Yellow Fever is a viral disease that poses a significant public health risk, particularly due to its epidemic-prone nature. It is caused by a flavivirus, which is part of a group of viruses called arboviruses. Arboviruses are viruses that are spread to people through the bite of infected insects like mosquitoes and ticks.
In the case of this fever, the disease is transmitted by the bite of mosquitoes, mainly the Aedes and Haemagogus species. These mosquitoes become infected after biting the primates carrying the virus. The mosquitoes are predominantly found in Africa and South America, breeding in domestic, semi-domestic, and sylvatic (forest or jungle) areas, and are active during the day. The virus spread rapidly in human populations, highlighting the importance of prevention and control measures. The disease presents with a spectrum of symptoms ranging from mild flu-like manifestations to severe and potentially fatal conditions. Symptoms usually appear within three to six days after exposure. This disorder primarily targets internal organs, particularly the liver. The disease’s name is derived from two hallmark symptoms: fever and jaundice (yellowing of the skin).
Annually, an estimated 200,000 cases of this fever result in 30,000 deaths worldwide. The increasing incidence of yellow fever cases is attributed to various factors. These factors include decreased immunity to infectious diseases among the local population, climate change, deforestation, and high-density urbanization. Notably, Yellow fever is a vaccine-preventable disorder.1Gianchecchi, E., Cianchi, V., Torelli, A., & Montomoli, E. (2022). Yellow fever: origin, epidemiology, preventive strategies and future prospects. Vaccines, 10(3), 372.
Causes of Yellow Fever
The causes of this fever are multifaceted. At the most basic level, this fever is caused by an RNA virus. This RNA virus is specifically a member of the genus Flavivirus. It is also known as yellow fever virus (YFV). The positive single standard YFV is transmitted to humans through the bites of infected mosquitoes. As the virus is highly infectious, it can spread rapidly. Casual contact cannot cause this fever in other individuals. However, this infection can be transmitted through contaminated needles into the blood. The transmission cycles are given below.
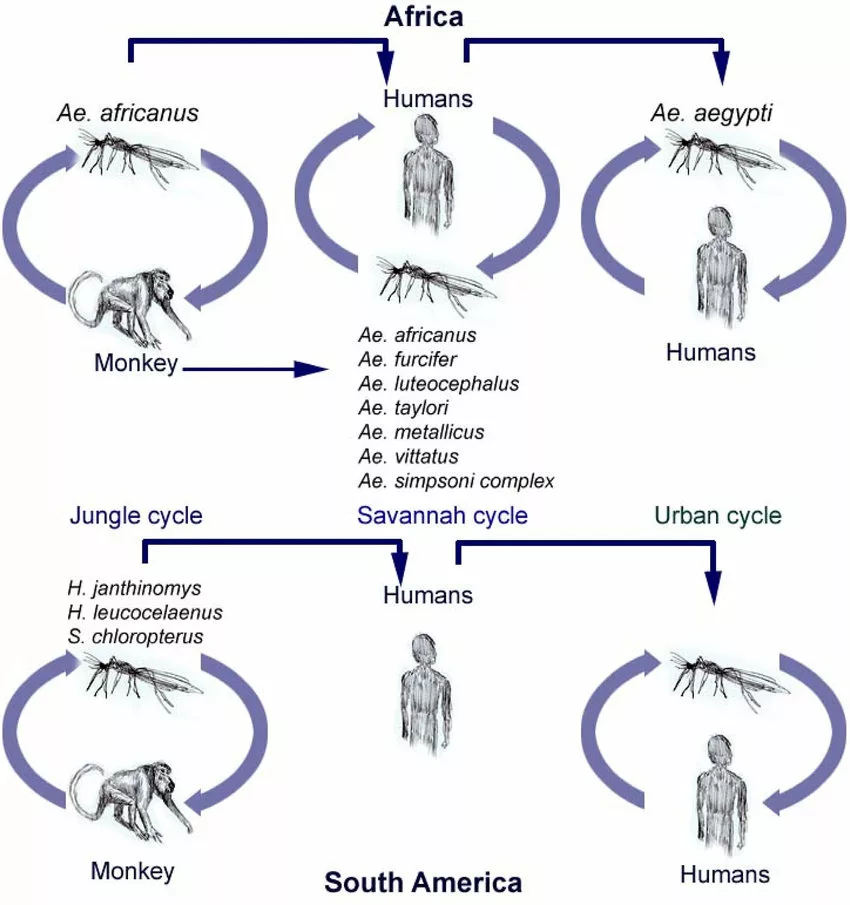
Transmission Cycles:
There are three kinds of transmission cycles of this fever.
The Sylvatic or Jungle Cycle
Wild mosquitoes bite monkeys, causing sylvatic yellow fever. These infected monkeys pass the virus to humans or other monkeys. The virus is transmitted by mosquitoes from monkeys to humans when humans visit or work in the jungle.2Moreira-Soto, A., Torres, M. C., de Mendonça, M. L., Mares-Guia, M. A., dos Santos Rodrigues, C. D., Fabri, A. A., … & de Filippis, A. B. (2018). Evidence for multiple sylvatic transmission cycles during the 2016–2017 yellow fever virus outbreak Brazil. Clinical Microbiology and Infection, 24(9), 1019-e1.
The Intermediate or Savannah Cycle
Intermediate yellow fever is a common type of outbreak in Africa. It occurs when semi-domestic mosquitoes, which breed in areas close to both human settlements and forests, transmit the virus between monkeys and humans. This cycle allows the virus to spread in both animal and human populations.
The Urban Cycle
Urban yellow fever spreads when infected individuals introduce this virus into highly populous areas, most commonly in areas where people have low immunity and a high mosquito density. This fever can not spread without a mosquito vector. But the spread can cause large epidemics.
Occasionally, infected tourists can transfer cases to other states that are free from yellow fever.
Pathophysiology of the Yellow Fever
The pathophysiology of this fever involves a complex interplay of viral replication, immune response, and tissue damage.
Viral Replication
After entering the human body, the virus replicates in the liver, lymph nodes, and spleen. The replication produces viral particles that can spread to other parts of the body. This process increases the amount of viral particles in the blood leading to a peak of viremia. This process takes place within three to five days after infection.
Immune Response
The initial immune response of the body to the virus is characterised by the activation of innate immune cells. These cells (dendritic and macrophages) recognize and engulf the virus. As the infection progresses, the adaptive immune response produces antibodies against the virus. Finally, a cytokine storm (excessive release of pro-inflammatory cytokines) can exacerbate the tissue damage.
Tissue Damage
The YFV primarily targets hepatocytes and causes liver dysfunction and liver damage. Damage to the tissues of the spleen can cause splenomegaly.
Signs & Symptoms
This fever has acquired its name from its two most common symptoms. These are yellowing of the skin and fever. The initial symptoms appear within 3 to 6 days after contact with the virus. Most people have no symptoms. Some represent very mild signs and symptoms. The initial symptoms may improve in less than a week. The most common symptoms are:
- Muscle pain
- Fever
- Headache
- Vomiting
- Black vomit
- Nausea
- Fatigue
- Body ache
- Weakness
In the majority of cases, these symptoms vanish in just three or four days. This phase is called the remission phase.
Only a small percentage of people enter a subsequent phase. This phase is called the toxic phase. Individuals enter it within 24 hours after recovering from mild symptoms.3Litvoc, M. N., Novaes, C. T. G., & Lopes, M. I. B. F. (2018). Yellow fever. Revista da Associação Médica Brasileira, 64, 106-113.
The symptoms of the second phase include:
- A very high fever
- Dark urine
- Jaundice
- Abdominal pain
- Shock
- Organ failure (liver and kidney failure)
- Hemorrhage (bleeding)4Monath, T. P., & Vasconcelos, P. F. (2015). Yellow fever. Journal of Clinical Virology, 64, 160-173.
Bleeding can occur in the eyes, nose, stomach, or mouth. Almost 30 to 60% of the patients who enter the toxic stage die within seven to ten days.
Possible Complications
If left untreated or entered the most severe phase, this fever can result in some complications.5Monath, T. P. (2005). Yellow fever. Medicine, 33(7), 21-23. These include :
- Internal bleeding
- Kidney failure
- Infection of the salivary gland
- Liver failure
- Coma
- Disseminated intravascular coagulation (DIC)
- Shock
- Secondary bacterial infection
- Death
How Can Yellow Fever Be Diagnosed?
If you have visited an area where this fever is found, see your healthcare provider and tell him when and where you have traveled. This fever is usually difficult to diagnose, particularly during the primary stage. The symptoms can also mimic signs of other tropical disorders like typhoid and malaria.
Clinical Evaluation:
The patient’s travel and medical history should be thoroughly assessed, especially any recent visits to endemic regions for yellow fever. During the evaluation, signs of severe illness, such as fever, fatigue, and jaundice, should be noted. In severe cases, Faget’s sign (the paradoxical combination of fever with a slow pulse) may be observed. Physical examination may reveal redness and inflammation of the conjunctiva, as well as petechiae, which are indicative of hemorrhagic manifestations in the advanced stages of the disease.
Laboratory Tests:
Complete Blood Count (CBC) & Blood Chemistry
Leukopenia and thrombocytopenia will indicate severe infection. Elevated liver enzymes and creatine kinase will indicate muscle injury or liver damage.
Polymerase Chain Reaction (PCR)
PCR will detect the yellow fever virus genome in plasma or serum samples.
In later stages, testing to identify antibodies is necessary, such as ELISA (serological testing).6Domingo, C., Charrel, R. N., Schmidt-Chanasit, J., Zeller, H., & Reusken, C. (2018). Yellow fever in the diagnostics laboratory. Emerging microbes & infections, 7(1), 1-15.
Imaging Test
Computed Tomography (CT) or abdominal ultrasound will reveal signs of liver damage or liver enlargement.
Treatment of Yellow Fever
Currently, there are no antiviral medications to treat yellow fever. However, a highly effective vaccine exists to prevent the disease. Although there is no specific cure for yellow fever, supportive management can improve outcomes and help manage symptoms and complications.
Supportive Management:
Supportive management includes the following measures:
Rest & Hydration
Your provider may direct you to drink a lot of water and other fluids to feel better and rest.
Close Monitoring
Yellow fever patients should be closely monitored for signs of worsening disease, like bleeding complications.
Antipyretics & Antiemetics
Antipyretics (acetaminophen) can alleviate initial symptoms of yellow fever. Antiemetics (ondansetron) can be used in case of nausea and vomiting.
If you need a painkiller, avoid painkillers, which can cause bleeding. Avoid using aspirin and non-steroidal anti-inflammatory drugs (NSAIDs). For example, naproxen and ibuprofen may increase the risk of bleeding.
Supportive Management for Severe Form of the Disease:
You will be admitted to the intensive care unit (ICU) in case of a severe form of yellow fever for close monitoring. Aggressive fluid management to prevent dehydration and organ failure in patients.
Management of Manifestations or Complications
Platelet transfusions are needed to correct thrombocytopenia. Coagulation factor replacement can be used to prevent bleeding disorders. In case of severe liver failure, liver transplantation is considered.7Callender, D. M. (2019). Management and control of yellow fever virus: Brazilian outbreak January-April 2018. Global public health, 14(3), 445-455.
Prevention of Yellow Fever
The most effective way to prevent yellow fever is through vaccination. If you are traveling to or living in areas where yellow fever is common, getting vaccinated is crucial.
Vaccine for Yellow Fever:
Vaccination is the most common method of preventing this condition. The vaccine is reasonable and safe. Only a single dose offers lifelong protection. In some cases, a booster dose may be recommended, especially for travelers who have been vaccinated more than ten years ago.
This vaccine offers effective immunity against yellow fever within ten days in 80 to 100% of the vaccinated people. In 30 days, it provides effective immunity to more than 99% of vaccinated people.
This vaccine is recommended for children over nine months and adults.8Monath, T. P. (2005). Yellow fever vaccine. Expert review of vaccines, 4(4), 553-574. Vaccination is also advised for people living in or traveling to countries with a recognized risk of this fever. Latin America and Africa are the states with the highest risk of exposure to this fever. These countries now need evidence of yellow fever vaccination before permitting you to travel there.
Local and state health sectors and travel medicine clinics usually offer this vaccine. If you travel to high-risk countries, repeat the vaccine every ten years. The approved vaccination centers also provide you with an international certificate of vaccination. The certificate will help you travel in high-risk areas.

A yellow fever vaccine booster dose is typically recommended in the following situations:
- Weakened Immune System: If you have a compromised immune system, such as from HIV/AIDS, chemotherapy, or immunosuppressive drugs, a booster may be advised.
- Young Age: If the initial vaccination was given to a child under the age of two years, a booster may be recommended later.
- Bone Marrow Transplant: Individuals who have undergone a bone marrow transplant may need a booster dose due to potential vaccine efficacy concerns.
Side Effects of the Vaccine:
Side effects can occur from the day of vaccination until 14 days after. Contact your provider if you notice flu, fever, or other unusual signs after taking the vaccine. Some of the most common side effects of the vaccine are:
- Headache
- Vomiting
- Nausea
- Muscle pain
- Joint pain
- Soreness at the site of injection
These side effects can last no more than three days.9Barrett, A. D., & Teuwen, D. E. (2009). Yellow fever vaccine—how does it work and why do rare cases of serious adverse events take place?. Current opinion in immunology, 21(3), 308-313.
Rarely can the yellow fever vaccine cause severe side effects. These include:
Although rare, the yellow fever vaccine can cause more severe side effects, including:
- Nervous System Reactions: Inflammation of the spinal cord or brain tissues (encephalitis or myelitis).
- Guillain-Barré Syndrome: An autoimmune disorder where the immune system attacks nerve cells, potentially causing muscle weakness or paralysis.
- Allergic Reactions: Serious allergic reactions, such as anaphylaxis, which can cause difficulty swallowing and breathing.
- Life-threatening Illness: Severe organ dysfunction and other complications in very rare cases.
Contraindications for Yellow Fever Vaccine
Excluded persons from the yellow fever vaccination include:
- Pregnant women
- Infants who are less than nine months old10Roukens, A. H., & Visser, L. G. (2008). Yellow fever vaccine: past, present and future. Expert opinion on biological therapy, 8(11), 1787-1795.
- People with severe lymphoma or leukemia
- People who are on steroids
- People who are undergoing chemotherapy
- People who have a thymus disorder or had it removed
- People with severe allergies to egg proteins
- People over the age of 65
- People who are allergic to any ingredient of the vaccine
Prevention Strategies:
In addition to vaccination, some other tips to prevent this fever include:
- Wear long-sleeved shirts, long pants and socks.
- It is best to wear clothes that are treated to repel mosquitoes.
- Use a mosquito repellent.
- Consider a bed net if the space does not have air conditioning or a screen on the windows.
- Avoid being outdoors during times when these mosquitoes are active. This means dawn to dusk, as the mosquitoes are active during the daytime.
- If you are diagnosed with this fever, continue to cover up. This can prevent a mosquito from biting you and then biting somebody else.
- Keep exact records of international travel days and dates, outdoor activities, and locations. This will help identify a viral infection after your return.
- Eliminate potential breeding sites of mosquitoes to reduce the risk of yellow fever transmission.
Yellow Fever Vs. Malaria
This fever is not the same disease as malaria. But they do not have some things in common.
- Mosquitoes spread both of these disorders.
- Both of them can cause severe sickness, even death and jaundice.
- Both of them can cause other flu-like symptoms and fever.
- Both of them can cause sickness, jaundice, and even death.
But there are significant differences between yellow fever and malaria, such as:
- The virus causes yellow fever, while a parasite causes malaria.
- Mosquitoes that spread yellow fever are different from those that spread malaria. Malaria spreads through the Anopheles, and yellow fever transmission occurs through Haemagogus or Aedes species.
- There is a vaccine to prevent yellow fever. But there is no vaccine to prevent malaria.
- Malaria is treatable, but yellow fever is not.
- Both conditions are life-threatening, but the death rates in malaria are higher.
If you are traveling to an area where malaria is prevalent, talk to your provider about preventive medications.11Okunlola, O. A., & Oyeyemi, O. T. (2022). Malaria transmission in Africa: Its relationship with yellow fever and measles. PloS one, 17(5), e0268080.
Key Facts
- This fever is an infectious disease.
- Initial symptoms are mild. In later stages, the most severe symptoms are jaundice, bleeding, and organ failure.
- There is no specific treatment for this condition. Healthcare providers recommend vaccination. A single dose of vaccine is enough to prevent yellow fever.
- As of 2023, 13 countries in Central and South America, as well as 34 countries in Africa, are endemic for yellow fever.
Final Remarks
Yellow fever is a devastating disease. It requires immediate action and attention. It presents mild to severe symptoms and high mortality rates. In areas where the disease is prevalent, precautions must be followed. Precautions will help in preventing its transmission. Vaccination is the most effective method to prevent yellow fever. Besides vaccination, there are several other preventive measures. These measures include wearing protective clothes and using insect repellents, etc. Travel safety is another important consideration. Consider a booster dose while traveling to areas where yellow fever is prevalent.
Refrences
- 1Gianchecchi, E., Cianchi, V., Torelli, A., & Montomoli, E. (2022). Yellow fever: origin, epidemiology, preventive strategies and future prospects. Vaccines, 10(3), 372.
- 2Moreira-Soto, A., Torres, M. C., de Mendonça, M. L., Mares-Guia, M. A., dos Santos Rodrigues, C. D., Fabri, A. A., … & de Filippis, A. B. (2018). Evidence for multiple sylvatic transmission cycles during the 2016–2017 yellow fever virus outbreak Brazil. Clinical Microbiology and Infection, 24(9), 1019-e1.
- 3Litvoc, M. N., Novaes, C. T. G., & Lopes, M. I. B. F. (2018). Yellow fever. Revista da Associação Médica Brasileira, 64, 106-113.
- 4Monath, T. P., & Vasconcelos, P. F. (2015). Yellow fever. Journal of Clinical Virology, 64, 160-173.
- 5Monath, T. P. (2005). Yellow fever. Medicine, 33(7), 21-23.
- 6Domingo, C., Charrel, R. N., Schmidt-Chanasit, J., Zeller, H., & Reusken, C. (2018). Yellow fever in the diagnostics laboratory. Emerging microbes & infections, 7(1), 1-15.
- 7Callender, D. M. (2019). Management and control of yellow fever virus: Brazilian outbreak January-April 2018. Global public health, 14(3), 445-455.
- 8Monath, T. P. (2005). Yellow fever vaccine. Expert review of vaccines, 4(4), 553-574.
- 9Barrett, A. D., & Teuwen, D. E. (2009). Yellow fever vaccine—how does it work and why do rare cases of serious adverse events take place?. Current opinion in immunology, 21(3), 308-313.
- 10Roukens, A. H., & Visser, L. G. (2008). Yellow fever vaccine: past, present and future. Expert opinion on biological therapy, 8(11), 1787-1795.
- 11Okunlola, O. A., & Oyeyemi, O. T. (2022). Malaria transmission in Africa: Its relationship with yellow fever and measles. PloS one, 17(5), e0268080.

