Traumatic Subarachnoid Hemorrhage (tSAH) is defined as the presence of bleeding below the subarachnoid space followed by trauma. Your brain consists of 3 layers of meninges that protect your brain and spinal cord. These are dura Mater (outermost layer), arachnoid mater (middle layer), and pia mater (innermost layer). The subarachnoid hemorrhage causes bleeding below the arachnoid layer of the brain.
 Subarachnoid hemorrhage is usually not age or gender specific, but it occurs most commonly in older people (40-60 years).
Subarachnoid hemorrhage is usually not age or gender specific, but it occurs most commonly in older people (40-60 years).
In traumatic brain injury, traumatic subarachnoid hemorrhage shows a poor prognosis and progressive neurological deterioration with a higher mortality rate. According to research studies, approximately 69 million people present with a traumatic brain injury each year, and subarachnoid hemorrhage is the most commonly caused by traumatic brain injury. 1Griswold, D., Fernández, L. L., & Rubiano, A. M. (2022). Traumatic Subarachnoid Hemorrhage: A Scoping Review. Journal of Neurotrauma, 39(1-2), 35–48. https://doi.org/10.1089/neu.2021.0007
Symptoms of Traumatic Subarachnoid Hemorrhage
There are multiple symptoms of traumatic subarachnoid hemorrhage. However, the most common symptoms of tSAH include:
- Unconsciousness
- Thunderclap headache (the worst headache of your life)
- Diplopia (double vision)
- Third nerve palsy (drooping of the eyelid)
- Nausea and vomiting
- Speaking difficulty
- Confusion
- Photophobia (light sensitive)
- Sensory or motor deficits
- Dilated pupils
- Signs of meningitis (neck rigidity)
- Seizures or fits
Causes of Subarachnoid Hemorrhage
Besides traumatic brain injury, subarachnoid hemorrhage is caused by the following:
- Ruptured aneurysm
- Alcohol abuse
- Arteriovenous malformation (AVM)
- Bleeding diathesis
- Hypertension
- Drugs
Risk Factors of Subarachnoid Hemorrhage
Subarachnoid hemorrhage is associated with many risk factors. A few risk factors of subarachnoid hemorrhage include the following:
- Aging
- History of hypertension
- Smoking
- Female Gender
- Genetic disorder
- Alcohol or cocaine abuse
- Marfan syndrome
- Ehler-danlos syndrome
- Neurofibromatosis type 1
Diagnosis of Traumatic Subarachnoid Hemorrhage
Your doctor will diagnose subarachnoid hemorrhage by taking a detailed history, performing a thorough neurological examination, and prescribing laboratory and radiological investigation.
History:
A detailed history supports the diagnosis of traumatic subarachnoid hemorrhage. Your doctor will ask the following question:
- History of trauma?
- Severe headache?
- Vomiting?
- Any comorbidity?
- History of hypertension?
- History of diabetes?
Neurological Examination:
After taking a detailed history, your doctor will perform a neurological examination to check motor or sensory loss. Neurological examination may be normal in a few patients, and others may have a focal deficit with impaired consciousness levels. Conscious level is checked by using the Glasgow Coma Scale (GCS).
- What is GCS?
GCS is performed to check your consciousness level. It has 15 numbers on the scale. It is performed as follows:
| Score |
Eye-opening | Verbal response | Motor response |
| 1 | None | None | None |
| 2 | Eye-opening in response to any stimulus | Incomprehensible sounds | Extension |
| 3 | Eye-opening in response to sound | Incomprehensible sentences or words | Abnormal flexion |
| 4 | Spontaneous response | Confused | Normal flexion |
| 5 | Well oriented | Localizes pain | |
| 6 | Obeys all commands |
Mild: 13-15 Moderate: 9-12 Severe: 3-8
- What is the grading of subarachnoid hemorrhage?
The World Federation of Neurosurgical Societies (WFNS) graded the subarachnoid hemorrhage. However, this grading is done after the resuscitation of the patient rather than at the time of presentation in the emergency department. There are five grades of subarachnoid hemorrhage:
| Grade | GCS | Focal deficits |
| 1 | 15 | No focal deficit |
| 2 | 13-14 | No focal deficit |
| 3 | 13-14 | Focal deficits are present |
| 4 | 7-12 | It may or may not be present |
| 5 | 3-9 | It may or may not be present |
Focal deficit means dysphasia (inability to speak resulting from brain damage or brain injury) or limb weakness.
Laboratory Investigations:
Following the initial phase of management, the progression of patient treatment necessitates a series of essential laboratory investigations. These investigations play a pivotal role in not only advancing the patient’s therapeutic journey but also in effectively eliminating alternative causes of subarachnoid hemorrhage, thereby ensuring accurate diagnosis and tailored treatment strategies.
These are the following:
Complete Blood Count (CBC)
A comprehensive evaluation of the patient’s blood composition, including red blood cells, white blood cells, and platelets, is undertaken through a complete blood count. This assessment aids in identifying any potential abnormalities that could contribute to the subarachnoid hemorrhage or impact the treatment trajectory.
Random Blood Sugar (RBS)
Measurement of the random blood sugar level assists in discerning the patient’s glycemic status. Fluctuations in blood sugar levels can influence the overall health condition and potentially impact the course of subarachnoid hemorrhage treatment.
Platelets Count
The count of platelets, vital for blood clotting, is determined. Deviations from the normal platelet count could indicate underlying conditions that may have triggered the subarachnoid hemorrhage.
Electrolytes Level
Assessment of electrolyte levels, encompassing sodium, potassium, and chloride, provides insights into the patient’s metabolic balance. Imbalances in electrolytes could potentially exacerbate the effects of subarachnoid hemorrhage and warrant careful management.
Lumbar Puncture
Lumbar puncture is highly sensitive for the diagnosis of subarachnoid hemorrhage in the first 12 hours of traumatic brain injury. It can diagnose subarachnoid hemorrhage even if the CT scan is normal. Lumbar puncture indicates higher opening pressure and the presence of red blood cells in cerebrospinal fluid. Moreover, Xanthochromia (presence of degradation products of hemoglobin in CSF) demonstrates that blood has been in the cerebrospinal fluid for 2 hours. It can last for at least two weeks.
Additionally, Spectrophotometry detects breakdown products of blood, including oxyhemoglobin, methemoglobin, and bilirubin. Comparatively, this test has a higher sensitivity than xanthochromia, but it is not preferred.
Rationale For Laboratory Investigations
Besides lumbar puncture for traumatic subarachnoid hemorrhage, the following laboratory investigations help determine the severity and complications associated with subarachnoid hemorrhage.
2Subarachnoid hemorrhage laboratory findings – wikidoc. (2022). Wikidoc.org. https://www.wikidoc.org/index.php/Subarachnoid_hemorrhage_laboratory_findings
| Blood test | Result | Rationale |
| Complete blood count (CBC) and platelet count | Increased number of leukocytes (leukocytosis)
Polycythemia (increased RBCs in the blood) Thrombocytopenia |
Look for infections
Hematocrit and platelet count help determine hemorrhagic complications and associated risk factors. |
| Serum electrolyte levels | Increased or decreased levels of serum calcium, sodium, or potassium | Serum electrolyte levels are the baseline for the detection of hemorrhagic complications |
| Serum PT\APTT\INR | Increased levels of PT \ APTT \ INR | Increased levels indicate coagulopathy |
| Renal function tests | Increased BUN and creatinine levels | Renal function tests are the baseline for the detection of hemorrhagic complications. |
| Cardiac enzymes | Higher levels of Trop I, Trop T, and CKMB | Higher levels of cardiac enzymes suggest myocardial ischemia ongoing along with subarachnoid hemorrhage. |
Radiological Investigation:
Radiological investigations remain the mainstay of diagnosis. Moreover, these interventions are always required in patients with trauma. In patients with head trauma, the following investigations are required:3Kim, J., & Seung Jin Lee. (2020). Traumatic Subarachnoid Hemorrhage Resulting from Posterior Communicating Artery Rupture. International Medical Case Reports Journal, Volume 13, 237–241. https://doi.org/10.2147/imcrj.s254160
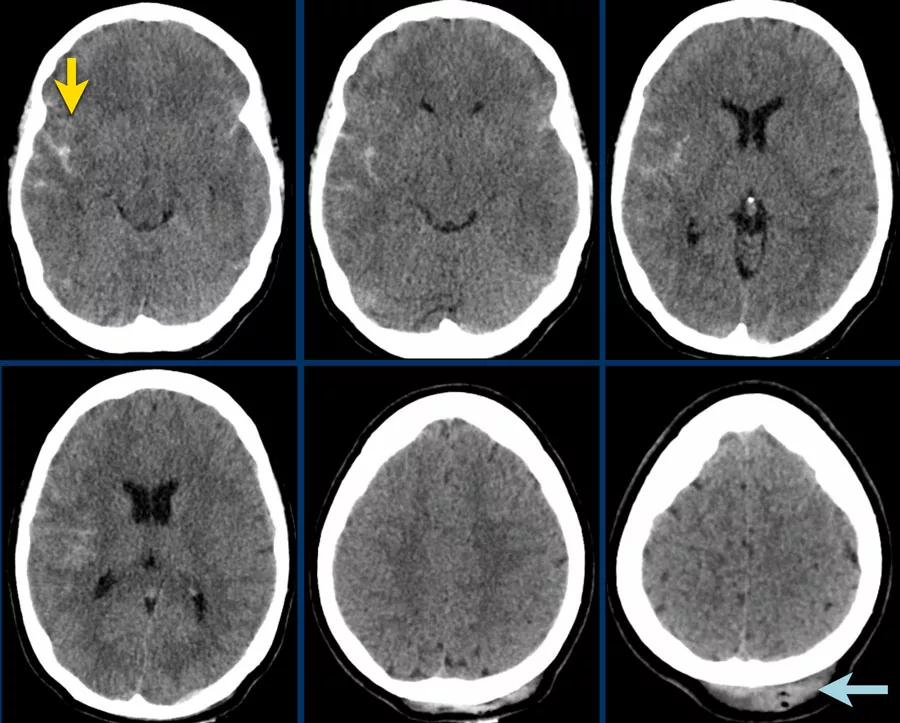
CT Brain
CT brain is the investigation of choice in patients with traumatic brain injury when performed within 12 hours of injury. It confirms bleeding into the brain in most of the cases. The sensitivity of this radiological scan lessens after one week of the traumatic brain injury. In these patients, doctors usually prescribe lumbar puncture. However, the sensitivity of a CT scan depends on the amount of blood and the time period. Usually, a small amount of blood fills the sulci, and contusions are visible.
Angiography
While MRI and CT angiography offer visual insights into the site of bleeding, it’s noteworthy that digital subtraction angiography stands as the gold standard investigation in this context. Importantly, digital subtraction angiography provides comprehensive access to both the vertebral and carotid arteries.
MRI
MRI, on the other hand, is recommended primarily in scenarios involving subacute brain bleeding. This imaging technique serves as a valuable tool under such circumstances.
Other Radiological Investigations:
Other radiological investigations required to rule out the other injuries are:
X-ray Chest
X-ray chest is performed to rule out any chest abnormality and trauma to the chest in a roadside accident.
Xray Pelvis
An X-ray pelvis is required to see the pelvis abnormality, hip joint fracture, or any other concealed hemorrhage.
FAST Scan
The FAST scan is compulsory in traumatic patients to rule out any abdominal viscera injury and bleeding.
Treatment of Traumatic Subarachnoid Hemorrhage
Traumatic subarachnoid hemorrhage poses a life-threatening emergency situation. However, following emergency management, the next step involves admitting the patient to the intensive care unit for the treatment of traumatic subarachnoid hemorrhage. Whenever there is a patient with traumatic subarachnoid hemorrhage, your doctor will follow these measures: 4Tibor Becske, MD. (2023, June 30). Subarachnoid Hemorrhage Treatment & Management: Approach Considerations, Initial Management, Rebleeding, and Clipping/Coiling Aneurysms. Medscape.com; Medscape. https://emedicine.medscape.com/article/1164341-treatment#d10?form=fpf
ABCDE Protocol:
Medical professionals consistently adhere to this protocol in trauma cases. The ABCDE protocol encompasses the following steps:
- Airway: The first step in the management of trauma patients includes checking the patency of the airway. Ask the patient to tell his name. However, if there is any suspicion of airway obstruction, clear the airway first.
- Breathing: In this phase, check breathing by monitoring oxygen saturation and respiration. If oxygen saturation drops, give oxygen support to the patient.
- Circulation: This step ensures optimal blood circulation in the body. After passing the IV line, maintain fluid circulation to avoid hypovolemic shock.
- Disability: Check for the disability of the patient.
- Exposure: Complete exposure of the patient is compulsory to see any other injuries on different parts of your body.
After the ABCDE protocol and getting radiological reports, your doctor will start medical management with regular cardiac monitoring, pulse oximetry, and input-output records.
Medical Management:
Medical intervention includes bed rest with hourly monitoring (strict input-output monitoring and fluid replacement). Calcium channel blockers are the drug of choice for the treatment of subarachnoid hemorrhage. Hence, your doctor may give Oral nimodipine 60 mg (a calcium channel blocker) to lower the risk of vasospasm.
Your doctor may prescribe other medications like:
- Laxatives
- antihypertensive to control blood pressure
- Analgesics
- Antiemetics (to prevent vomiting)
- Compression stocking
- Gastric protection (PPI)
In case of raised Intracranial Pressure, Your doctor may prescribe the following medications:
- Mannitol
- Loop diuretics
- Steroids (like dexamethasone)
Surgical Management:
Surgical interventions play a crucial role in preventing the leakage of blood into the subarachnoid space. Additionally, statistics reveal that approximately 15-30 percent of patients afflicted with subarachnoid hemorrhage succumb to the condition prior to hospital admission, and a further 25% meet the same fate within the initial 24 hours, irrespective of medical intervention. The prognosis for subarachnoid hemorrhage (SAH) remains unfavorable, marked by elevated levels of morbidity and mortality. Therefore, a range of surgical strategies are employed to address this complex condition:
Clipping
Clipping is no longer used as a first-line treatment of traumatic subarachnoid hemorrhage. The principle of clipping is to clip the ruptured aneurysm to stop the extravasation of blood. The clip is applied to the neck of the aneurysm without harming the adjacent artery.
Endovascular Methods
It is the first-line treatment option for SAH. It includes endovascular coil and balloon embolization and endovascular flow diversion. However, Coil embolization has a better response than other endovascular methods. In coil embolization, your surgeon fills the aneurysm with a coil that reduces blood flow toward the aneurysm.
Other Surgical Treatments
Additionally, other surgical treatments include ligation of the affected artery by tapping the aneurysm to reduce blood flow toward the affected site.
What are the Complications of SAH?
Complications of SAH include neurological and systemic complications. These are the following:
- Neurological Complications:
Neurological complications include vasospasm-related ischemia, neurological deficits, and hydrocephalus. - Systemic Complications:
Systemic complications are electrolyte imbalance, pulmonary edema, cardiac infarct, hypertension, and arrhythmia.
Subarachnoid Hemorrhage vs. Subdural Hematoma?
As the word suggests, sub means below, so Subarachnoid hemorrhage refers to acute bleeding below the arachnoid layer. It results from the rupture of the aneurysm or traumatic brain injury. On the other hand, subdural hematoma is characterized by a collection of blood between the inner layer of the dura and the arachnoid mater. Additionally, Trauma is the most common cause of subdural hematoma. Both of these have different radiological and clinical findings as well.
Conclusion:
To conclude, subarachnoid hemorrhage occurs due to bleeding below the arachnoid layer. Most patients with subarachnoid hemorrhage present with unconsciousness, confusion, and coma. Subarachnoid hemorrhage is a medical emergency. Therefore, in case of traumatic brain injury, immediately bring the victim to the hospital for emergency treatment in the golden hour (first hour after trauma).
Refrences
- 1Griswold, D., Fernández, L. L., & Rubiano, A. M. (2022). Traumatic Subarachnoid Hemorrhage: A Scoping Review. Journal of Neurotrauma, 39(1-2), 35–48. https://doi.org/10.1089/neu.2021.0007
- 2Subarachnoid hemorrhage laboratory findings – wikidoc. (2022). Wikidoc.org. https://www.wikidoc.org/index.php/Subarachnoid_hemorrhage_laboratory_findings
- 3Kim, J., & Seung Jin Lee. (2020). Traumatic Subarachnoid Hemorrhage Resulting from Posterior Communicating Artery Rupture. International Medical Case Reports Journal, Volume 13, 237–241. https://doi.org/10.2147/imcrj.s254160
- 4Tibor Becske, MD. (2023, June 30). Subarachnoid Hemorrhage Treatment & Management: Approach Considerations, Initial Management, Rebleeding, and Clipping/Coiling Aneurysms. Medscape.com; Medscape. https://emedicine.medscape.com/article/1164341-treatment#d10?form=fpf

