Acute Pancreatitis is inflammation of the pancreas that happens suddenly. The enzymes in your pancreas start attacking your tissue, which leads to intense pain, impaired digestion, and organ damage.
What is Acute Pancreatitis?
Acute pancreatitis is when your pancreas suddenly becomes inflamed. It causes severe abdominal pain and other serious health issues. This happens because the digestive enzymes inside your pancreas start working too early and begin to damage your pancreatic tissue.
Acute pancreatitis happens all over the world and is one of the most common emergencies involving your digestive system. It affects about 5 to 30 people out of every 100,000 each year, with higher rates in developed countries. While it can affect people of any age, you are more likely to get it if you’re between 30 and 50 years of age. The condition was first described in detail by the French doctor Jean Cruveilhier in the early 1800s.1Roberts, S. E., Akbari, A., Thorne, K., Atkinson, M., & Evans, P. A. (2013). The incidence of acute pancreatitis: impact of social deprivation, alcohol consumption, seasonal and demographic factors. Alimentary Pharmacology & Therapeutics, 38(5), 539–548. https://doi.org/10.1111/apt.12408
What causes Acute Pancreatitis?
Acute pancreatitis can be idiopathic (without a pinpointed cause) or a result of a number of factors. These causes of acute pancreatitis include:
Gallstones:
Gallstones are the most common cause of acute pancreatitis. If you have gallstones, they can get stuck in the opening of your pancreas (called the ampulla) and block the flow of digestive juices. This blockage causes pressure and irritation inside your pancreas and leads to inflammation. This type of pancreatitis can happen suddenly and is more common in women, especially during their third trimester of pregnancy.

Alcohol:
Drinking large amounts of alcohol regularly puts you at risk for acute pancreatitis. Your pancreas breaks down alcohol into toxic substances that harm the cells inside it. This damage causes inflammation and sometimes permanent scarring. Sometimes, even short periods of heavy drinking can trigger pancreatitis if you’re sensitive to alcohol.
Genetic Factors:
If pancreatitis runs in your family, you might have inherited a gene that makes you more likely to get it. For example, mutations in the cationic trypsinogen gene cause many cases of pancreatitis. Also, if you have cystic fibrosis, the gene changes can increase your chances of repeated pancreatitis attacks.
Medical Procedures:
If you undergo an ERCP (endoscopic retrograde cholangio-pancreatography) procedure, which examines your bile and pancreatic ducts, there is a small risk (about 5 to 8%) that it may cause pancreatitis. This usually happens within a few days after the procedure and is mostly mild or moderate.
High Blood Fat Levels or Hypertriglyceridemia:
If your blood contains very high levels of triglycerides — over 1000 mg/dL — this can trigger pancreatitis. This is often linked to uncontrolled diabetes or certain inherited conditions.
Medications:
Some medicines can cause pancreatitis as a side effect. These include drugs like:
- Azathioprine
- Antibiotics (like tetracycline)
- Diuretics (water pills)
- Anti-seizure and psychiatric medications
Infections:
Certain infections, such as the mumps virus, hepatitis B or C, and some bacterial infections, cause your pancreas to become inflamed.
Trauma:
If your abdomen gets hit hard or you have surgery near your pancreas, this trauma can cause pancreatitis.
Autoimmune:
Sometimes your immune system mistakenly attacks your pancreas, causing inflammation. This is called autoimmune pancreatitis and may require special treatment.
Blockage by Tumors or Cysts:
Rarely, tumors, cysts, or scarring inside your pancreatic duct can block digestive juices and cause pancreatitis.2Bartel, M. (2024, March 4). Acute Pancreatitis. MSD Manual Consumer Version; MSD Manuals. https://www.msdmanuals.com/home/digestive-disorders/pancreatitis/acute-pancreatitis
Symptoms of Acute Pancreatitis
When you develop acute pancreatitis, you typically experience a sudden onset of symptoms. Some pancreatitis symptoms include.
- Fever
- Tachycardia
- Jaundice if bile flow is blocked
- Rapid breathing
- Trouble breathing
- Shock
Some specific symptoms of acute pancreatitis are detailed below:
Abdominal Pain:
The most characteristic symptom is severe abdominal pain. You’ll often feel a dull and constant ache in your upper abdomen. This pain usually starts suddenly and worsens gradually until it becomes constant. It commonly radiates through your abdomen to your back, sometimes between your shoulder blades.
Moreover, your abdomen is often tender to touch, with muscle guarding and possible swelling. You might notice that bowel sounds are decreased or absent, indicating reduced intestinal movement.

Nausea & Vomiting:
You may also experience nausea and repeated vomiting, which can worsen your discomfort and contribute to dehydration. Often, you’ll lose your appetite during an episode.
Diarrhea:
Some patients notice loose, watery stools due to impaired digestion as a result of pancreatic enzyme disruption.
Cullen Sign:
The Cullen sign is a blue-colored discoloration around your belly button caused by bleeding into the abdominal tissues.
Grey-Turner Sign:
If you have had internal bleeding, there could be reddish-brown bruising along your sides, which is referred to as the Grey-Turner sign.3Acute pancreatitis. (2024). Patient.info. https://patient.info/digestive-health/gallstones-and-bile/acute-pancreatitis
Complications of Acute Pancreatitis
Sometimes, pancreatitis can lead to complications that affect not only your pancreas but also other organs as well.
Necrotizing Pancreatitis:
In severe cases, parts of your pancreas tissue lose blood supply and die. This process is called necrosis. The dead tissue can become infected, which increases your risk of serious infections, e.g,. You can develop pockets of pus called pancreatic abscesses. These require drainage or surgery.
Pancreatic Pseudocysts:
Sometimes, fluid and enzymes leak out of your inflamed pancreas and collect in a sac-like structure called a pseudocyst. These cysts don’t have a true lining like normal cysts, but can grow large. These cause abdominal pain, blockages of nearby organs, or become infected.
Respiratory Complications:
You might develop acute respiratory distress syndrome, where inflammation causes fluid buildup in your lungs. This often requires intensive care and mechanical ventilation.
Hypocalcemia:
Low calcium levels can occur because calcium binds with fat released from your damaged pancreas. This can cause muscle spasms or cramps, especially in your hands and feet.
Hemorrhage & Shock:
Your inflamed pancreas or surrounding blood vessels may bleed internally. This bleeding can cause a drop in your blood pressure (shock), requiring urgent blood transfusions and intervention.
Multi-Organ Failure:
Your body’s reaction to pancreatic inflammation can cause widespread inflammation throughout your bloodstream, known as SIRS. This may affect your lungs, kidneys, and heart. It can worsen to multiple organ failure and death if not treated at once.4Lucocq, J., & Sanjay Pandanaboyana. (2024). Acute pancreatitis. Surgery (Oxford). https://doi.org/10.1016/j.mpsur.2024.10.005
Phases of Acute Pancreatitis
Acute pancreatitis has two main phases:
Early Phase of Acute Pancreatitis:
This happens in the first week. Your body reacts to the inflammation with symptoms like pain, fever, and vomiting. You may also have low blood pressure or trouble breathing if the inflammation is severe. Most people get better during this phase with supportive care.
Late Phase of Acute Pancreatitis:
The late phase of acute pancreatitis comes after the first week, especially if the disease is severe. You might develop complications like infected fluid collections or dead tissue in the pancreas. This phase can last for weeks and may need special treatments like drainage or surgery.
Classification of Acute Pancreatitis
Acute pancreatitis is divided into three types based on how serious it is:5Gapp, J., Tariq, A., & Chandra, S. (2023, February 9). Acute Pancreatitis. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK482468/
| Type of Acute Pancreatitis | Description |
| Mild acute pancreatitis | You may feel sick, but your organs work normally. Most people get better in a few days with treatment. |
| Moderately severe acute pancreatitis | You might have some short-term problems like fluid around your pancreas or mild organ damage. These can usually improve without serious damage. |
| Severe acute pancreatitis | One or more of your organs, like your lungs or kidneys, may stop working. It can lead to infection, dead tissue, and serious long-term problems. You may need treatment in the ICU. |
How is an Acute Pancreatitis diagnosis established?
To diagnose acute pancreatitis, your doctor will confirm if you have at least two out of the following three features:
- You must have typical abdominal pain, which usually comes on suddenly in the upper abdomen (epigastric area), is severe, and may radiate to your back. You might also feel nauseated or vomit alongside this pain.
- You should have blood tests showing amylase or lipase levels that are more than three times the upper normal limit. Lipase is generally more reliable than amylase because it stays elevated longer and is more specific to the pancreas.
- You might undergo imaging tests like a contrast-enhanced CT scan, MRI, or ultrasound, especially if the diagnosis is unclear. These can show characteristic signs such as pancreatic swelling, fluid collections, or fat stranding around your pancreas.
- You only need two of these three features to be diagnosed with acute pancreatitis, so if your pain and enzyme levels are classic, you may not need imaging right away.
History & Physical Exam:
When you come to the hospital with acute pancreatitis, your doctor will start by asking questions about your symptoms. Most people with acute pancreatitis feel sudden, severe pain in the upper belly that often spreads to the back. Your doctor may ask if you recently drank a lot of alcohol, had a big meal, or have a history of gallstones.
During the physical exam, your doctor will gently press on your belly to check for tenderness, swelling, or guarding (when your muscles tighten while being touched). You may look sick, lie still because movement worsens pain, or breathe shallowly to avoid belly movement. Your doctor might check your heart rate, breathing, and blood pressure for signs of dehydration or infection. If the condition is severe, you could show signs like low blood pressure, confusion, or yellowing of the skin or eyes. Your doctor might also look for special signs like Cullen’s sign or Grey-Turner’s sign.
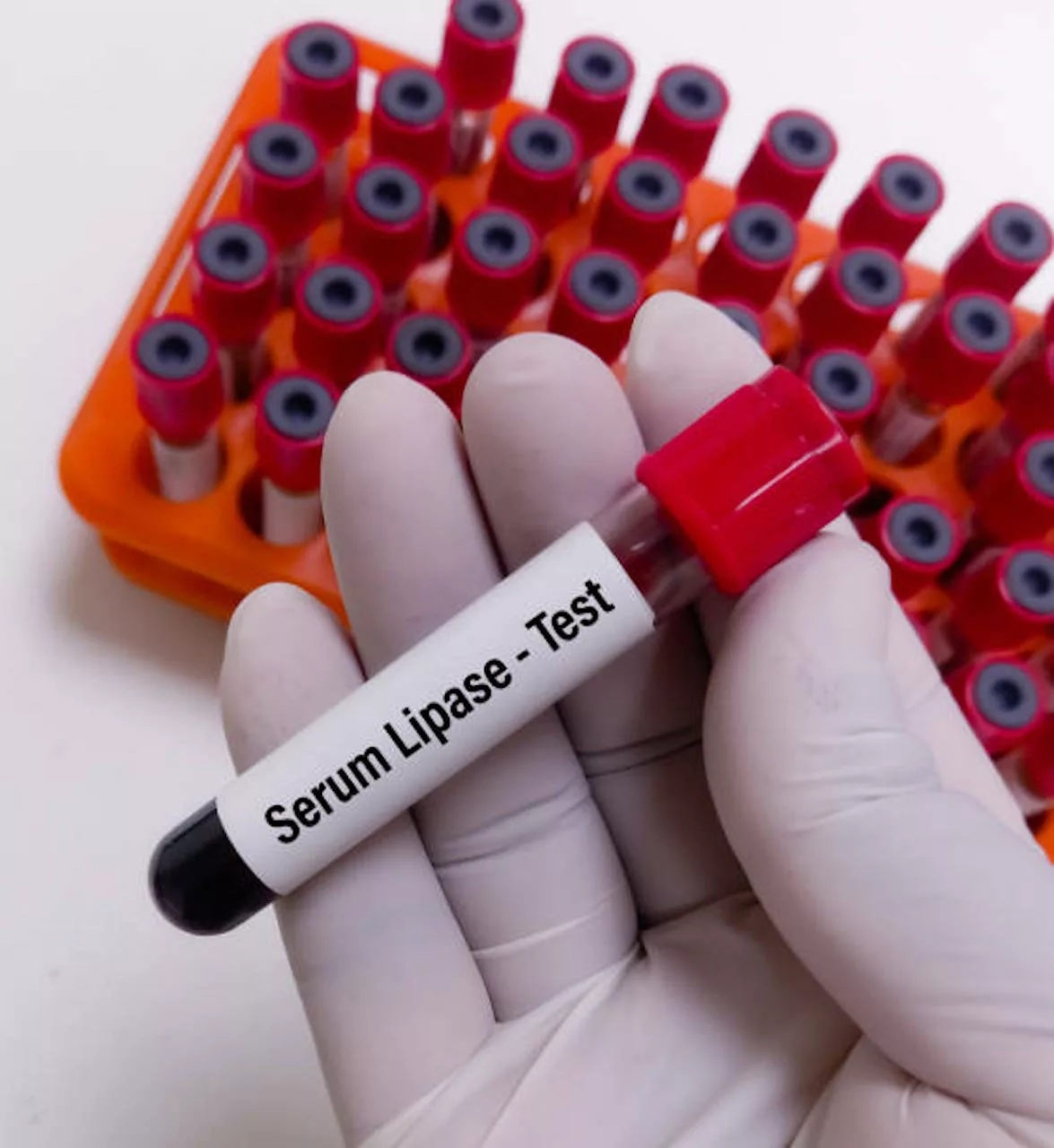
Blood Tests:
A variety of blood tests are performed to diagnose acute pancreatitis.
- Blood tests check the levels of amylase and lipase, enzymes made by the pancreas. A high level of lipase is usually a strong sign of pancreatitis.
- Liver tests are done to check if gallstones are blocking bile flow.
- Blood sugar, calcium, and fat levels are tested, as these can be related to pancreatitis.
- Kidney function tests and electrolytes help assess how your body is coping.
- A complete blood count checks for infection or severe inflammation.
- A test called CRP may be done after 48 hours to measure how much inflammation is present.
Imaging:
Imaging is used to support a provisional diagnosis of acute pancreatitis.
- An ultrasound is often the first scan used to look for gallstones and see if the pancreas is swollen.
- A CT scan gives detailed imaging of the pancreas and can show if there are any complications. Diagnosis of infection may include a CT scan showing gas bubbles or a fine needle test with positive bacterial results.
- An MRI or MRCP provides clear images of the bile and pancreatic ducts without using radiation.
- An X-ray is done to rule out other problems, like a hole in the stomach or intestine.6Szatmary, P., Grammatikopoulos, T., Cai, W., Huang, W., Mukherjee, R., Halloran, C., Beyer, G., & Sutton, R. (2022). Acute Pancreatitis: Diagnosis and Treatment. Drugs, 82(12), 1251–1276. https://doi.org/10.1007/s40265-022-01766-4
What do I need to know about Acute Pancreatitis treatment?
Despite being a “surgical” condition, acute pancreatitis doesn’t need surgery in the early stages. Acute pancreatitis treatment options include:
Medications:
Medicines are used to manage pain, control symptoms, and treat or prevent infection if needed.
- Pain relief is usually given through intravenous medications to help ease discomfort.
- Antibiotics are only used if there is a confirmed or suspected infection in the pancreas.
- If infection is suspected, doctors may start antibiotics while looking for the cause, but these are stopped if no infection is found.
- Preventive antibiotics are not recommended, even in severe or necrotizing pancreatitis.
- Medicines like octreotide and pancreatic enzyme blockers are not helpful and are not used in treatment.
Supportive Care:
Supportive care helps your body recover and avoid complications.
- Most patients are admitted to the hospital and given fluids through an IV to prevent dehydration.
- Nutrition is carefully managed; some people may need to stop eating temporarily, while others may receive special feeding through a tube.
- Routine blood tests and imaging are performed to evaluate your condition.
- Rest, pain management, and regular observation are key during recovery.
Procedures:
Some people may need special procedures if a cause, such as a gallstone, is found or if their condition worsens.
For instance, a procedure called ERCP is used to remove gallstones blocking the bile ducts. It is only done if stones are confirmed or if there is no improvement after 24 hours. ERCP carries risks like infection, bleeding, or worsening pancreatitis, so it is not used routinely.7Kundumadam S, Fogel EL, Gromski MA. Gallstone pancreatitis: general clinical approach and the role of endoscopic retrograde cholangiopancreatography. Korean J Intern Med. 2021 Jan;36(1):25-31. doi: 10.3904/kjim.2020.537. Epub 2021 Jan 1. PMID: 33147903; PMCID: PMC7820643.
Surgery:
In severe cases with fluid around the pancreas, surgery is delayed until it is safer. It is only considered when absolutely necessary, especially in severe cases or complications.
- Minimally invasive surgery uses small cuts and special tools to remove dead tissue. It usually means a quicker recovery.
- Open surgery is done through a larger cut in your abdomen to clean out infected or damaged areas when the problem is more serious.
- Continuous drainage means placing tubes to slowly drain infected fluid from around your pancreas. This can be done without major surgery.
- Gallbladder removal via cholecystectomy is done in people with gallstone-related pancreatitis to prevent future attacks.8Jeffrey. (2025, April 22). Acute Pancreatitis: Practice Essentials, Background, Pathophysiology. Medscape.com; Medscape. https://emedicine.medscape.com/article/181364-overview
Acute vs. Chronic Pancreatitis
If you have acute pancreatitis, your pancreas suddenly becomes swollen and inflamed. You will likely feel sharp abdominal pain that starts quickly. Your symptoms emerge but usually get better with proper treatment.
If you have chronic pancreatitis, your pancreas is damaged over a long time. This can happen if you keep drinking heavily or have repeated attacks of acute pancreatitis. Your pancreas gets scarred and doesn’t work well anymore. Unlike acute pancreatitis, the damage in chronic pancreatitis can’t be treated or cured.
Conclusion
Acute pancreatitis refers to the sudden inflammation of the pancreas. Gallstones and drinking alcohol are the two major causes, alongside idiopathic acute pancreatitis. Symptoms include radiating abdominal pain, nausea, and vomiting. It can range from mild to severe. Acute pancreatitis symptoms start early but can be resolved with treatment. In severe cases, surgery is needed.
Refrences
- 1Roberts, S. E., Akbari, A., Thorne, K., Atkinson, M., & Evans, P. A. (2013). The incidence of acute pancreatitis: impact of social deprivation, alcohol consumption, seasonal and demographic factors. Alimentary Pharmacology & Therapeutics, 38(5), 539–548. https://doi.org/10.1111/apt.12408
- 2Bartel, M. (2024, March 4). Acute Pancreatitis. MSD Manual Consumer Version; MSD Manuals. https://www.msdmanuals.com/home/digestive-disorders/pancreatitis/acute-pancreatitis
- 3Acute pancreatitis. (2024). Patient.info. https://patient.info/digestive-health/gallstones-and-bile/acute-pancreatitis
- 4Lucocq, J., & Sanjay Pandanaboyana. (2024). Acute pancreatitis. Surgery (Oxford). https://doi.org/10.1016/j.mpsur.2024.10.005
- 5Gapp, J., Tariq, A., & Chandra, S. (2023, February 9). Acute Pancreatitis. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK482468/
- 6Szatmary, P., Grammatikopoulos, T., Cai, W., Huang, W., Mukherjee, R., Halloran, C., Beyer, G., & Sutton, R. (2022). Acute Pancreatitis: Diagnosis and Treatment. Drugs, 82(12), 1251–1276. https://doi.org/10.1007/s40265-022-01766-4
- 7Kundumadam S, Fogel EL, Gromski MA. Gallstone pancreatitis: general clinical approach and the role of endoscopic retrograde cholangiopancreatography. Korean J Intern Med. 2021 Jan;36(1):25-31. doi: 10.3904/kjim.2020.537. Epub 2021 Jan 1. PMID: 33147903; PMCID: PMC7820643.
- 8Jeffrey. (2025, April 22). Acute Pancreatitis: Practice Essentials, Background, Pathophysiology. Medscape.com; Medscape. https://emedicine.medscape.com/article/181364-overview