What is Primary Pulmonary Hypertension?
Primary Pulmonary Hypertension is a rare and progressive condition characterized by high blood pressure in the pulmonary arteries that take blood with low oxygen from your heart to the lungs. It is also known as idiopathic pulmonary artery hypertension as it does not arise in the background of any disease. When the pressure in the pulmonary artery exceeds 25mmHg, the disease starts showing symptoms in your body, and it has dangerous consequences if not properly dealt with.1Anderson, J. J., & Lau, E. M. (2022). Pulmonary Hypertension Definition, Classification, and Epidemiology in Asia. JACC Asia, 2(5), 538-546. https://doi.org/10.1016/j.jacasi.2022.04.008
Clinically, it is defined as a syndrome of dyspnea, chest pain, and syncope caused by increased pulmonary vascular resistance without any known underlying cause. 2Archer S, Rich S. Primary Pulmonary Hypertension: A Vascular Biology and Translational Research “Work in Progress.” Originally published November 28, 2000. Circulation. 2000;102(22):2781–2791. https://doi.org/10.1161/01.CIR.102.22.2781
Incidence of Primary Pulmonary Hypertension
This condition is quite notorious for causing almost 150 deaths per year, as it has no definite cure. The US has nearly 2-5 cases per million per year. Females are more prone to suffer from this disease.3Johnson, C., Corris, P. A., Leary, P. J., Rich, S., Yacoub, M., & Roth, G. A. (2021). Prevalence, incidence, and survival of pulmonary arterial hypertension: A systematic review for the global burden of disease 2020 study. Pulmonary Circulation, 12(1). https://doi.org/10.1002/pul2.12020
Causes
There are no specific and evident causes of this condition. However, in patients having a family history of primary pulmonary hypertension, there is the presence of a defect in the gene BMPR-ll. Cases in which primary pulmonary hypertension occurs due to a genetic defect are very rare. The most recent NICE classification system signifies some other genes that may be involved in the pathogenesis of primary pulmonary hypertension. These are ALK1, ENG, SMAD9, CAV1 and KCK3. The defect in these genes severely impacts the transport of potassium ion channels in your body.
Some studies indicate that there might be a possibility of other factors in the pathophysiology of primary pulmonary hypertension, too. Any injury to your pulmonary system starts a series of actions in your body, like fibrosis, scarring, or thrombosis. This mechanism adversely affects the normal vasculature of your pulmonary artery by disrupting the normal blood flow. The abnormal blood flow increases the pressure in the artery, contributing to the development of this condition.
Although it doesn’t have any precise reason behind its cause, most of the people having PPH have a history of certain associated abnormalities like connective tissue disease, liver or lung problems, SLE, esophageal motility disorder, and exposure to some agents (cocaine, amphetamines).4Hoeper, M. M., Ghofrani, A., Grünig, E., Klose, H., Olschewski, H., & Rosenkranz, S. (2017). Pulmonary Hypertension. Deutsches ÄRzteblatt International, 114(5), 73-84. https://doi.org/10.3238/arztebl.2017.0073
Primary Vs. Secondary Pulmonary Hypertension
The word primary indicates that primary pulmonary hypertension is idiopathic, having no known cause behind its pathogenesis. Many studies show typical changes in pulmonary arteries, like fibrosis or thickening, causing abnormal blood flow and eventually leading to increased blood pressure. High blood pressure in the pulmonary artery also affects your right heart, causing right heart failure in many cases. In rare cases, PPH develops along with portal hypertension (high blood pressure in the portal vein that supplies your liver).
On the other hand, secondary pulmonary hypertension develops in the background of a specific disease associated with your heart, lungs, and vessels, as well as certain systemic and metabolic disorders. Lung diseases that become a cause of secondary pulmonary hypertension are mainly COPD, interstitial lung disease, or developmental lung diseases. Secondary pulmonary hypertension also develops in people having problems with their left heart, like systole or diastole dysfunction or any defect in the mitral or aortic valves. Conditions like DVT or the formation of a thrombus in your arteries also contribute to the pathogenesis of secondary pulmonary hypertension. Moreover, if you have any blood, systemic, or metabolic disorders like thyroid disease, you might have a risk of developing secondary pulmonary hypertension.
Symptoms of Primary Pulmonary Hypertension
Symptoms do not come up in the early stage of the disease. As the disease progresses, it exhibits its non-specific symptoms in your body. These are:
Dyspnea:
In the early stages, dyspnea (shortness of breath) occurs during exercise or strenuous work. The presence of dyspnea even at rest indicates the progression of primary pulmonary hypertension, and early consultation with a doctor may benefit you in treating it before any severe complications occur.
Fatigue and weakness:
Fatigue is a common complaint in patients with primary pulmonary hypertension. Because it affects the right heart, even a little work can make you tired and weak.
Syncope:
In primary pulmonary hypertension, you may feel a temporary loss of consciousness. This occurs when your body cannot autoregulate your blood pressure due to defective mechanisms. As a result, your brain doesn’t get proper blood flow, leading to syncope or presyncope (a feeling before the actual loss of consciousness).5Lai, C., Potoka, K. C., Champion, H. C., Mora, A. L., & Gladwin, M. T. (2014). Pulmonary Arterial Hypertension: The Clinical Syndrome. Circulation Research, 115(1), 115. https://doi.org/10.1161/CIRCRESAHA.115.301146
Signs of Primary Pulmonary Hypertension
For the proper diagnosis, your physician performs your complete cardiac examination to identify signs of disease. Following are some crucial signs present in patients with primary pulmonary hypertension:
Defect in second heart sound:
During your chest auscultation, your physician might hear a loud pulmonary component of the second heart sound in your second left intercostal space.
Presence of a Murmur:
Primary pulmonary hypertension eventually affects your right heart and causes the tricuspid valve (between the right atrium and right ventricle) to regurgitate. Due to this backflow of blood in the right atrium, your physician hears an abnormal sound (murmur) at the left parasternal border.
Jugular Venous Pulsations:
As the blood cannot pump properly in primary pulmonary hypertension, it may accumulate and cause the distension of the jugular vein. This distension results in visible pulsation in the neck, indicating the severity of the condition.
Third heart sound:
Along with the murmur due to tricuspid regurgitation, there is also a third heart sound, or right-sided S3 gallop, in primary pulmonary hypertension. The reason behind S3 is the failure of the right heart due to persistent hypertension.
Enlarged Liver:
PPH causes your liver to increase in size, and your physician diagnoses hepatomegaly during superficial and deep palpation of your abdomen.
Ascites and Edema:
Primary pulmonary hypertension causes the accumulation of unpumped blood in the right heart, leading to blood leakage in the tissues. This leakage causes ascites, which is the presence of fluid in the abdomen. Sometimes, pitting edema also occurs in the legs and sacral area.6Lehrman, S., Romano, P., Frishman, W., Rashid, A., Dobkin, J., & Reichel, J. (2002). Primary pulmonary hypertension and cor pulmonale. Cardiology in review, 10(5), 265–278. https://doi.org/10.1097/00045415-200209000-00003
Risk factors of Primary Pulmonary Hypertension
You have a higher possibility of developing primary pulmonary hypertension if you have the following risk factors:7Faqih, S. A., Noto-Kadou-Kaza, B., Abouamrane, L. M., Mtiou, N., El Khayat, S., Zamd, M., Medkouri, G., Benghanem, M. G., & Ramdani, B. (2016). Pulmonary hypertension: prevalence and risk factors. International journal of cardiology. Heart & vasculature, 11, 87–89. https://doi.org/10.1016/j.ijcha.2016.05.012
- Family history
- Age
- Obesity, along with obstructive sleep apnea
- Pregnancy
- High altitude
- Drugs and toxins (methamphetamines)
Diagnosis of Primary Pulmonary Hypertension
History and physical examination are essential steps in diagnosing any disease. These two steps make the disease easy for your physician to diagnose. After analyzing the specific findings of primary pulmonary hypertension by examination, the following investigations are used to confirm the diagnosis:
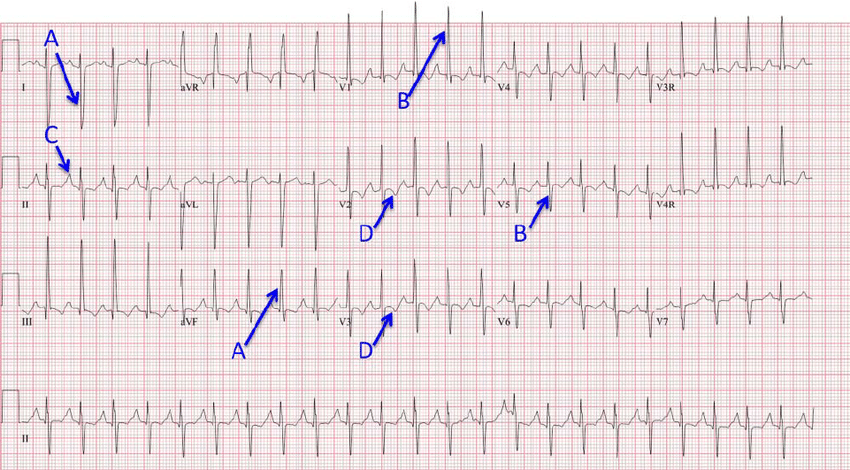
ECG:
ECG findings in primary pulmonary hypertension typically become evident when the right heart is involved. Common ECG abnormalities include right axis deviation, right ventricular hypertrophy, and signs of right atrial enlargement. ST depression and T-wave inversion may also be observed in the anterior leads. Although ECG can be a useful initial investigation, it is important to note that not all patients with primary pulmonary hypertension will exhibit these abnormalities.
Chest X-RAY
Symptoms of dyspnea, along with primary pulmonary hypertension, indicate lung involvement. In such cases, chest X-rays are a useful first-line investigation as they clearly show the enlargement of the right heart due to hypertension and the dilation of the pulmonary arteries.
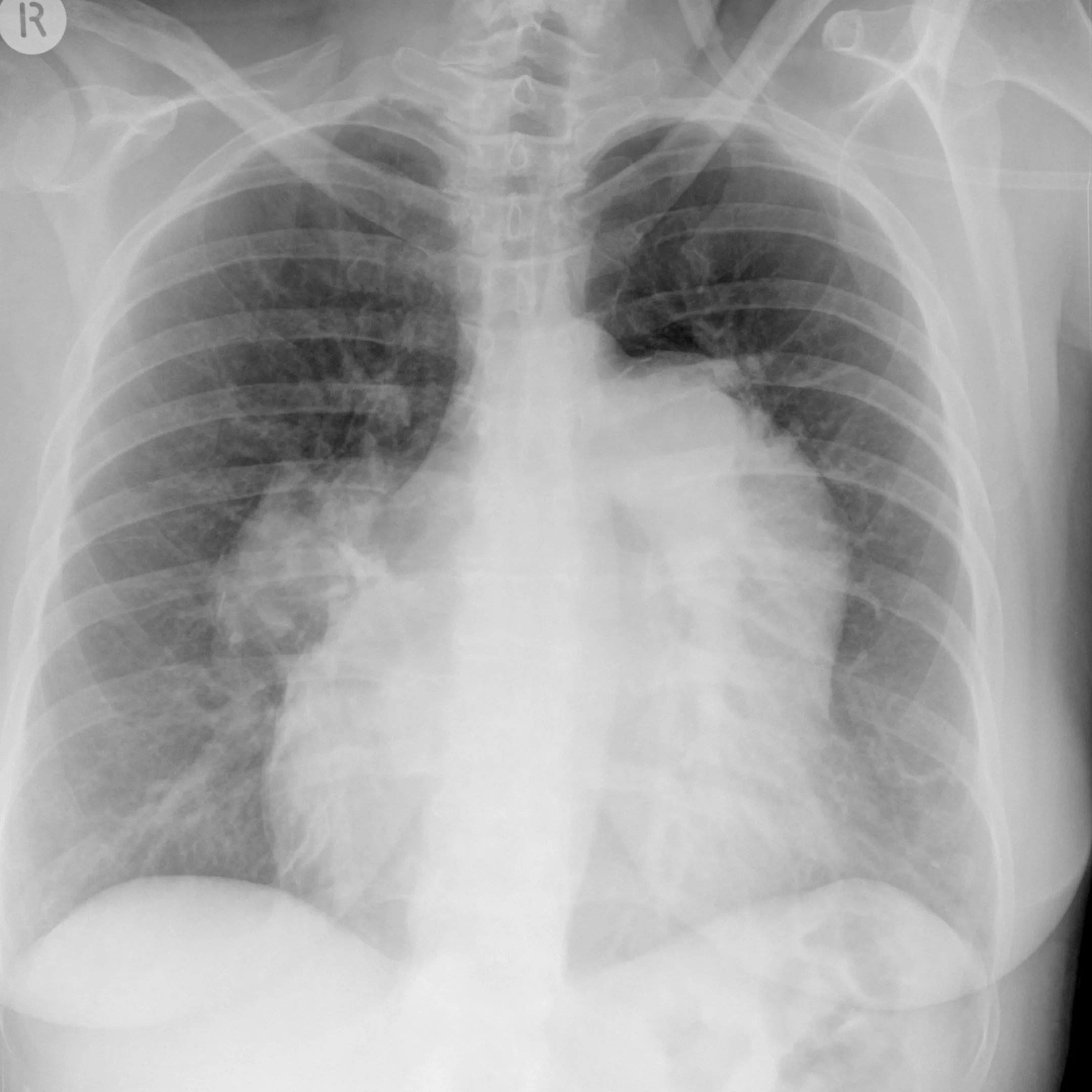
Case courtesy of Alexandra Stanislavsky, Radiopaedia.org. From the case rID: 12644
Echocardiography:
Echocardiography helps to diagnose primary pulmonary hypertension when there is suspicion of any contributing factor like left heart failure. It aids in showing right heart enlargement, valvular diseases, decreased right heart function, and flat interventricular septum (septum between two ventricles). If the echocardiography shows the presence of fluid in your pericardial cavity, there is a suspicion that this condition is getting severe.
Cardiac catheterization:
Cardiac catheterization is a valuable investigation in diagnosing primary pulmonary hypertension. The surgeon inserts a catheter into the pulmonary arterial circulation. This helps measure the pressure in the pulmonary artery and diagnose secondary causes of pulmonary hypertension. However, it is crucial to note that cardiac catheterization is contraindicated in patients with primary pulmonary hypertension who have left heart failure.

Laboratory tests:
Some laboratory tests, such as pulmonary function tests, the presence of antinuclear antibodies, and B-type natriuretic peptides, aid in diagnosing these diseases.
Thyroid tests:
Screening for the thyroid gland is done in patients with primary pulmonary hypertension. This is crucial because, in patients with hyperthyroidism, the pressure in the pulmonary artery increases.
Exercise testing:
Patients occasionally suffer from exercise intolerance due to the involvement of the lungs. To measure lung capacity, your physician performs a 6-minute walk test. In addition to exercise, pulmonary function tests are also carried out.8Anand, S., Sadek, A., Vaidya, A., & Oliveros, E. (2023). Diagnostic Evaluation of Pulmonary Hypertension: A Comprehensive Approach for Primary Care Physicians. Journal of Clinical Medicine, 12(23), 7309. https://doi.org/10.3390/jcm12237309
Treatment of Primary Pulmonary Hypertension
The main goal of treatment is to lower the pressure in the pulmonary artery. Physicians follow the following treatment:
Calcium Channel Blockers:
The mechanism of CCBs is to dilate the smooth muscles of arteries. In this way, they dilate the pulmonary artery, lower its resistance, and ultimately reduce its pressure. When used for a longer period, they are very effective in treating primary pulmonary hypertension. However, calcium channel blockers must not be used in patients with right heart failure as they worsen the function of the right heart.
Specific Therapy:
Some drugs are specifically used for this condition and have also proven to be very effective. These are:
Prostacyclins Analogs
These include Epoprostenol, Treprostinil (subcutaneous, intravenous, inhaled, and extended-release oral tablets), Iloprost (inhaled), and Selexipag (oral).
Endothelin Receptor Antagonists
These are Bosentan, Ambrisentan, and Macitentan (used for adults).
Oral Phosphodiesterase Type-5 Inhibitor
These include Sildenafil and Tadalafil.
Gunalyate Cyclase Stimulator
Riocigiuat is orally used for adults.
Combination therapy of these specific medications is more effective than monotherapy. The most widely used combination is Ambrisentan with tadalafil, which helps reduce the symptoms by 50%.9Rose-Jones, L. J., & Mclaughlin, V. V. (2015). Pulmonary hypertension: types and treatments. Current cardiology reviews, 11(1), 73–79. https://doi.org/10.2174/1573403×09666131117164122
Ancillary Treatment:
Ancillary treatment gives good results in patients with this condition. It includes:
Anticoagulation
Anticoagulants like warfarin significantly reduce the clinical symptoms of primary pulmonary hypertension.
Diuretics
This condition causes fluid to leak into the tissues, leading to edema. Loop diuretics like furosemide have been proven effective in treating peripheral edema.
Oxygen
The initial symptom you may face is shortness of breath, and oxygen therapy helps resolve it.

Digoxin
In patients having right heart failure due to primary pulmonary hypertension, the physician prescribes the digoxin tablet to improve the functional capacity of the right heart.
Diet & activity:
A diet low in sodium and fluid is recommended in patients with primary pulmonary hypertension, as sodium exacerbates the symptoms of fluid overload. It would be best if you avoided strenuous work and exercise. However, a little activity might help to lessen the severity of symptoms.
Transplantation & Septoplasty:
The indication of lung transplant in patients with this condition is the deterioration of symptoms even with the use of medicines. On the other hand, Atrial septostomy is a surgical procedure in which a hole is created in the atrial septum (the wall between the right and left atria of the heart) to relieve right heart pressure and improve cardiac output in patients with severe PAH. This procedure is usually considered in selective patients with refractory symptoms despite optimal medical therapy and who are not candidates for lung transplantation. Atrial septostomy can improve symptoms and quality of life in some patients, but it is associated with significant risks and should be performed by experienced cardiologists or cardiac surgeons.10Schwab, K. E., MD. (n.d.). Pulmonary Arterial Hypertension Treatment & management: approach considerations, oxygen supplementation, preventive care. https://emedicine.medscape.com/article/303098-treatment
Complications of Primary Pulmonary Hypertension
Complications that you may experience are:11Mak, S. M., Strickland, N., & Gopalan, D. (2017). Complications of pulmonary hypertension: a pictorial review. The British journal of radiology, 90(1070), 20160745. https://doi.org/10.1259/bjr.20160745
- Right heart enlargement and failure
- Massive pulmonary artery dilatation
- Myocardial infarction
- Asthma-like symptoms
- Pulmonary artery dissection
- Alveolar hemorrhage due to long-term use of anticoagulants
- Pericardial effusion
- Congestive hepatopathy (cirrhosis)
Prognosis of Primary Pulmonary Hypertension
For people with untreated primary pulmonary hypertension, the survival rate is very poor. From the day of diagnosis of the disease, patients can only live up to 3 years. However, the medical therapy specific to this condition, like prostacyclin analogs, greatly improves your symptoms.12Turina, J., Wirz, P., & Krayenbühl, H. P. (1977). Verlauf und Prognose der primären pulmonalen Hypertonie [Course and prognosis of primary pulmonary hypertension]. Schweizerische medizinische Wochenschrift, 107(49), 1825–1828.
Conclusion
In conclusion, it is a quite common disease with a poor prognosis. It is idiopathic as it doesn’t have any specific factor behind its cause. Primary pulmonary hypertension ultimately leads to right heart failure, edema, and liver cirrhosis. Echocardiography, chest x-rays, and cardiac catheterization help to diagnose it. Initially, take medical treatments like calcium channel blockers, prostacyclin analogs, and anticoagulants, as they aid in decreasing the severity of your symptoms. It is better to start the treatment as soon as possible to avoid complications like pulmonary dilatation, pulmonary artery dissection, and myocardial infarction.
Refrences
- 1Anderson, J. J., & Lau, E. M. (2022). Pulmonary Hypertension Definition, Classification, and Epidemiology in Asia. JACC Asia, 2(5), 538-546. https://doi.org/10.1016/j.jacasi.2022.04.008
- 2Archer S, Rich S. Primary Pulmonary Hypertension: A Vascular Biology and Translational Research “Work in Progress.” Originally published November 28, 2000. Circulation. 2000;102(22):2781–2791. https://doi.org/10.1161/01.CIR.102.22.2781
- 3Johnson, C., Corris, P. A., Leary, P. J., Rich, S., Yacoub, M., & Roth, G. A. (2021). Prevalence, incidence, and survival of pulmonary arterial hypertension: A systematic review for the global burden of disease 2020 study. Pulmonary Circulation, 12(1). https://doi.org/10.1002/pul2.12020
- 4Hoeper, M. M., Ghofrani, A., Grünig, E., Klose, H., Olschewski, H., & Rosenkranz, S. (2017). Pulmonary Hypertension. Deutsches ÄRzteblatt International, 114(5), 73-84. https://doi.org/10.3238/arztebl.2017.0073
- 5Lai, C., Potoka, K. C., Champion, H. C., Mora, A. L., & Gladwin, M. T. (2014). Pulmonary Arterial Hypertension: The Clinical Syndrome. Circulation Research, 115(1), 115. https://doi.org/10.1161/CIRCRESAHA.115.301146
- 6Lehrman, S., Romano, P., Frishman, W., Rashid, A., Dobkin, J., & Reichel, J. (2002). Primary pulmonary hypertension and cor pulmonale. Cardiology in review, 10(5), 265–278. https://doi.org/10.1097/00045415-200209000-00003
- 7Faqih, S. A., Noto-Kadou-Kaza, B., Abouamrane, L. M., Mtiou, N., El Khayat, S., Zamd, M., Medkouri, G., Benghanem, M. G., & Ramdani, B. (2016). Pulmonary hypertension: prevalence and risk factors. International journal of cardiology. Heart & vasculature, 11, 87–89. https://doi.org/10.1016/j.ijcha.2016.05.012
- 8Anand, S., Sadek, A., Vaidya, A., & Oliveros, E. (2023). Diagnostic Evaluation of Pulmonary Hypertension: A Comprehensive Approach for Primary Care Physicians. Journal of Clinical Medicine, 12(23), 7309. https://doi.org/10.3390/jcm12237309
- 9Rose-Jones, L. J., & Mclaughlin, V. V. (2015). Pulmonary hypertension: types and treatments. Current cardiology reviews, 11(1), 73–79. https://doi.org/10.2174/1573403×09666131117164122
- 10Schwab, K. E., MD. (n.d.). Pulmonary Arterial Hypertension Treatment & management: approach considerations, oxygen supplementation, preventive care. https://emedicine.medscape.com/article/303098-treatment
- 11Mak, S. M., Strickland, N., & Gopalan, D. (2017). Complications of pulmonary hypertension: a pictorial review. The British journal of radiology, 90(1070), 20160745. https://doi.org/10.1259/bjr.20160745
- 12Turina, J., Wirz, P., & Krayenbühl, H. P. (1977). Verlauf und Prognose der primären pulmonalen Hypertonie [Course and prognosis of primary pulmonary hypertension]. Schweizerische medizinische Wochenschrift, 107(49), 1825–1828.

