What is Xanthelasma?
Xanthelasma is a rare and benign skin condition in which yellow patches form near the skin of the eyelid. The yellow lesions may be flat or slightly raised, forming bumps, and the most common site is near the inner canthus (of the upper eyelid).
Xanthelasma is a type of xanthoma, i.e., a condition of localized deposits of fats (lipids) within different organs. Thus, bumps in xanthelasma are composed of cholesterol (lipid) deposits. The plaques may have the following characteristics:
- Semi-solid or chalky
- Soft
- Papular
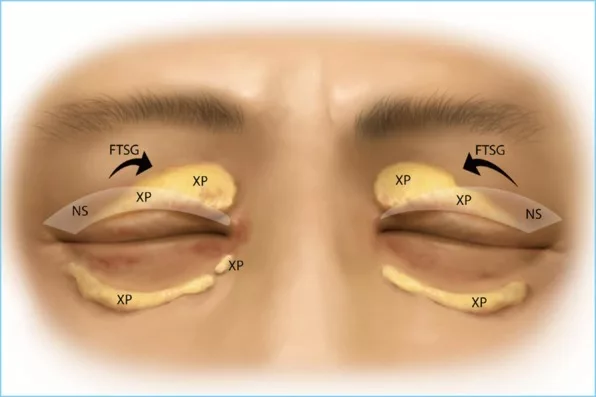
Also known as Xanthelasma palpebrum/palpebrarum (XP), the condition usually indicates underlying health conditions such as hypercholesterolemia (high cholesterol levels), diabetes, and thyroid pathologies. Treatment involves removing the plaques using cryotherapy, laser therapy, and surgical excision. All the modalities are effective in complete removal. However, there is a high rate of recurrence in most patients.
Stages Of Xanthelasma
Based on the location and extent of lesions, it can be classified under the following grades:
- Grade Ⅰ: This is the beginning stage of xanthelasma, characterized by lesion formation in the upper eyelids only.
- Grade Ⅱ: Lesions extend to the medial canthal area of the eye.
- Grade Ⅲ: Yellow lesions spread to the lower eyelids and involve the medial sides of both upper and lower eyelids.
- Grade Ⅳ: Both eyelids are diffusely involved. Lesions are seen on the medial and lateral sides of the eyelids.

Xanthoma Vs. Xanthelasma
A xanthoma refers to a localized deposition of lipids within an organ system. In most cases, xanthomatous lesions correspond to underlying hyperlipidemia. They can develop anywhere, but the most common sites are the hand, elbows, buttocks, and feet. You may also develop them in your joints and tendons.
When a xanthoma develops on the skin, it is termed xanthelasma. It is the most common type of cutaneous xanthoma, having a global prevalence of 1.1-4.4% (1.1% in women and 0.3% in men).1Nair, P. A., & Singhal, R. (2017). Xanthelasma palpebrarum–a brief review. Clinical, cosmetic and investigational dermatology, 1-5.
Xanthelasma Symptoms
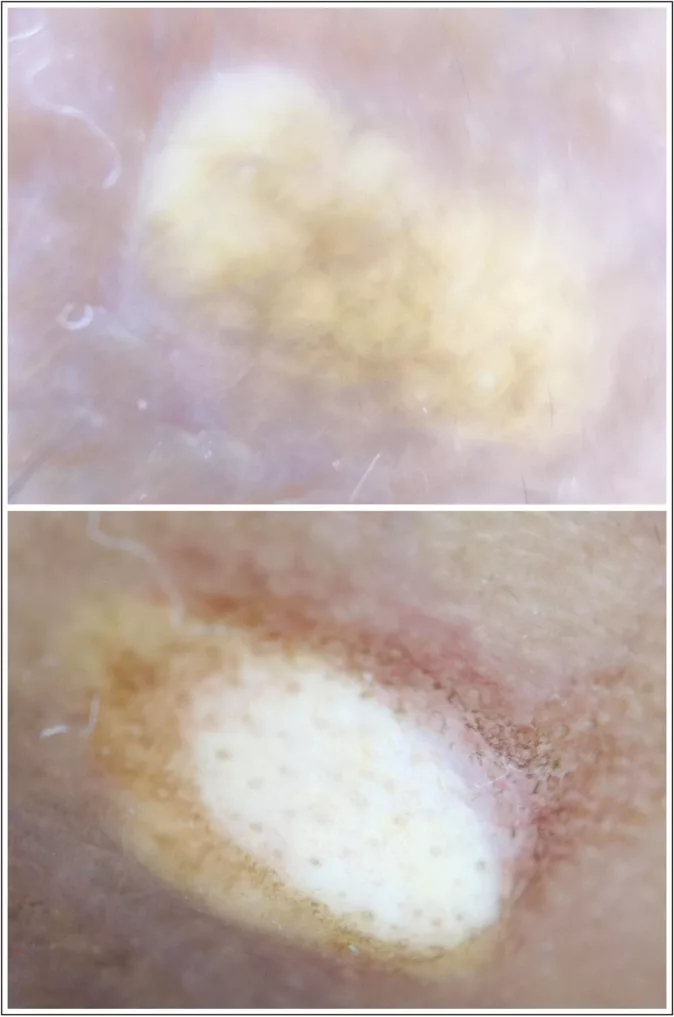
Most patients report the development of yellowish-raised lesions on the eyelid and nose skin. The lesions or papules are not itchy and not painful. The plaques usually have a chalky appearance. However, the presentation can vary from yellow papules to red-brown macules. The consistency can also vary from chalky to semi-solid.2Zak, A., Zeman, M., Slaby, A., & Vecka, M. (2014). Xanthomas: clinical and pathophysiological relations. Biomedical Papers of the Medical Faculty of Palacky University in Olomouc, 158(2). Most patients seek medical help only for aesthetic reasons.
Xanthelasma Causes & Risk Factors
The exact causes of xanthelasma are unknown. However, experts believe individuals with specific underlying comorbidities are at a greater risk of developing xanthelasma palpebrum. Being a woman, aged between 30 and 50 years, predisposes you to skin disease.
The risk groups for xanthelasma include:
Hyperlipidemia & Obesity
The periorbital fat deposits in the skin point towards a deranged lipid profile of the patient. The link between dyslipidemia and xanthelasma is controversial. According to a study in Taiwan, 50% of patients who underwent xanthelasma treatment suffered from hyperlipidemia, while the remaining 50% had optimal lipid profiles. However, the researchers concluded a link between hyperlipidemia and xanthelasma.3Wang, K. Y., Hsu, K. C., Liu, W. C., Yang, K. C., & Chen, L. W. (2018). Relationship between xanthelasma palpebrarum and hyperlipidemia. Annals of plastic surgery, 80(2S), S84-S86.
It was revealed in a 2020 study that there is no association between xanthelasma and serum levels of cholesterol (hypercholesterolemia), LDL, HDL, and triglycerides.4Kampar, P., Anum, Q., & Lestari, S. (2020). The correlation between lipid profile and xanthelasma. Berkala Ilmu Kesehatan Kulit dan Kelamin-Periodical of Dermatology and Venereology, 32(2), 119-25. On the contrary, a 2022 study found an 80% prevalence of dyslipidemia in xanthelasma patients.5Rai, A., Karki, S., Sah, S. P., Kamat, L. N., & Pradhan, M. (2022). Dyslipidemia in Patients with Xanthelasma Palpebrarum Visiting the Department of Dermatology of a Tertiary Care Centre: A Descriptive Cross-sectional Study. JNMA: Journal of the Nepal Medical Association, 60(250), 529. Moreover, metabolic syndrome and obesity are present in several xanthelasma patients.6Agarwal, K., Saikia, P., & Podder, I. (2022). Metabolic syndrome and dyslipidemia in xanthelasma palpebrarum and associated risk–2 factors–A case‐control study. Journal of Cosmetic Dermatology, 21(12), 7018-7024.
Genetics
A family history of hypercholesterolemia/hyperlipidemia may play a role. The latest research highlights the role of genetically predicted plasma proteins in disease occurrence. Evidence suggests that serum levels of 12 plasma proteins (genetically predicted) are associated with XP.7Hu, W., Liu, Y., Lian, C., & Lu, H. (2024). Genetic insight into putative causes of xanthelasma palpebrarum: a Mendelian randomization study. Frontiers in Immunology, 15, 1347112.
Smoking
Many regard smoking as a significant risk factor for periorbital hyperpigmentation and XP. In a study, almost 49% of xanthelasma patients were smokers. This factor is closely followed by obesity and hyperlipidemia.8Platsidaki, E., Kouris, A., Agiasofitou, E., Antoniou, C., & Kontochristopoulos, G. (2016). Periorbital hyperpigmentation in patients with xanthelasma palpebrarum: an interesting observation. The Journal of Clinical and Aesthetic Dermatology, 9(4), 52.
Nicotine addiction is recognized as a major risk factor for XP. Around 40% of XP cases have a smoking history. Moreover, obese smokers are at a greater risk of developing cardiovascular pathologies.9Dey, A., Aggarwal, R., & Dwivedi, S. (2013). Cardiovascular profile of xanthelasma palpebrarum. BioMed Research International, 2013.
Diabetes
A significant number of xanthelasma patients suffer from diabetes mellitus and metabolic syndrome.10Gondane, S., Meherda, A., & Kothiwala, R. (2020). To study the prevalence of metabolic syndrome and dyslipidemia in patients of xanthelasma palpebrarum at a tertiary care hospital. Asian Journal of Diabetology, 21(3), 10-14. Several diabetes patients suffer from central obesity and deranged lipid profiles. This further predisposes them to the periorbital skin condition.
Thyroid Issues
Hypothyroidism can cause multiple cutaneous changes. Largely hypothyroidism, but rarely, hyperthyroidism can also lead to skin and hair defects.11Bains, A., Tegta, G. R., & Vedant, D. (2019). A cross-sectional study of cutaneous changes in patients with acquired thyroid disorders. Clinical Dermatology Review, 3(1), 72-77. In a case report, a hyperthyroid patient suffered from multiple xanthomas.12Khondker, L., & Huda, F. (2017). Multiple xanthomas in a patient with hypothyroidism: A case report and review of the literature. The Gulf journal of dermatology & venereology, 24(2), 37-46. This can be attributed to lipid profile dysregulation in thyroid patients.
Cosmetic Procedures
In the modern world, numerous men and women opt for cosmetic procedures to enhance their looks. Very rarely, these procedures can lay the foundation for xanthelasma. Per a case report, a 38-year-old woman developed xanthelasma after undergoing hyaluronic acid fillers in the periorbital area of both eyes. The patient reported xanthelasma lesions but didn’t have a history of hyperlipidemia.13Simões Pires, V., Wender, I. O., Santos, M. F., Sartori, G. L., Vivian, A., & Dallagnese, G. (2021). Xanthelasma palpebrarum after hyaluronic acid injection in the lower eyelid: A case report and review of the literature. Journal of cosmetic dermatology, 20(9), 2750-2752. Therefore, dermatologists should be aware of this type of adverse reaction of injectable fillers.
How To Diagnose Xanthelasma?
Your doctor will visually examine the yellow XP lesions. The lesions are well-circumscribed and may be slightly raised from the surrounding skin. Multiple xanthelasmas can occur. The disease is graded based on the extent of eyelid involvement.
Your healthcare provider will also order lipid profile tests to rule out underlying hyperlipidemia. These blood tests check serum cholesterol levels, High-density Lipoproteins (HDL), and Low-density Lipoproteins (LDL). Other tests include blood sugar levels and thyroid function tests.
Complications Of Xanthelasma

Xanthelasma may arise due to excess cholesterol in the body. While cholesterol accumulation in the eyelid skin can be a cosmetic concern, deposition within the arteries can lead to serious conditions like atherosclerosis.
Atherosclerosis is a condition of plaque (fat) buildup in the inner layer of the arteries. This problem is interlinked with other pathologies like hypertension and cardiovascular disease. Studies show that XP and cardiovascular pathologies have similar mechanisms of development; thus, xanthelasma patients are at a greater risk of cardiovascular disease.14Lousa, R., Alves, M., Mota, C., Brito, D., Almeida, A. G., Pinto, F. J., & Caldeira, D. (2022). The association of xanthelasma palpebrum with cardiovascular events: systematic review with meta-analysis. European Journal of Preventive Cardiology, 29(13), 1740-1743.
Xanthelasma Treatment
The skin condition is benign and does not cause harm apart from esthetic concerns. Xanthelasma removal is the most common treatment procedure. Multiple effective ways exist to remove xanthelasma lesions. However, there is a high rate of recurrence.
Methods to remove xanthelasma include:
Laser Therapy
Different types of lasers are safe and have shown promising results in Xanthelasma removal. Multiple laser therapy sessions (depending on the severity of the condition) can completely remove xanthelasma lesions.
Ablative fractional laser therapy
Ablative fractional laser therapy using carbon dioxide (CO2) leads to completely removing the lesions. This gives superior results when combined with cryotherapy.15Jeong, B. H., Na, C. H., & Kim, M. S. (2021). The therapeutic outcome of xanthelasma treated with cryotherapy and fractional CO 2 laser. 프로그램북 (구 초록집), 73(1), 352-352. The ultra pulse CO2 laser helps remove XP-affected skin without complications or side effects. No recurrence was noted in subjects till 6 months after treatment.16RAMTEKE, M. N., & KHEMANI, U. N. (2021). A Prospective Interventional Study of Xanthelasma Palpebrarum Treated with Ultrapulse Carbon Dioxide Laser. Journal of Clinical & Diagnostic Research, 15(8). An ablative YAG laser is also efficacious and safe in improving the skin condition of XP patients.17Soliman, M. M., El Diasty, E. Y., Ibrahim, N. F., & Tawfik, A. A. (2023). Fractional Erbium YAG laser versus pulsed dye laser in the treatment of Xanthelasma palpebrarum: Randomized comparative intrapatient study. Journal of Radiation Research and Applied Sciences, 16(4), 100657.
Non-Ablative Laser
Moreover, you can get treated with a non-ablative laser. Treatment with a pulsed dye laser is a relatively patient-friendly procedure. It is painless with minimal to no post-procedure complications (swelling, scarring, etc.). There is a complete clearance of the skin and no recurrence. Additionally, modern doctors have effectively treated XP with fractional plasma instead of lasers.18CHELES, D. (2021). Treatment of xanthelasma with fractional plasma. This technique utilizes plasma instead of lasers to remove xanthelasma.
Chemical Peels
Topical application of Trichloroacetic acid (95%) helps ease the surgical removal of the yellow skin. A chemical peel can reduce small-sized lesions, and when compared, a fractional laser has the upper hand.19Al‐Kady, N. A. S., Hamdino, M., & Abdel Kawy, F. A. W. (2021). Fractional CO2 laser versus trichloroacetic acid 50% for xanthelasma palpebrarum therapy. Journal of cosmetic dermatology, 20(3), 763-768. However, it has proven to be an effective and inexpensive adjunct for surgical excision of XP.20Osaki, T. H., & Osaki, M. H. (2019). Management of diffuse xanthelasma palpebrarum using trichloroacetic acid application to reduce lesions followed by surgical excision. Aesthetic Surgery Journal, 39(1), NP6-NP8.
Some physicians suggest injecting intradermal heparin for grade Ⅰ and Ⅱ xanthelasma lesions. This is a cost-effective technique. However, an ablative CO2 laser is the treatment of choice for advanced stages.21Neinaa, Y. M. E. H., Awara, B. S. E. S., Shalaby, O. E. S., & Abd El‐Naby, N. M. (2023). Clinical and dermoscopic assessment of ablative carbon dioxide laser versus intradermal heparin sodium in xanthelasma. Photodermatology, Photoimmunology & Photomedicine, 39(6), 648-656.
Cryotherapy
Cold therapy or cryotherapy is an effective way to remove benign skin growths non-surgically. The doctor applies liquid nitrogen on the lesions using a spraying device, a cryoprobe, or a cotton swab. Liquid nitrogen cryotherapy is effective. However, doctors rarely adopt it due to a high risk of eyelid swelling.22Labandeira, J., Vázquez‐Osorio, I., Figueroa‐Silva, O., Pereiro Jr, M., & Toribio, J. (2015). Tolerability and effectiveness of liquid nitrogen spray cryotherapy with very short freeze times in the treatment of xanthelasma palpebrarum. Dermatologic Therapy, 28(6), 346-350.
Radiofrequency Advanced Electrolysis (RAF)
Advanced electrolysis is a procedure in which current is passed through the skin to cauterize blemishes and skin lesions. Passing of the thermolysis current helps achieve cosmetic results. A study showed that radiofrequency advanced electrolysis removes XP plaques and has great patient outcomes.23Smith, V., Santos, S. D., & Whiteley, M. (2015). Treatment of xanthelasma palpebrarum using radiofrequency advanced electrolysis. Journal of Aesthetic Nursing, 4(8), 385-389.
Conventional Surgery
Despite the success of minimally invasive procedures, experts believe traditional surgery (excision using a scalpel/surgical knife) is the best way to treat xanthelasma palpebrum. Numerous clinical studies advocate using surgery for xanthelasma due to its effectiveness and high patient satisfaction rates. Many believe it should be the first therapeutic option in XP management.24DORNELAS, M. T., PEDROSA, N. V., DORNELAS, G. V., CHAOUBAH, A., FERNANDES, A. D. S., CARVALHO, E. D. L., … & BELGO, T. R. R. (2023). Eyelid Xanthelasma: surgical treatment as the first choice. Revista Brasileira de Cirurgia Plástica, 37, 498-504.
How To Prevent Recurrence?
The recurrence of xanthelasma is very common. Therefore, you should modify your lifestyle to minimize the chances of redevelopment. Hyperlipidemia is the major suspected cause of XP. Therefore, it is crucial to manage your cholesterol levels.
How Can You Manage Cholesterol Levels?
- Medications: Most doctors prescribe statin drugs such as rosuvastatin and simvastatin to lower cholesterol levels.
- Exercise and weight maintenance: Perform exercise regularly and maintain an optimal weight profile.
- Dietary modifications: Limit fatty foods (saturated fats) such as cheese, butter, bacon, etc.
- Lifestyle modifications: Quit smoking and limit alcohol consumption to keep your arteries and body free of cholesterol deposits.
Final Word
Xanthelasma or Xanthelasma palpebrum is a benign condition of the skin in which yellow plaques of cholesterol form on the eyelid and nose region. It is mostly linked to underlying hyperlipidemia, diabetes, and thyroid issues. As it may be linked to increased cholesterol levels in the body, xanthelasma patients are more likely to suffer from serious complications such as atherosclerosis, hypertension, and coronary artery disease. The growths of XP are harmless, and most patients seek treatment for esthetic purposes. The most common and effective treatment modalities are laser therapy (ablative carbon dioxide, YAG lasers, and non-ablative pulsed dye lasers) and surgical excision. However, in treatment, there are high recurrence rates. You should maintain an optimal lipid profile and ideal weight to prevent this.
Refrences
- 1Nair, P. A., & Singhal, R. (2017). Xanthelasma palpebrarum–a brief review. Clinical, cosmetic and investigational dermatology, 1-5.
- 2Zak, A., Zeman, M., Slaby, A., & Vecka, M. (2014). Xanthomas: clinical and pathophysiological relations. Biomedical Papers of the Medical Faculty of Palacky University in Olomouc, 158(2).
- 3Wang, K. Y., Hsu, K. C., Liu, W. C., Yang, K. C., & Chen, L. W. (2018). Relationship between xanthelasma palpebrarum and hyperlipidemia. Annals of plastic surgery, 80(2S), S84-S86.
- 4Kampar, P., Anum, Q., & Lestari, S. (2020). The correlation between lipid profile and xanthelasma. Berkala Ilmu Kesehatan Kulit dan Kelamin-Periodical of Dermatology and Venereology, 32(2), 119-25.
- 5Rai, A., Karki, S., Sah, S. P., Kamat, L. N., & Pradhan, M. (2022). Dyslipidemia in Patients with Xanthelasma Palpebrarum Visiting the Department of Dermatology of a Tertiary Care Centre: A Descriptive Cross-sectional Study. JNMA: Journal of the Nepal Medical Association, 60(250), 529.
- 6Agarwal, K., Saikia, P., & Podder, I. (2022). Metabolic syndrome and dyslipidemia in xanthelasma palpebrarum and associated risk–2 factors–A case‐control study. Journal of Cosmetic Dermatology, 21(12), 7018-7024.
- 7Hu, W., Liu, Y., Lian, C., & Lu, H. (2024). Genetic insight into putative causes of xanthelasma palpebrarum: a Mendelian randomization study. Frontiers in Immunology, 15, 1347112.
- 8Platsidaki, E., Kouris, A., Agiasofitou, E., Antoniou, C., & Kontochristopoulos, G. (2016). Periorbital hyperpigmentation in patients with xanthelasma palpebrarum: an interesting observation. The Journal of Clinical and Aesthetic Dermatology, 9(4), 52.
- 9Dey, A., Aggarwal, R., & Dwivedi, S. (2013). Cardiovascular profile of xanthelasma palpebrarum. BioMed Research International, 2013.
- 10Gondane, S., Meherda, A., & Kothiwala, R. (2020). To study the prevalence of metabolic syndrome and dyslipidemia in patients of xanthelasma palpebrarum at a tertiary care hospital. Asian Journal of Diabetology, 21(3), 10-14.
- 11Bains, A., Tegta, G. R., & Vedant, D. (2019). A cross-sectional study of cutaneous changes in patients with acquired thyroid disorders. Clinical Dermatology Review, 3(1), 72-77.
- 12Khondker, L., & Huda, F. (2017). Multiple xanthomas in a patient with hypothyroidism: A case report and review of the literature. The Gulf journal of dermatology & venereology, 24(2), 37-46.
- 13Simões Pires, V., Wender, I. O., Santos, M. F., Sartori, G. L., Vivian, A., & Dallagnese, G. (2021). Xanthelasma palpebrarum after hyaluronic acid injection in the lower eyelid: A case report and review of the literature. Journal of cosmetic dermatology, 20(9), 2750-2752.
- 14Lousa, R., Alves, M., Mota, C., Brito, D., Almeida, A. G., Pinto, F. J., & Caldeira, D. (2022). The association of xanthelasma palpebrum with cardiovascular events: systematic review with meta-analysis. European Journal of Preventive Cardiology, 29(13), 1740-1743.
- 15Jeong, B. H., Na, C. H., & Kim, M. S. (2021). The therapeutic outcome of xanthelasma treated with cryotherapy and fractional CO 2 laser. 프로그램북 (구 초록집), 73(1), 352-352.
- 16RAMTEKE, M. N., & KHEMANI, U. N. (2021). A Prospective Interventional Study of Xanthelasma Palpebrarum Treated with Ultrapulse Carbon Dioxide Laser. Journal of Clinical & Diagnostic Research, 15(8).
- 17Soliman, M. M., El Diasty, E. Y., Ibrahim, N. F., & Tawfik, A. A. (2023). Fractional Erbium YAG laser versus pulsed dye laser in the treatment of Xanthelasma palpebrarum: Randomized comparative intrapatient study. Journal of Radiation Research and Applied Sciences, 16(4), 100657.
- 18CHELES, D. (2021). Treatment of xanthelasma with fractional plasma.
- 19Al‐Kady, N. A. S., Hamdino, M., & Abdel Kawy, F. A. W. (2021). Fractional CO2 laser versus trichloroacetic acid 50% for xanthelasma palpebrarum therapy. Journal of cosmetic dermatology, 20(3), 763-768.
- 20Osaki, T. H., & Osaki, M. H. (2019). Management of diffuse xanthelasma palpebrarum using trichloroacetic acid application to reduce lesions followed by surgical excision. Aesthetic Surgery Journal, 39(1), NP6-NP8.
- 21Neinaa, Y. M. E. H., Awara, B. S. E. S., Shalaby, O. E. S., & Abd El‐Naby, N. M. (2023). Clinical and dermoscopic assessment of ablative carbon dioxide laser versus intradermal heparin sodium in xanthelasma. Photodermatology, Photoimmunology & Photomedicine, 39(6), 648-656.
- 22Labandeira, J., Vázquez‐Osorio, I., Figueroa‐Silva, O., Pereiro Jr, M., & Toribio, J. (2015). Tolerability and effectiveness of liquid nitrogen spray cryotherapy with very short freeze times in the treatment of xanthelasma palpebrarum. Dermatologic Therapy, 28(6), 346-350.
- 23Smith, V., Santos, S. D., & Whiteley, M. (2015). Treatment of xanthelasma palpebrarum using radiofrequency advanced electrolysis. Journal of Aesthetic Nursing, 4(8), 385-389.
- 24DORNELAS, M. T., PEDROSA, N. V., DORNELAS, G. V., CHAOUBAH, A., FERNANDES, A. D. S., CARVALHO, E. D. L., … & BELGO, T. R. R. (2023). Eyelid Xanthelasma: surgical treatment as the first choice. Revista Brasileira de Cirurgia Plástica, 37, 498-504.