Malocclusion is a dental condition characterized by misalignment or improper positioning of the teeth when the jaws are closed. Patients with maligned tooth relationships should consult an orthodontist who will help patients in achieving an ideal dental occlusion and a balanced facial profile.
Before the commencement of treatment, orthodontists seek to know the cause of malocclusion. Abnormal development of tooth and jaw bones is the major cause of dental malocclusion. However, malocclusion of teeth can also result from several para-functional habits like mouth breathing, thumb sucking, pacifier sucking, and bruxism.
Definition
Malocclusion is a dental anatomy that emerges from improper positioning of the maxilla and mandible or faulty relation of upper and lower teeth. If this condition is left untreated, it will cause multiple oral complications in the patients. In dentistry, normal occlusion takes place when the mesiobuccal cusp(a part of the tooth) of the upper first molar rests in the buccal groove(a depression-like portion of the tooth) of the lower first molar. However, there will be no anomaly in the size, position, and alignment of the rest of the teeth in the mouth. However, if their tooth relationship gets disturbed and teeth have abnormal size, shape, and position, it will come under the category of malocclusion 1Masucci, C., Oueiss, A., Maniere-Ezvan, A., Orthlieb, J. D., & Casazza, E. (2020). Qu’est-ce qu’une malocclusion ? [What is a malocclusion?]. L’ Orthodontie francaise, 91(1-2), 57–67. https://doi.org/10.1684/orthodfr.2020.11
Classification of Malocclusion
There are multiple classifications of malocclusion, but the most common classification used in dentistry was Angle’s classification, which was presented by Dr. Edward Hartley Angle, also known as the father of modern orthodontists2Gravely, J. F., & Johnson, D. B. (1974). Angle’s classification of malocclusion: an assessment of reliability. British journal of orthodontics, 1(3), 79–86. https://doi.org/10.1179/bjo.1.3.79. He took the mesiobuccal cusp(an important part of the anatomy of the tooth) of the maxillary(upper) first molar as a reference and presented three types of malocclusions. We also observe the bone position and incisor relation for better understanding.
Class I Malocclusion
It refers to the normal molar relationship and normal positioning of the jaw, but teeth may be spaced, crowded, rotated, have anomalous shape and size, and abnormal positioning of single or multiple teeth3DiBenedetto D. C. (2011). Defining malocclusion. Journal of the American Dental Association (1939), 142(4), 368–369. https://doi.org/10.14219/jada.archive.2011.0178\
Class II Malocclusion
In this type of malocclusion, the mesiobuccal cusp of the upper first molar rests mesial(towards the midline) to the buccal groove of the lower first molar. In a bony relationship, the maxilla lies ahead of the mandible. When considering incisors, it has two further divisions:
- Class II, Division 1
In division 1, the upper incisors are protruding, which results in a significant increase in the horizontal relationship between the upper and lower incisors. This condition happens when a patient has a V-shaped maxillary bone with a constricted canine region. - Class II, Division 2
In division 2, upper central incisors show palatal(towards the inner side of the mouth) inclination, which causes deep overbite. In this condition, the maxilla has a broader size with the usual U-shaped shape.

Class III Malocclusion
In this type, the mesiobuccal cusp of the upper first molar lies distal(away from the midline) to the buccal groove of the lower first molar. Considering the bony relation, the mandible rests ahead of the maxilla. While lower incisors maintain a protruding(outward) relation concerning upper incisors. These conditions happen due to developmental issues like excessive growth of the mandible or multiple environmental or genetic factors.
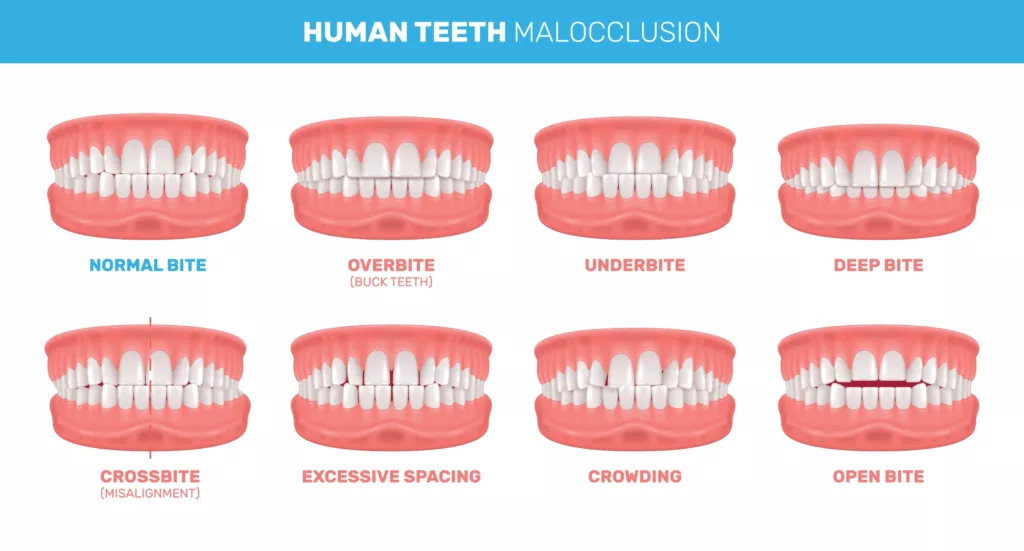
Types of Malocclusion
- When upper and lower teeth come in contact with each other, we observe an occlusal relationship like the area of lower teeth gets covered by upper teeth, and this coverage area tells us the extent of overbite. The normal range of this vertical overlap is 2-3mm. While it’s not unusual to have a bit of an overlap of the lower front teeth, an increased overbite can cause problems like your front teeth biting down onto your gums or your lower front teeth biting into the roof of your mouth. If the overlap range exceeds the normal value, it is termed a deep bite.
- If both upper and lower teeth fail to overlap vertically, this situation is termed an open bite.
- In some conditions, the upper front teeth are positioned backward with respect to the lower front teeth. This situation is termed as underbite or Anterior crossbite.
- The horizontal distance between the upper and lower central teeth describes the overjet, and its normal range is 2-3mm. An increase in overjet can lead to protrusion and incompetent lips. It can often interfere with chewing food and speaking properly.
- A crossbite occurs when your upper teeth bite inside your lower teeth. It can happen on one or both sides of your jaw and can affect your front or back teeth as well.
- Similarly, crowding occurs when there is less than normal space for teeth positioning.
- Spacing occurs when there is more than normal space for teeth positioning.
Impacts of Malocclusion
Malocclusion has various effects, and it impacts the day-to-day life of people experiencing malocclusion. For instance,
- Oral Hygiene: Difficulty in cleaning, leading to plaque buildup, cavities, and gum disease.
- Speech Problems: Articulation difficulties, potential lisp due to malocclusion.
- Self-Esteem: Aesthetic concerns impacting confidence and social interactions.
- TMJ Disorders: Strain on the temporomandibular joint, potential discomfort, and pain.
- Breathing & Sleep: Severe malocclusion contributing to obstructive sleep apnea.
- Nutrition: Avoidance of certain foods impacts nutritional intake.
- Chewing & Digestion: Inefficient chewing affects proper food breakdown and digestion.
Symptoms of Malocclusion
The main features of different classes of malocclusion are explained ahead.
Class I Malocclusion
- Patients have normal facial height and a balanced facial aesthetic.
- Regarding dental features, there is a tendency for crowding due to large size teeth or small arch space.
- Spacing can occur due to smaller-sized teeth or greater arch space.
- Abnormal occlusal contacts due to crossbite and abnormal shape of teeth.
Class II Malocclusion
- Patients may experience a retrognathic(pushed backward) profile
- Smaller facial height
- Oversized maxilla(upper jaw)
- Shorter mandible(lower jaw)
- Retruded or set back chin.
Type 2 Division 1 Malocclusion
Patients might have:
- increased overjet
- increased open bite
- protruded(set forward) upper lips, which distort the ideal facial aesthetic
- forward upper teeth.
Type 2 Division 2 Malocclusion
In this case, the patient has:
- retruded(set back) upper lips
- a concave side profile
- a gummy smile
- inwardly placed upper central incisors
Class III Malocclusion
The patient has:
- a prognathic(forward inclination) profile
- protruded out chin
- increased facial height
- the retruded middle third of the face
- the prominent lower third of the face
- protruded lower teeth
Prevalence of Malocclusion
Malocclusion is one of the most prevalent dental issues in dentistry. Most people suffer from type 1 malocclusion. Among types 2 and 3, the occurrence of type 2 malocclusion is greater than type 3. The prevalence of type 3 malocclusion is less than 8%4Kasparaviciene, K., Sidlauskas, A., Zasciurinskiene, E., Vasiliauskas, A., Juodzbalys, G., Sidlauskas, M., & Marmaite, U. (2014). The prevalence of malocclusion and oral habits among 5-7-year-old children. Medical science monitor: international medical journal of experimental and clinical research, 20, 2036–2042. https://doi.org/10.12659/MSM.890885
Causes of Malocclusion
There are various causes of malocclusion. A few of these are described next:
- Developmental abnormalities like cleft lip and palate cause type 3 malocclusion.
- Pressing of the chin in intrauterine life(the time when the baby is in the body of his mother) results in type 2 malocclusion.
- Skeletal factors like facial trauma or mal-positioned jaws.
- Dental factors also play a significant role in the malocclusion of teeth. For instance, crowding of teeth, missing teeth, or supernumerary teeth.
- Dental caries play a crucial role in tooth loss and improper occlusion.
- Para-functional habits like tooth grinding, bottle feeding for a long time, lip biting, and continuous thumb sucking5Grippaudo, C., Paolantonio, E. G., Antonini, G., Saulle, R., La Torre, G., & Deli, R. (2016). Association between oral habits, mouth breathing and malocclusion. Associazione fra abitudini viziate, respirazione orale e malocclusione. Acta otorhinolaryngologica Italica : organo ufficiale della Societa italiana di otorinolaringologia e chirurgia cervico-facciale, 36(5), 386–394. https://doi.org/10.14639/0392-100X-770

How to Fix Malocclusion of Teeth
Addressing suspected malocclusion in patients requires a systematic approach that ensures accurate diagnosis and effective treatment planning. Adhering to these steps in a sequential manner is pivotal for precise diagnosis and successful resolution of malocclusion-related issues.
Here’s a glimpse into the steps your dental professional will take to guide you through the process:
- History:
Your dental provider will initiate the journey by delving into your comprehensive medical and dental history. This crucial step allows them to understand your unique dental journey, previous treatments, and any underlying medical conditions that may influence the treatment plan. - Examination:
After understanding your history, your dental provider will conduct a thorough dental examination. This encompasses a meticulous assessment of both your upper and lower jaws, as well as an evaluation of the alignment of your teeth. Facial soft tissues and your overall facial profile are also taken into account to provide a holistic perspective. - Imaging:
In certain cases, your dentist might recommend diagnostic imaging to gather more insights. An Orthopantomogram (OPG) provides a comprehensive view of your oral structures, while a Lateral Cephalogram offers valuable information about the relationship between your jaws and teeth. - Dental impression:
Next, your dentist will take an impression of the upper and lower arch(jaw) and study the relationship properly. These impressions serve as a foundation for planning orthodontic interventions tailored to your unique alignment requirements. - Diagnosis:
After completing the study, an accurate diagnosis is made to know the type of malocclusion and intensity of the anomaly. Based on the diagnosis, your dental provider will recommend a treatment approach that aligns with your goals. This might involve orthodontic techniques such as braces or aligners, the use of dental appliances like retainers, or, in complex cases, a combination of orthodontics and surgical interventions.
Treatment of Malocclusion of Teeth
Different types of malocclusion demand different types of treatments. We cannot generalize a single treatment for all the cases. Every case demands its independent attention and treatment plan. The following treatment options are available.
Orthodontic treatment:
In this procedure, teeth are repositioned with the help of orthodontic appliances like braces, brackets, wires, and aligners.
Growth Modification:
This approach is applicable during the developmental stage. It involves targeting the growth patterns of both hard and soft tissues using growth modification appliances like Headgear and chin cups.
Surgical Procedure:
This includes simple procedures like single or multiple teeth extraction and complex procedures like jaw repositioning. Jaw repositioning surgeries address conditions such as underbites, overbites, and crossbites that might not be entirely correctable through non-surgical means.
Type I Malocclusion
Within the framework of Type I Malocclusion, your dental provider may opt for a strategic approach utilizing braces to rectify misalignments. This method effectively addresses concerns such as dental spaces, overcrowding, and the realignment of rotated teeth. Patients have to wear the corrective appliances for almost two to three years with six-month use of retainers to avoid any type of relapse. Corrective appliances are small devices that are manufactured to correct malocclusion of the teeth.
Type II Malocclusion
In cases characterized by Type II Malocclusion, personalized strategies are employed to achieve optimal restoration. These strategies are influenced by the patient’s developmental stage:
1. Growing Age Patients: For those still in their growing phase, the approach entails a combination of growth modification and orthodontic treatment facilitated by specialized orthodontic appliances. This dynamic combination aims to guide the natural growth trajectory toward achieving an improved bite and dental alignment.
2. Post-Growth Phase Patients: Individuals who have surpassed their growth phase are guided toward a comprehensive path. This path involves a harmonious blend of orthognathic (jaw) surgery in tandem with orthodontic treatment. This collaborative approach tackles the malocclusion comprehensively, addressing both skeletal and dental concerns to ensure a balanced and functional occlusion.
In moderate to severe cases, orthodontists may extract the upper first premolars plus the lower second premolars to create space for ideal dental relationships.
Type III Malocclusion
For growing age patients, growth modification and orthodontic treatment aim to correct facial features and maintain balance. Post-growth, corrective surgeries may be considered for severe cases. In severe Type III malocclusion, extractions of lower first premolars, upper second premolars, or both can create space for tooth setbacks. Customized strategies ensure harmony and functionality. However, in certain considerations, other teeth, such as the lower jaw incisor or the first permanent molar, may have been selected 6Jha, A. K., & Chandra, S. (2021). Early Management of Class III Malocclusion in Mixed Dentition. International journal of clinical pediatric dentistry, 14(2), 331–334. https://doi.org/10.5005/jp-journals-10005-1752.
Post-Treatment Retention:
After completion of the treatment phase, patients must undergo the retention period in which patients wear different types of retainers to prevent relapse of soft and hard tissues.

How to Get Rid of Para-functional Habits
When para-functional habits contribute to teeth misalignment, taking swift action is essential. Here’s a concise roadmap to tackle these habits and promote a healthier smile:
- Self-Awareness and Abandoning Habits: Recognize and consciously quit para-functional habits to prevent further dental issues.
- Psychologist Support for Young Patients: Seek professional help for stubborn young patients to overcome these habits under expert guidance.
- Habit-Breaking Appliances: When habits persist, orthodontists may recommend specialized devices to discourage these behaviors.7Abraham R, Kamath G, Sodhi JS, Sodhi S, Rita C, Sai Kalyan S. Habit breaking appliance for multiple corrections. Case Rep Dent. 2013;2013:647649. doi: 10.1155/2013/647649. Epub 2013 Oct 3. PMID: 24198976; PMCID: PMC3808727.
- Orthodontic Appliance Usage: Educate patients on proper orthodontic appliance usage for effective treatment.
- Retention Phase and Retainers: Emphasize retainer use to maintain treatment results and prevent relapse.

Severe Overbite Malocclusion & Under bite Malocclusion
Patients can undertake the surgical procedure with great care and reassure the patient of all the possible complications to avoid any inconvenience in the post-operative phase. So, it is advisable for patients to allow their orthodontists to do mock surgeries on customized models to reduce the chances of relapse.
Conclusion
Only a tiny fraction of the population has perfect occlusion, while the rest suffers from different types of malocclusions. To reduce the incidence of malocclusion of teeth, it is recommended that people should take proper care of their teeth, avoid all types of abnormal habits, and consult a dentist at a young age to avoid severe facial and dental deformities.
Refrences
- 1Masucci, C., Oueiss, A., Maniere-Ezvan, A., Orthlieb, J. D., & Casazza, E. (2020). Qu’est-ce qu’une malocclusion ? [What is a malocclusion?]. L’ Orthodontie francaise, 91(1-2), 57–67. https://doi.org/10.1684/orthodfr.2020.11
- 2Gravely, J. F., & Johnson, D. B. (1974). Angle’s classification of malocclusion: an assessment of reliability. British journal of orthodontics, 1(3), 79–86. https://doi.org/10.1179/bjo.1.3.79
- 3DiBenedetto D. C. (2011). Defining malocclusion. Journal of the American Dental Association (1939), 142(4), 368–369. https://doi.org/10.14219/jada.archive.2011.0178\
- 4Kasparaviciene, K., Sidlauskas, A., Zasciurinskiene, E., Vasiliauskas, A., Juodzbalys, G., Sidlauskas, M., & Marmaite, U. (2014). The prevalence of malocclusion and oral habits among 5-7-year-old children. Medical science monitor: international medical journal of experimental and clinical research, 20, 2036–2042. https://doi.org/10.12659/MSM.890885
- 5Grippaudo, C., Paolantonio, E. G., Antonini, G., Saulle, R., La Torre, G., & Deli, R. (2016). Association between oral habits, mouth breathing and malocclusion. Associazione fra abitudini viziate, respirazione orale e malocclusione. Acta otorhinolaryngologica Italica : organo ufficiale della Societa italiana di otorinolaringologia e chirurgia cervico-facciale, 36(5), 386–394. https://doi.org/10.14639/0392-100X-770
- 6Jha, A. K., & Chandra, S. (2021). Early Management of Class III Malocclusion in Mixed Dentition. International journal of clinical pediatric dentistry, 14(2), 331–334. https://doi.org/10.5005/jp-journals-10005-1752
- 7Abraham R, Kamath G, Sodhi JS, Sodhi S, Rita C, Sai Kalyan S. Habit breaking appliance for multiple corrections. Case Rep Dent. 2013;2013:647649. doi: 10.1155/2013/647649. Epub 2013 Oct 3. PMID: 24198976; PMCID: PMC3808727.

