the impacted teeth and the neighboring structures such as the nerve canal. Its biggest advantage is the ability to reveal all impacted teeth in a single image, significantly lowering the radiation dose otherwise administered to the patient through multiple periapical radiographs. It is considered the diagnostic modality of choice for impacted wisdom teeth.6Flygare L, Ohman A. Preoperative imaging procedures for lower wisdom teeth removal. Clin Oral Investig. 2008 Dec;12(4):291-302. doi: 10.1007/s00784-008-0200-1. Epub 2008 Apr 30. PMID: 18446390.
CBCT
CBCT can be considered a type of dental CT, specially designed to provide a 3D view of bone-impacted wisdom teeth and their adjacent structures.CBCT provides greater anatomical detail and can be used throughout the procedure. The benefit of a lesser radiation dose makes it an ideal imaging technique.7Ghaeminia H, Meijer GJ, Soehardi A, Borstlap WA, Mulder J, Vlijmen OJ, Bergé SJ, Maal TJ. The use of cone beam CT for the removal of wisdom teeth changes the surgical approach compared with panoramic radiography: a pilot study. Int J Oral Maxillofac Surg. 2011 Aug;40(8):834-9. doi: 10.1016/j.ijom.2011.02.032. Epub 2011 Apr 19. PMID: 21507612.
Indications for Impacted Wisdom Teeth Removal
Swelling of the Surrounding Gum
For most patients, the first and foremost indication of a third molar impaction is the swelling of the soft tissue covering and the surrounding the impacted tooth. This may lead to the formation of a small gap between the gum and the second molar that may accumulate food and other debris over time. Without adequate cleaning and frequent dental check-ups, the gum may become swollen, can bleed during chewing, and cause intense pain. The term used for this condition is pericoronitis, which can result in swelling of the associated lymph nodes and fever in its most severe form.
Orthodontic Treatment
Usually, before starting orthodontic treatment, all impacted wisdom teeth are extracted regardless of their symptomatic status. This decreases the chances of treatment relapse and prevents problems of spacing or alignment of teeth in the future.
Involvement of Adjacent Teeth
One of the most common indications of treating impacted wisdom teeth symptoms is the adverse sequelae it causes in the neighboring erupted second molar. Bone-impacted wisdom teeth, especially those lying with the crown facing the midline, can put pressure on the roots of the second molar. This can damage the roots, leading to resorption, or lead to a pocket formation that can initiate the process of root caries. Since most of these undesirable changes take place within the confines of the soft tissue, they mostly go clinically unnoticed until symptoms start to arise. In the most severe cases, the vital therapy or extraction of the second molar may become a necessity together with impacted wisdom tooth removal.
Site of Potential Pathology
According to a study, almost 64% of impacted wisdom teeth, if left untreated, may lead to a pathology later in life. This pathology may either be related to the affected teeth or to their adjacent structures.8Dodson TB, Susarla SM. Impacted wisdom teeth. BMJ Clin Evid. 2014 Aug 29;2014:1302. PMID: 25170946; PMCID: PMC4148832. Studies also conclude that since not all impactions cause blatant symptoms, many asymptomatic and retained impacted teeth are more likely to be involved. Dentigerous cysts and ameloblastoma were the most common cysts and tumors, respectively, to be associated with retained impacted teeth.9Mortazavi, H., & Baharvand, M. (2016). Jaw lesions associated with impacted tooth: A radiographic diagnostic guide. Imaging Science in Dentistry, 46(3), 147. https://doi.org/10.5624/isd.2016.46.3.147
Current Strategies to Treat Impacted Wisdom Teeth
Oral surgery is the most common therapy employed to relieve patients from impacted wisdom teeth symptoms. However, impacted wisdom teeth removal may also be undertaken as a preventive measure to keep problems associated with the condition at bay. As the risk of post-operative complications increases with age, many dentists believe that wisdom teeth should be removed timely. The most favorable time of extraction is during the teenage and adolescent years.
Periodic Follow-up
Asymptomatic bone-impacted wisdom teeth can be retained without treatment with regular clinical and radiographic follow-ups to detect possible pathoses. In cases where a patient’s advanced age and comorbidities preclude oral surgery, this may be the safest approach.
Operculectomy
Patients with partially bony impacted wisdom teeth that have adequate space for eruption can benefit from the removal of the soft tissue barrier i.e. operculectomy. This minimally invasive procedure can also help with inflammation arising from continuous food impaction between the gum overlying the partially erupted molar and its coronal portion.
Guided eruption
This procedure is rarely performed and it is more suitable for lower impacted wisdom teeth in which the molars are orthodontically brought into occlusion. Guided eruption is more commonly employed in impactions involving canines and premolars.
Coronectomy
For impacted wisdom teeth removal that may endanger the adjacent nerve, sinuses, or teeth, coronectomy may be an appropriate therapy. In this procedure, a pre-operative radiograph rules out periapical pathologies and ascertains the relationship of the impacted wisdom tooth. The procedure involves sectioning the tooth at the crown level, leaving the root intact. Typically, the sectioning is performed approximately 3-4 mm below the surrounding bone level. Coronectomy is especially useful for patients with dental anxiety or underlying medical conditions that make full extraction riskier. However, it is not recommended for horizontally impacted wisdom teeth or those with existing periapical infections. Strict follow-up is required to monitor the status of the retained roots and ensure no complications arise over time.
Extraction
After a thorough pre-operative examination, the oral surgeon might deem extraction of the impacted wisdom teeth, irrespective of the symptomatic treatment, to be the only therapeutic option available. Extraction is the gold standard for impacted wisdom teeth infection treatment.
Assessing Difficulty of Extraction
An assessment of the difficulty of extraction minimizes undesirable post-operative complications. The criteria include:
Factors related to the Impacted Wisdom Teeth:
When the impaction is completely horizontal, such that the crown of the wisdom tooth is at a right angle to the roots of the adjacent second molar, a risk is present of damaging the latter during the surgery. There are multiple standards to guide pre-surgical planning. A preliminary assessment of the inclination and angulation of the bone-impacted wisdom teeth can reduce the incidence and severity of postoperative complications.
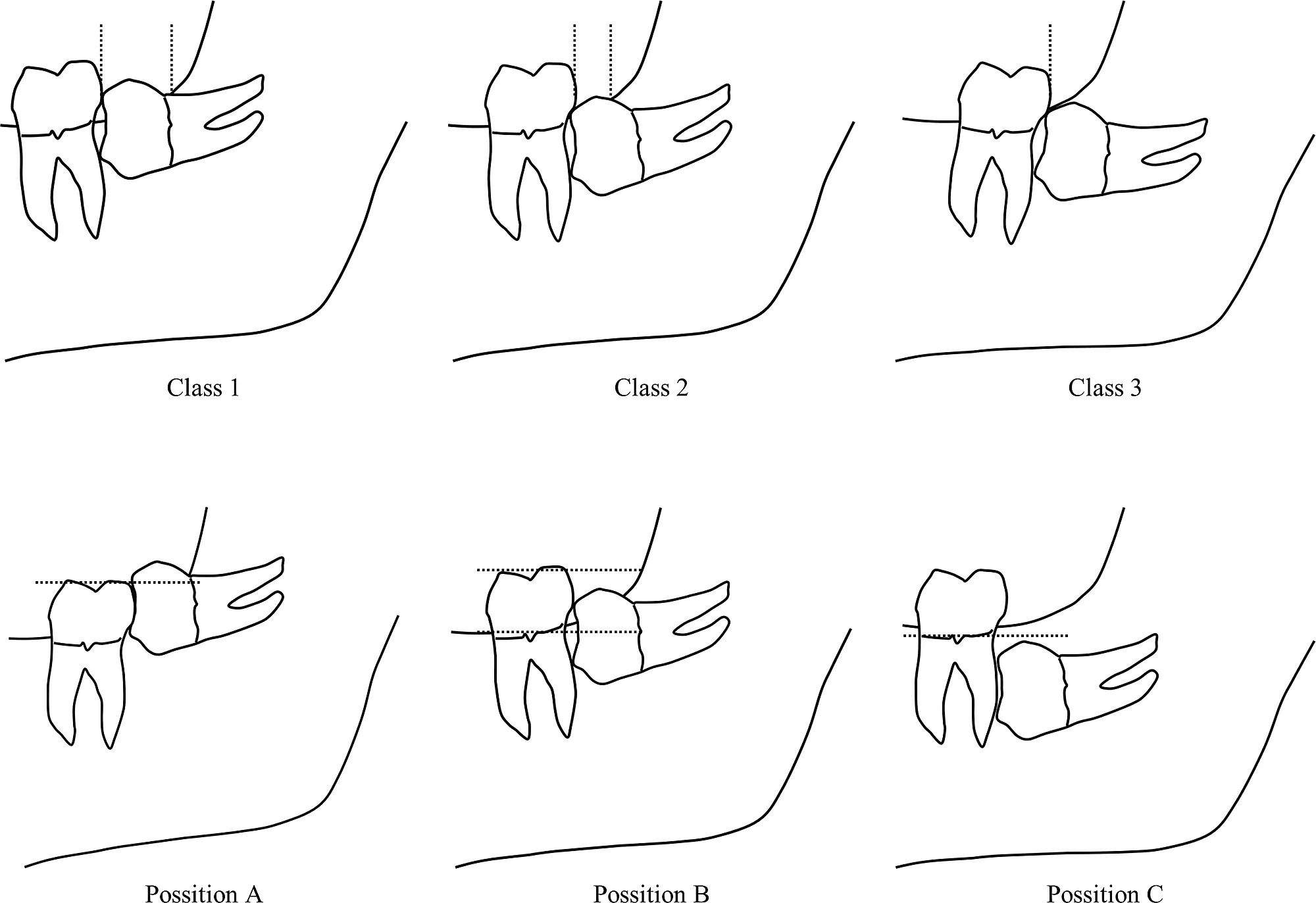
Pre-surgical classification systems, such as Pell and Gregory, help categorize impactions based on the tooth’s depth and relation to the ramus of the mandible. However, some studies suggest that these classifications may not always reliably predict the difficulty of extraction.10García García, A., Gude Sampedro, F., Gandara Rey, J., Gandara Vila, P., & Somoza Martin, M. (2000). Pell–Gregory classification is unreliable as a predictor of difficulty in extracting impacted lower third molars. *British Journal of Oral and Maxillofacial Surgery, 38*(6), 585–587. https://doi.org/10.1054/bjom.2000.0535 The anatomy of the impacted wisdom teeth is another important determinant. Teeth with divergent roots and closeness to the nerve canal require meticulous surgical technique, preferably by an experienced oral and maxillofacial surgeon.
Patient-Related Factors:
Advanced age, obesity, and an immunocompromised state increase the chances of post-operative complications and delay healing. Odontophobia or dental anxiety can also adversely affect the outcome of the surgery. Patients who suffer from problems related to their jaw can have limited mouth opening that restricts surgical access. After the difficulty assessment, the doctor will choose between local and general anesthesia. The dentist will give an incision on the overlying soft tissue to approach the tooth in its bony confines. A small ditch will be created around the tooth. This will make space for instrument insertion and tooth sectioning. Depending on the skill of the surgeon, tooth anatomy, and the patient’s ease, the tooth may either be extracted in total or maybe sectioned.
Potential Side Effects of Wisdom Teeth Removal
Dry Socket:
The medical term for this condition is alveolar osteitis. It is the most common postoperative complication of impacted wisdom teeth removal. The main symptoms of this condition include pain at or near the site of extraction, abnormal taste in the mouth, and bad breath.11Tarakji, B., Saleh, L. A., Umair, A., Azzeghaiby, S. N., & Hanouneh, S. (2015). Systemic Review of Dry Socket: Aetiology, Treatment, and Prevention. Journal of Clinical and Diagnostic Research: JCDR, 9(4), ZE10. https://doi.org/10.7860/JCDR/2015/12422.5840
Sensation Disorders:
This is an infrequent complication of impacted wisdom tooth surgery. It is a result of poor pre-operative planning or erroneous imaging.
Post-Operative Bleeding:
Many patients may experience greater than normal bleeding, especially in the absence of meticulous post-surgery care. Sucking strongly on straws immediately after the procedure, underlying bleeding disorders, and continuous physical irritation to the site of extraction are the most common culprits.
Facial Swelling:
Swelling of the jaw or edema is common after an impacted wisdom tooth extraction. Generally, the longer the duration of the surgery, the greater the post-operative swelling.12de Santana-Santos T, de Souza-Santos aA, Martins-Filho PR, da Silva LC, de Oliveira E Silva ED, Gomes AC. Prediction of postoperative facial swelling, pain, and trismus following third molar surgery based on preoperative variables. Med Oral Patol Oral Cir Bucal. 2013 Jan 1;18(1):e65-70. doi: 10.4317/medoral.18039. PMID: 23229245; PMCID: PMC3548647.
Conclusion
Impacted wisdom teeth are a direct result of evolution and changes in the way humans lead their lives. Smaller jaws mean that they may not always be able to accommodate an extra molar. In case of infection, removal is inevitable. Prophylactic removal should be undertaken when the risks of retention outweigh the benefits. The medical profile, dental hygiene, and skill of the surgeon together determine the outcomes. If you are experiencing pain and discomfort, don’t delay seeing a dentist. It may be an impacted wisdom tooth requiring immediate removal.
Refrences
- 1McArdle LW, Renton T. The effects of NICE guidelines on the management of third molar teeth. Br Dent J. 2012;213:E8. doi: 10.1038/sj.bdj.2012.780
- 2Renton T, Wilson NH. Problems with erupting wisdom teeth: signs, symptoms, and management. Br J Gen Pract. 2016 Aug;66(649):e606-8. doi: 10.3399/bjgp16X686509. PMID: 27481985; PMCID: PMC4979926.
- 3Richardson M.E. The etiology and prediction of mandibular third molar impaction. Angle Orthod. 1977;47:165–172. doi: 10.1043/0003-3219(1977)047<0165:TEAPOM>2.0.CO2.
- 4Pinto, A. C., Francisco, H., Marques, D., Martins, J. N. R., & Caramês, J. (2024). Worldwide Prevalence and Demographic Predictors of Impacted Third Molars—Systematic Review with Meta-Analysis. Journal of Clinical Medicine, 13(24), 7533. https://doi.org/10.3390/jcm13247533
- 5Jung, H., & Cho, H. (2013). Prevalence of missing and impacted third molars in adults aged 25 years and above. Imaging Science in Dentistry, 43(4), 219. https://doi.org/10.5624/isd.2013.43.4.219
- 6Flygare L, Ohman A. Preoperative imaging procedures for lower wisdom teeth removal. Clin Oral Investig. 2008 Dec;12(4):291-302. doi: 10.1007/s00784-008-0200-1. Epub 2008 Apr 30. PMID: 18446390.
- 7Ghaeminia H, Meijer GJ, Soehardi A, Borstlap WA, Mulder J, Vlijmen OJ, Bergé SJ, Maal TJ. The use of cone beam CT for the removal of wisdom teeth changes the surgical approach compared with panoramic radiography: a pilot study. Int J Oral Maxillofac Surg. 2011 Aug;40(8):834-9. doi: 10.1016/j.ijom.2011.02.032. Epub 2011 Apr 19. PMID: 21507612.
- 8Dodson TB, Susarla SM. Impacted wisdom teeth. BMJ Clin Evid. 2014 Aug 29;2014:1302. PMID: 25170946; PMCID: PMC4148832.
- 9Mortazavi, H., & Baharvand, M. (2016). Jaw lesions associated with impacted tooth: A radiographic diagnostic guide. Imaging Science in Dentistry, 46(3), 147. https://doi.org/10.5624/isd.2016.46.3.147
- 10García García, A., Gude Sampedro, F., Gandara Rey, J., Gandara Vila, P., & Somoza Martin, M. (2000). Pell–Gregory classification is unreliable as a predictor of difficulty in extracting impacted lower third molars. *British Journal of Oral and Maxillofacial Surgery, 38*(6), 585–587. https://doi.org/10.1054/bjom.2000.0535
- 11Tarakji, B., Saleh, L. A., Umair, A., Azzeghaiby, S. N., & Hanouneh, S. (2015). Systemic Review of Dry Socket: Aetiology, Treatment, and Prevention. Journal of Clinical and Diagnostic Research: JCDR, 9(4), ZE10. https://doi.org/10.7860/JCDR/2015/12422.5840
- 12de Santana-Santos T, de Souza-Santos aA, Martins-Filho PR, da Silva LC, de Oliveira E Silva ED, Gomes AC. Prediction of postoperative facial swelling, pain, and trismus following third molar surgery based on preoperative variables. Med Oral Patol Oral Cir Bucal. 2013 Jan 1;18(1):e65-70. doi: 10.4317/medoral.18039. PMID: 23229245; PMCID: PMC3548647.





