Acute pyelonephritis is a serious bacterial infection of the kidneys that leads to renal inflammation and is one of the most common kidney disorders. It typically arises as a complication of an ascending urinary tract infection (UTI), where bacteria travel from the bladder to the kidneys. Less commonly, the infection may spread through the bloodstream, particularly in immunocompromised individuals.
The condition is characterized by symptoms such as fever, flank pain, chills, nausea, vomiting, and urinary symptoms like frequency, urgency, and dysuria. If left untreated, acute pyelonephritis can lead to complications such as kidney abscess, sepsis, or chronic kidney damage.1Belyayeva M, Leslie SW, Jeong JM. Acute Pyelonephritis. 2024 Feb 28. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan–. PMID: 30137822.
How Common is Acute Pyelonephritis?
The incidence of acute pyelonephritis varies by gender. It occurs at a rate of 3 to 4 cases per 10,000 males annually, compared to 15 to 17 cases per 10,000 females. Women are more frequently affected due to anatomical factors, such as a shorter urethra, which predisposes them to UTIs. Pregnant women are particularly vulnerable due to hormonal changes and urinary stasis. In contrast, men with acute pyelonephritis often experience higher mortality rates, likely due to delayed diagnosis or associated comorbidities.
In the United States, approximately 250,000 cases are reported annually, making it a significant healthcare concern. Early diagnosis and treatment with antibiotics are critical to prevent severe complications and reduce mortality.2Belyayeva, M., Leslie, S. W., & Jeong, J. M. (2024). Acute pyelonephritis. In StatPearls [Internet]. StatPearls Publishing.
Pathophysiology
Kidneys make urine to dispose off waste. This urine travels through the ureters and then gathers in the bladder. It moves toward the urethra from the bladder to leave your body. This process washes out microbes, other germs, and bacteria from your body naturally.
But sometimes, bacteria move upward. They then infect parts of the tract, such as the urethra, ureters, and bladder. These bacteria can move into the kidneys (one or both) and cause a kidney infection.
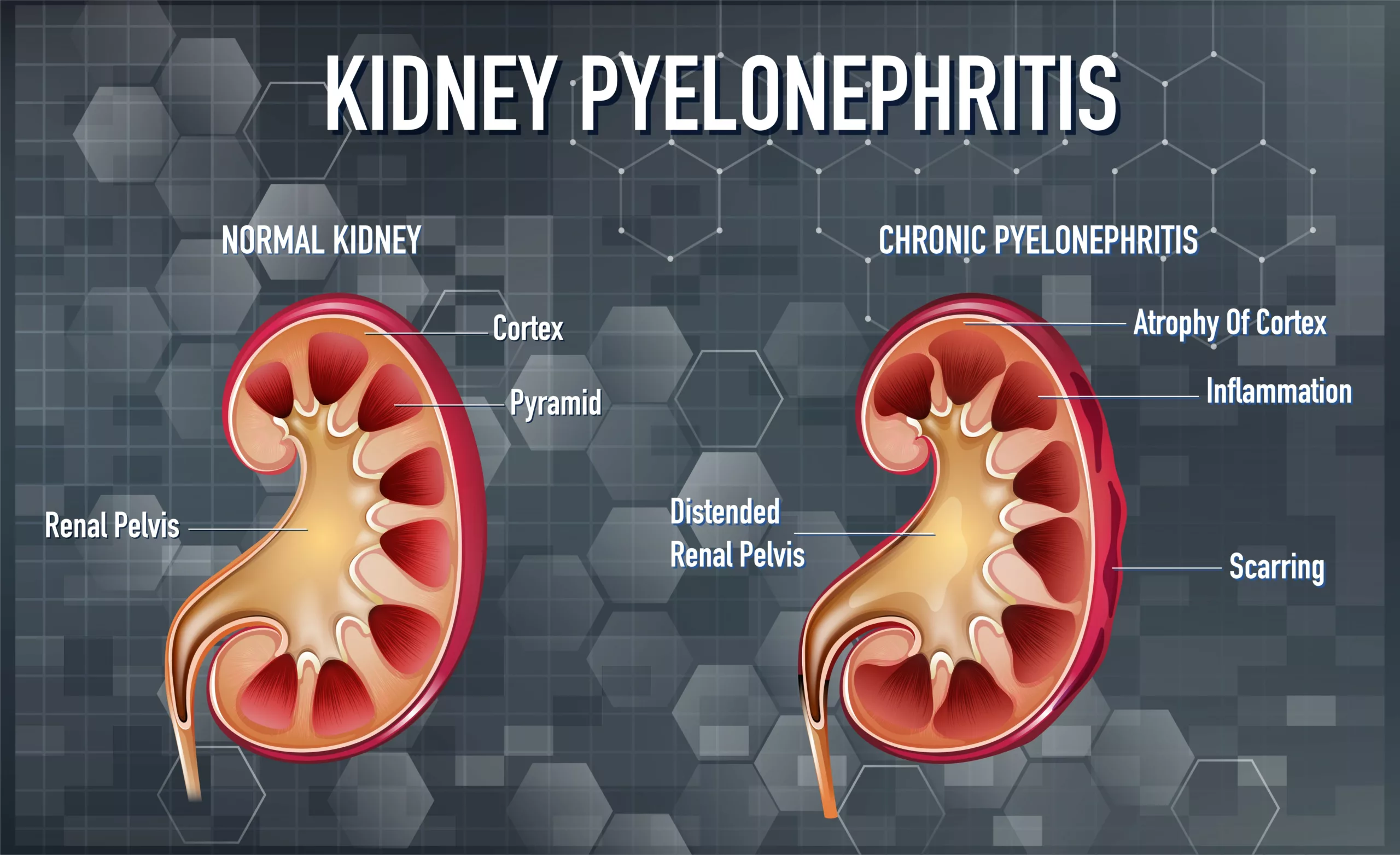
The infected kidneys make an acute response and release chemokines. Some other inflammatory factors are also released. This release results in damage to the renal parenchyma. This process may lead to complete renal involvement, known as pyelonephritis.3de Dios Ruiz-Rosado, J., Robledo-Avila, F., Cortado, H., Rangel-Moreno, J., Justice, S. S., Yang, C., … & Partida-Sanchez, S. (2021). Neutrophil-macrophage imbalance drives the development of renal scarring during experimental pyelonephritis. Journal of the American Society of Nephrology, 32(1), 69-85.
Symptoms & Signs of Acute Pyelonephritis
TAcute pyelonephritis typically presents with symptoms that develop rapidly within 1-2 days of infection onset. The severity and range of symptoms can vary but generally include the following:
- Pain: Flank or back pain, often localized to one side of the abdomen, is a hallmark symptom. Abdominal pain may also occur.
- Fever: High fever, usually exceeding 102°F (38.9°C), often accompanied by chills or shaking.
- Urinary Symptoms: Painful or burning urination (dysuria), cloudy or foul-smelling urine (sometimes fishy-smelling), blood or pus in the urine (hematuria or pyuria), and increased urinary frequency.
- Systemic Symptoms: Fatigue, general body aches, and nausea or vomiting, often due to the body’s systemic response to infection.
Other symptoms of acute pyelonephritis include:
- Nausea
- Chills or shaking
- General aching
- Vomiting
- Fatigue
- Mental confusion
Symptoms are different in older adults and children than in other people. Mental confusion is the most common symptom among older adults. In children, symptoms may include fever, irritability, and poor feeding, often associated with vesicoureteral reflux (VUR) or congenital urinary tract abnormalities.
Chronic pyelonephritis, on the other hand, often presents with milder or absent symptoms and is characterized by recurrent infections, kidney scarring, and progressive damage. If left untreated, it can lead to long-term complications such as renal dysfunction.4BMJ Best Practice. (n.d.). Pyelonephritis. Retrieved from https://bestpractice.bmj.com/topics/en-us/551#:~:text=Summary,confirm%20the%20diagnosis%20of%20pyelonephritis.
Causes of Acute Pyelonephritis
Acute pyelonephritis typically arises from an ascending bacterial infection. Bacteria enter the body through the urethra, multiply in the bladder, and then travel via the ureters to the kidneys.
Common Pathways of Infection
- Ascending Infection: This is the primary cause of pyelonephritis. The bacteria, often originating in the gastrointestinal tract, enter the urethra and bladder and ascend to the kidneys.5Flores-Mireles, A. L., Walker, J. N., Caparon, M., & Hultgren, S. J. (2015). Urinary tract infections: epidemiology, mechanisms of infection and treatment options. Nature Reviews Microbiology, 13(5), 269-284.
- Hematogenous Spread: Although uncommon, bacteria can reach the kidneys through the bloodstream, particularly in individuals with ureteral obstructions or weakened immune systems.
Predisposing Factors
- Gender and Anatomy: Women are more susceptible due to a shorter urethra, hormonal changes, and the urethra’s proximity to the anus.
- Urinary Obstruction: Conditions like kidney stones can block urinary flow, leading to pyonephrosis, a severe and potentially life-threatening form of obstructive pyelonephritis.
- Incomplete Bladder Emptying: This can result from urinary tract obstructions, allowing bacteria to multiply.
- Renal Transplantation: Transplant patients are at higher risk due to immunosuppression and abnormal kidney anatomy, especially during the first six months post-transplant.
- Vesicoureteral Reflux (VUR): This congenital condition causes urine to flow backward from the bladder into the kidneys during urination.6Banker, H., & Aeddula, N. R. (2022). Vesicoureteral reflux. In StatPearls [Internet]. StatPearls Publishing.
Other Contributing Factors:
- Recent urinary tract surgery
- Use of urinary catheters
- Nerve or spinal cord damage affecting bladder control
- Certain medications that suppress immune function
Causative Organisms
Escherichia coli (E. coli) is the most common cause of urinary tract infections and subsequent pyelonephritis.7Bono, M. J., Leslie, S. W., & Reygaert, W. C. (2017). Uncomplicated urinary tract infections. Other bacterial species that may cause pyelonephritis include:
- Proteus
- Enterococcus
- Pseudomonas
- Enterobacteria
- Staphylococcus
Acute Pyelonephritis in Pregnancy
Pregnancy causes various physiological and anatomical changes in the bodies of women. These also include physiological changes in the urinary tract. One of the significant factors involved in these changes is hormones.
Hormones, commonly progesterone levels, increase during pregnancy. This increase leads to the relaxation of the smooth muscles of the tract, ureters, and bladder. Relaxation of the muscles reduces ureteral tone. It also alters the dynamics of the bladder. This process allows the ascent of bacteria from the urethra to the bladder. Eventually, the kidneys become infected.
The changes in the immune system during pregnancy impair the body’s capabilities. The body becomes unable to combat bacterial infections. These factors create a conducive environment for the development of UTIs during pregnancy.
This highlights the significance of proactive measures to manage and prevent these infections. Acute pyelonephritis during pregnancy requires admission to the hospital. It can threaten the lives of both the baby and the mother. Additionally, it increases the risk of premature baby deliveries. Treatment includes beta-lactam for about 24 hours until the symptoms get better. Preventive measures are a urine culture between the 12th and 16th weeks of pregnancy.8Silverman, M. D., & Turrentine, M. A. (2023). Urinary Tract Infections in Pregnant Individuals.
Diagnosis
The diagnosis of acute pyelonephritis is through physical examination and medical history. But, laboratory checks and imaging tests can be more helpful.
Clinical Examination:
The physical examination assesses the signs of infection, including:
- Abdominal tenderness
- Rapid breathing rate
- Rapid heart rate
- High blood pressure
Doctors review patients’ medical history. It includes underlying medical conditions, a history of UTIs, and kidney stones.
Laboratory Tests:
Blood Culture
This detects bacteria present in the bloodstream. It can help identify the causative agent.
Complete Blood Count (CBC)
CBC evaluates the signs of infection. These signs include:
- An elevated white blood cell count and an elevated eosinophil count.
- Blood urea nitrogen and creatinine levels are usually measured. These levels assess kidney function and determine kidney disease.
Urinalysis
Urinalysis involves analyzing a clean-catch urine sample or using a urethral catheter in children to identify pyuria, which is the most common finding in acute pyelonephritis. The presence of leukocyte esterase and nitrites in the urine suggests bacterial infection, particularly from urease-producing bacteria, while protein or blood in the urine indicates inflammation or infection. A urine culture is also performed to confirm the presence of specific bacteria and guide antibiotic therapy.
Imaging Tests:
Imaging tests are only considered for high-risk patients. High-risk patients include:
- Septic patients
- Patients with weak immunity
- People with a single kidney
- Worsening renal function
- Surgically corrected urinary tract anomalies
- People with diabetes
- People with urolithiasis
- Fever
- People with AIDS
- Patients are unresponsive to treatment
Ultrasonography
Ultrasonography helps in assessing pyelonephritis. It looks for:
- Tumors
- Cysts
- Enlargement of the kidney and ureter
- Kidney stones
- Other kinds of obstruction in the urinary tract.
Magnetic Resonance Imaging (MRI)
When ultrasound is insufficient to detect pyelonephritis, MRI is utilized. MRI with intravenous contrast evaluates:
- Kidneys and surrounding tissues for edema and inflammation
- Fluid or abscesses
- Structural abnormalities
- Kidney stones
Computed Tomography (CT) Scan
A CT scan indicates high-risk patients. A CT scan with intravenous contrast for the evaluation of the kidneys for:
- Focal wedge-shaped defects
- Inflammation
- Edema
- Stones
- Enlargement
- Structural abnormalities
Radioactive Images
A dimercaptosuccinic acid (DMSA) test is for scarring of the kidneys in pyelonephritis. It tracks an injection of radioactive substances. Healthcare professionals inject the material into the vein of the arm. This material travels to the kidneys.
Images show a scarred and infected area. The radioactive material travels through the kidney.9Belyayeva, M., Leslie, S. W., & Jeong, J. M. (2024). Acute pyelonephritis. In StatPearls [Internet]. StatPearls Publishing.
Cystoscopy & Renal Scintigraphy
Cystoscopy visualizes the urethra and bladder to find underlying structural abnormalities. Renal scintigraphy is a nuclear medicine test. It detects functional abnormalities in kidney function.
Management & Treatment of Acute Pyelonephritis
Antipyretics, analgesics, and antibiotics are the mainstays of treatment for acute pyelonephritis. The selection of antibiotics is empiric in the initial stages. Antibiotic therapy is customizable on the basis of urinalysis and culture results.
Antibiotics:
In most cases, the causative agent is E.coli. Treatment is with oral sulfamethoxazole-trimethoprim or cephalosporins for 14 days. They are also advised to take fluoroquinolone for 7 days.10Lee, R. A., Centor, R. M., Humphrey, L. L., Jokela, J. A., Andrews, R., Qaseem, A., & Scientific Medical Policy Committee of the American College of Physicians*. (2021).
Empiric Antibiotics for Acute Pyelonephritis
These antibiotics include:
- Fluoroquinolone for seven days
- Cefpodoxime (200 mg) for 7-10 days (twice a day)
- Amoxicillin-clavulanate (875 mg) for 7 to 10 days (twice a day)
- Sulfamethoxazole-trimethoprim for about 14 days
- Cefadroxil (1 g) for 7-14 days (twice a day)
Antibiotics Recommended During Pregnancy
These antibiotics include:
- Cefepime
- Gentamicin
- Ceftriaxone
- Aztreonam
- Ampicillin11Silverman, M. D., & Turrentine, M. A. (2023). Urinary Tract Infections in Pregnant Individuals.
Pain Management:
Nonsteroidal anti-inflammatory drugs work efficiently for managing pain and fever in acute pyelonephritis.
Hospital Admission:
In case of ineffective drug therapy, the patient needs admission to the hospital. The length of stay in the hospital depends on the severity of the condition and your response to the treatment. The treatment will include:
- Antibiotics and intravenous hydration for 24 to 48 hours.
- Doctors track your urine and blood to trace the infection.
Surgical Management:
Upon recurrent kidney infections, surgery removes the obstruction. Surgery also corrects the structural problems of the kidneys. Surgery will also drain the abscess that is not responding to the given antibiotics.
Nephrectomy is for severe infection. Nephrectomy involves the removal of a part of the kidney.
Potential Complications
Acute pyelonephritis can lead to more serious complications. Emphysematous pyelonephritis is one of the most severe complications. It arises from acute pyelonephritis 12Sherchan, R., & Hamill, R. (2024). Emphysematous Pyelonephritis. In StatPearls [Internet]. StatPearls Publishing. Some other complications include:
- Acute renal failure
- Renal abscess
- Renal vein thrombosis
- Papillary necrosis
- Renal atrophy
Prognosis
Management of the majority of the patients requires:
- Oral antibiotics
- Antipyretics
- Anti-inflammatories.
Uncomplicated pyelonephritis is not considered lethal or dangerous. Unless it has associations with other conditions. Despite improvements, there is still high mortality and morbidity.
Pregnant females suffering from acute pyelonephritis are at an increased risk of:
- Premature delivery
- Restricted intrauterine growth
- Acute respiratory distress syndrome
- Renal injury
- Sepsis
- Fetal death
The overall mortality rate reported in some studies is 10-20%. The increased mortality rate is often associated with the following:
- Age (more than 65 years)
- Renal failure
- Diabetes
- Intravascular coagulation
- Septic shock
- Long-term use of a catheter
- Male gender
Prevention of Acute Pyelonephritis
Acute pyelonephritis can be a severe disorder. As soon as you doubt that you have a UTI or pyelonephritis, immediately contact your doctor. This condition requires immediate medical attention.
Following are some prevention tips:
- Drink more water and fluids to increase urination. This will help in removing bacteria from the urethra.
- Wipe from back to front if water is not available.
- Urinate after intercourse to flush out bacteria.
- Avoid the use of products that can irritate the urethra
- Take a shower regularly
- Always change sweaty or wet undergarments. This will prevent bacteria from getting into your body.
Acute Cystitis versus Pyelonephritis
Cystitis refers to a lower urinary tract infection. It is also known as an infection of the urinary bladder. Cystitis begins with a bacterial infection in the urinary tract. Complicated and uncomplicated cystitis are the two types of cystitis.
Complicated cystitis has several risk factors. These include an increased likelihood of severe infection. Also, there is a chance of antibiotic therapy failure. Uncomplicated cystitis involves a lower UTI in either men or women.13Li, R., & Leslie, S. W. (2023). Cystitis. In StatPearls [Internet]. StatPearls Publishing.
Pyelonephritis occurs due to the inflammation of the upper urinary tract and includes:
- The ureters
- Renal pelvis
- Kidneys.
But cystitis arises due to inflammation in the lower urinary tract and includes:
- Urethra and bladder.
- Pyelonephritis is the most severe infection of cystitis due to inflammation.
- Cystitis is different from pyelonephritis due to the lack of some systemic findings.
These include chills, fever, and sepsis. Their methods of treatment vary due to the variable severity of the conditions.
Conclusion
Acute pyelonephritis is a serious condition. It needs immediate medical attention to prevent complications. A clear understanding of the condition will help you take proactive steps. These steps can reduce the risk of developing the condition.
Early use of antibiotics can also improve outcomes. Remember! With prompt recognition of the causes and symptoms, early intervention should be performed. With suitable management, even patients with severe conditions can have good outcomes.
Refrences
- 1Belyayeva M, Leslie SW, Jeong JM. Acute Pyelonephritis. 2024 Feb 28. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan–. PMID: 30137822.
- 2Belyayeva, M., Leslie, S. W., & Jeong, J. M. (2024). Acute pyelonephritis. In StatPearls [Internet]. StatPearls Publishing.
- 3de Dios Ruiz-Rosado, J., Robledo-Avila, F., Cortado, H., Rangel-Moreno, J., Justice, S. S., Yang, C., … & Partida-Sanchez, S. (2021). Neutrophil-macrophage imbalance drives the development of renal scarring during experimental pyelonephritis. Journal of the American Society of Nephrology, 32(1), 69-85.
- 4BMJ Best Practice. (n.d.). Pyelonephritis. Retrieved from https://bestpractice.bmj.com/topics/en-us/551#:~:text=Summary,confirm%20the%20diagnosis%20of%20pyelonephritis.
- 5Flores-Mireles, A. L., Walker, J. N., Caparon, M., & Hultgren, S. J. (2015). Urinary tract infections: epidemiology, mechanisms of infection and treatment options. Nature Reviews Microbiology, 13(5), 269-284.
- 6Banker, H., & Aeddula, N. R. (2022). Vesicoureteral reflux. In StatPearls [Internet]. StatPearls Publishing.
- 7Bono, M. J., Leslie, S. W., & Reygaert, W. C. (2017). Uncomplicated urinary tract infections.
- 8Silverman, M. D., & Turrentine, M. A. (2023). Urinary Tract Infections in Pregnant Individuals.
- 9Belyayeva, M., Leslie, S. W., & Jeong, J. M. (2024). Acute pyelonephritis. In StatPearls [Internet]. StatPearls Publishing.
- 10Lee, R. A., Centor, R. M., Humphrey, L. L., Jokela, J. A., Andrews, R., Qaseem, A., & Scientific Medical Policy Committee of the American College of Physicians*. (2021).
- 11Silverman, M. D., & Turrentine, M. A. (2023). Urinary Tract Infections in Pregnant Individuals.
- 12Sherchan, R., & Hamill, R. (2024). Emphysematous Pyelonephritis. In StatPearls [Internet]. StatPearls Publishing
- 13Li, R., & Leslie, S. W. (2023). Cystitis. In StatPearls [Internet]. StatPearls Publishing.

